Quick Reference for Personality Disorders
| Poor Prognosis | Good Prognosis |
|---|---|
| Parental brutality/incest (Stone 1990) | High IQ (McGlashan 1985; Stone 1990) |
| Greater affective instability (McGlashan 1992) | Absence of narcissistic entitlement (Plakun 1991) |
| Magical thinking (McGlashan 1992) | Absence of parental divorce (Plakun 1991) |
| Impulsivity and substance abuse (Links et al. 1993) | |
| Comorbid schizotypal, antisocial, or paranoid features (Links et al. 1998; McGlashan 1986; Stone 1993) | |
| Presence of maternal psychopathology (Paris et al. 1988) | |
| Family history of mental illness (Paris et al. 1988) |
| Affective-Dysregulation | Impulsive-Behavioral | Cognitive-Perceptual |
|---|---|---|
| SSRI | SSRI | Low-dose antipsychotic |
| Low-dose antipsychotic | Low-dose antipsychotic | SSRI |
| Clonazepama | Lithium carbonate | |
| MAOIb | MAOIb | |
| Lithium | Carbamazepine | |
| Divalproex | ||
| Naltrexonec |
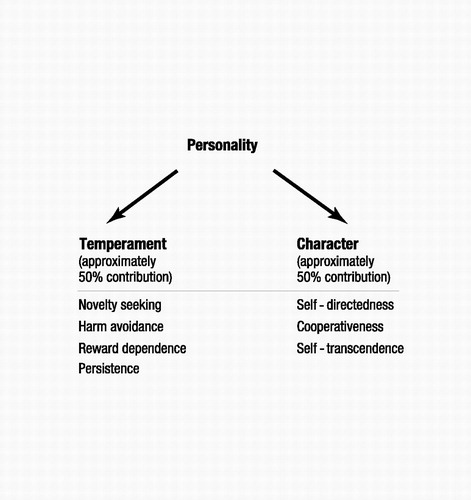
Figure 1. A Psychobiological Model of Personality Disorder
Source:Gabbard GO: Psychodynamic Psychiatry in Clinical Practice, 4th ed. Washington, DC, American Psychiatric Publishing, 2005, p. 443 (based on Cloninger et al., 1993)
| Need for admiration and affirmation from the therapist |
| Idealization of the therapist |
| Assumption of twinship between therapist and patient |
| Proneness to feel shamed and humiliated by the therapist |
| Contempt and devaluation toward the therapist, often related to envy |
| Denial of the therapist’s autonomy |
| Omnipotent control of the therapist |
| Insistence on exclusive dyadic relatedness that does not allow for a third party |
| Use of the therapist as a sounding board without empathy for the therapist’s experience |
| Denial of dependency on the therapist |
| Inability to accept help from the therapist |
| Cluster | Type | Characteristic Features |
|---|---|---|
| A | Odd or eccentric | |
| Paranoid | Pervasive distrust and suspiciousness of others such that their motives are interpreted as malevolent | |
| Schizoid | Pervasive pattern of detachment from social relationships and restricted range of expression of emotions in interpersonal settings | |
| Schizotypal | Pervasive pattern of social and interpersonal deficits marked by acute discomfort with, and reduced capacity for, close relationships as well as by cognitive or perceptual distortions and eccentricities of behavior | |
| B | Dramatic, emotional, or erratic | |
| Antisocial | History of conduct disorder before age 15; pervasive pattern of disregard for and violation of the rights of others; current age at least 18 | |
| Borderline | Pervasive pattern of instability of interpersonal relationships, self-image, and affects, and marked impulsivity | |
| Histrionic | Pervasive pattern of excessive emotionality and attention seeking | |
| Narcissistic | Pervasive pattern of grandiosity (in fantasy or behavior), need for admiration, and lack of empathy | |
| C | Anxious or fearful | |
| Avoidant | Pervasive pattern of social inhibition, feelings of inadequacy, and hypersensitivity to negative evaluation | |
| Dependent | Pervasive and excessive need to be taken care of that leads to submissive and clinging behavior and fears of separation | |
| Obsessive-compulsive | Pervasive pattern of preoccupation with orderliness, perfectionism, and mental and interpersonal control at the expense of flexibility, openness, and efficiency |
| I. | Mindfulness | ||||||||||||||||||||||||
| |||||||||||||||||||||||||
| II. | Distress tolerance | ||||||||||||||||||||||||
| |||||||||||||||||||||||||
| III. | Emotion regulation | ||||||||||||||||||||||||
| |||||||||||||||||||||||||
| IV. | Interpersonal effectiveness | ||||||||||||||||||||||||
| |||||||||||||||||||||||||
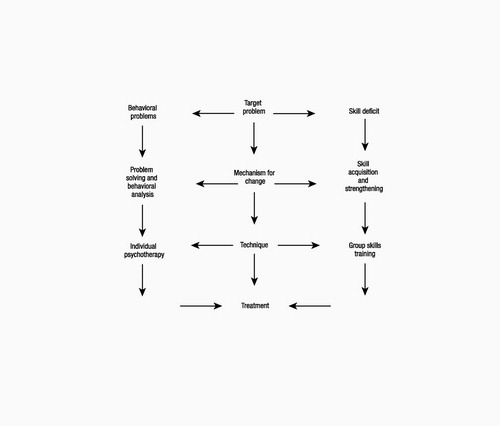
Figure 2. Dialectical Behavior Therapy: Two-Pronged Approach
Source:Stanley B, Brodsky BS: Dialectical behavior therapy, in The American Psychiatric Publishing Textbook of Personality Disorders. Edited by Oldham JO, Skodol AE, Bender DS. Washington, DC, American Psychiatric Publishing, 2005, chapter 19, p. 311
Cloninger CR, Srvakic DM, Pryzbeck TR: A psychobiological model of temperament and character. Arch Gen Psychiatry 1993; 50:975–990Crossref, Google Scholar
Gabbard GO: Combining medication with psychotherapy in the treatment of borderline personality disorder, in Psychotherapy and Personality Disorders (Review of Psychiatry Series; Oldham JM and Riba MB, series eds.), vol 19. Edited by Gunderson JG, Gabbard GO. Washington, DC, American Psychiatric Press, 2000, pp 65–90Google Scholar
Links PS, Heslegrave R, vanReekum R: Prospective follow-up study of borderline personality disorder: prognosis, prediction of outcome, and axis II comorbidity. Can J Psychiatry 1998; 43:265–270Crossref, Google Scholar
Links PS, Mitton JE, Steiner M: Stability of borderline personality disorder. Can J Psychiatry 1993; 38:255–259Crossref, Google Scholar
McGlashan TH: Prediction of outcome in BPD, in The Borderline: Current Empirical Research. Edited by McGlashan TH. Washington, DC, American Psychiatric Press, 1985, pp 61–98Google Scholar
McGlashan TH: The Chestnut Lodge Follow-up Study, III: long-term outcome of borderline personalities. Arch Gen Psychiatry 1986; 43:20–30Crossref, Google Scholar
McGlashan TH: The longitudinal profile of BPD: contributions from the Chestnut Lodge Follow-up Study, in Handbook of the Borderline Diagnosis. Edited by Silver D, Rosenbluth M. Madison, CT, International Universities Press, 1992Google Scholar
Paris J, Nowlis D, Brown R: Developmental factors in the outcome of borderline personality disorder. Compr Psychiatry 1988; 29:147–150Crossref, Google Scholar
Plakun EM: Prediction of outcome in borderline personality disorder. J Personal Disord 1991; 5:93–101Crossref, Google Scholar
Soloff PH: Algorithms for pharmacological treatment of personality dimensions: symptom-specific treatments for cognitive-perceptual, affective, and impulse-behavioral dysregulation. Bull Menninger Clin 1998; 62:195–214Google Scholar
Stone MH: Long-term outcome in personality disorders. Br J Psychiatry 1993; 162:299–313Crossref, Google Scholar
Stone MH: The Fate of Borderline Patients: Successful Outcome and Psychiatric Practice. New York, Guilford, 1990Google Scholar



