Assessment of Panic Disorder Across the Life Span
Abstract
Panic disorder is a relatively common anxiety disorder that is often disabling. It may or may not be associated with agoraphobia. Panic disorder can be imitated by various medical illnesses, which, even when treated, can get cued with panic symptoms. It is also frequently comorbid with other psychiatric disorders including depression, generalized anxiety disorder, and substance use disorders. Although often initially seen in early adulthood, panic disorder can also present in childhood or in the geriatric population. Clinicians should thus be aware of the variability in clinical presentations that may be associated with both the pediatric and geriatric age groups. This article provides a broad overview of various screening and assessment tools used to evaluate panic disorder across the lifespan. The article also highlights some of the developmental differences and variability in the clinical presentation of pediatric and geriatric panic disorder.
Panic disorder is a common psychiatric disorder that affects up to 5% of the population at some point in their lifetime (1). The essential features of panic disorder include recurrent, often unexpected, panic attacks followed by at least 1 month of persistent concern about having another panic attack, worry about the possible implications or consequences of the panic attacks, or a significant behavioral change related to the attacks (2). Panic attacks are discrete episodes associated with an intense fear or discomfort and accompanied by at least 4 of the 13 somatic or cognitive symptoms listed in the DSM-IV-TR: accelerated heart rate, shortness of breath, chest pain, choking sensations, hot/cold flashes, sweating, trembling, nausea, depersonalization/derealization, fear of dying, fear of going crazy, and fear of losing control (Table 1) (3). Panic attacks usually have an abrupt onset and last from 10 to 45 minutes (4). Many times, these may result in behavioral modifications in daily routine. Although panic attacks can occur in associated anxiety disorders including phobias and social anxiety disorder, panic attacks associated with panic disorder are unique as they occur spontaneously without an environmental trigger. Panic disorder may be associated with agoraphobia if the individual avoids places or situations from which escape may be difficult (5).
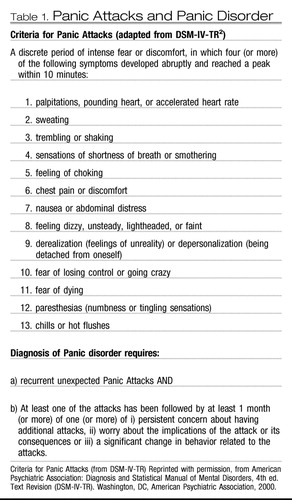 |
Table 1. Panic Attacks and Panic Disorder
Panic disorder must be distinguished from various psychiatric disorders and physical conditions that can have associated panic symptoms. Some of these conditions include other anxiety disorders (including specific phobias and posttraumatic stress disorder), substance use disorders (including stimulant abuse or withdrawal from sedative agents), or medical conditions, including hyperthyroidism (6). Furthermore, the clinical presentation of panic disorder may vary depending on the age of presentation and may make it difficult for the clinician to assess and ascertain the significance of such symptoms (7). This article focuses on the distinct diagnostic dilemmas and assessment tools used in the evaluation of panic disorder across the lifespan. A discussion of treatment approaches for panic disorder is beyond the scope of this article, and the reader is referred elsewhere for such a discussion (8). The paucity of literature on this subject in both extremes of ages further limits the evidence base in these age groups. As a result, there are a few instances in this article where the author has to refer to a more general term, “anxiety disorder,” instead of panic disorder specifically.
ASSESSMENT IN CHILDREN AND ADOLESCENTS
Although panic disorder is believed to emerge in late adolescence or early adulthood, adults with panic disorder often report having had panic symptoms starting in childhood or early adolescence (9). In most such individuals panic disorder may have either been misdiagnosed or not come to clinical attention. Epidemiological studies have reported that panic attacks may not be rare in the community samples of adolescents, although panic disorder may not be commonly reported. For instance, Goodwin and Gotlib (10) reported a prevalence of 3.3% of panic attacks from among 1,285 youth, aged 9–17 years, whereas Whitaker et al. (11) reported lifetime prevalence of panic disorder to be 0.6% using a structured interview with 5,000 students aged 14–17 years. A much higher prevalence of panic disorder has, however, been reported in the clinical samples. Biederman et al. (12) reported that 6% of the children and adolescents consecutively referred to their pediatric psychopharmacology clinic met the criteria for panic disorder. Similarly, Masi et al. (13) found that 10.4% of their consecutive outpatients referred to a mood and anxiety service had panic disorder.
Clinical presentation of panic symptoms in younger children compared with that in adolescents can be intriguing (14). Such a presentation can be manifested by the presence of atypical symptoms including “hyperventilation syndrome,” nocturnal occurrences, and fewer somatic and cognitive symptoms (15). Still, some of the common symptoms in younger children include palpitations, shortness of breath, sweating, faintness, and weakness (16). Among adolescents, symptoms such as chest pain, trembling, headache, and vertigo are reported (17). Another interesting developmental difference between the two age groups is that children and younger adolescents may attribute their symptoms to the external environment compared with older adolescents. Older adolescents are more competent of internal attributions that are more typically seen with panic disorder. Furthermore, cognitive symptoms appear only among adolescents (18). Interestingly, the fear of dying has been reported to be the earliest cognitive symptom whereas feelings of losing control and symptoms of depersonalization and derealization appear later (15, 17). Given the complexity of establishing a diagnosis of panic disorder in this population, the clinician may benefit by using brief self-reports and rating scales for anxiety disorders, some of which are even available for the preschool child. Table 2 lists some of the freely available assessment tools that include self-report, parent, and clinician versions.
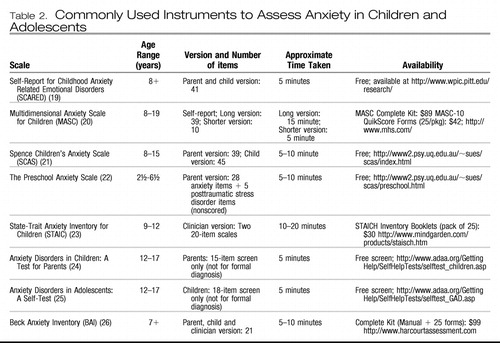 |
Table 2. Commonly Used Instruments to Assess Anxiety in Children and Adolescents
Another interesting aspect in this age group is the association of panic symptoms with comorbid anxiety disorders including separation anxiety disorder and generalized anxiety disorder (27, 28). Separation anxiety disorder has been reported to be associated with early-onset panic disorder but not necessarily with adult onset panic disorder (29). Similarly, agoraphobia has been reported more frequently in younger-onset panic disorder (30). Furthermore, mitral valve prolapse has also been associated with a higher incidence of panic disorder in the adolescent population (31). The clinician should also rule out any medical causes (such as pheochromocytoma and thyroid disease) and substance use disorders, both of which are well known to imitate panic disorder. More details are considered in the next section. Along with these comorbidities, a strong family history of panic disorder should cue the clinician to perform a detailed assessment for panic disorder in the child. Awareness of early-onset panic disorder and a detailed assessment can potentially improve diagnosis and treatment and thus decrease impairment and improve quality of life for these patients.
The American Academy of Child and Adolescent Psychiatry practice parameter for anxiety disorders also provides recommendations for assessment of various anxiety disorders. Although not specifically discussing panic disorder, the practice parameter recommends that clinicians routinely include screening questions about anxiety symptoms and that the questions should use developmentally appropriate language based on DSM-IV-TR criteria. If the screening indicates significant anxiety, the clinician should thoroughly evaluate the patient to determine the type, nature, frequency, and severity of the anxiety disorder and assess the functional impairment caused by it. Clinicians may also find it beneficial to use sections of the available diagnostic interviews such as the Anxiety Disorders Interview Schedule for DSM-IV-Child Version (ADIS). The ADIS has a Feelings Thermometer (ratings from 0 to 8) that may help children quantify and self-monitor ratings of fear and interference with functioning. Younger children may use more developmentally appropriate visual analogs such as smiley faces and upset faces to rate severity and interference (32).
ASSESSMENT IN THE ADULT POPULATION
As discussed initially, the DSM-IV-TR defines panic disorder as comprising discrete episodes of marked autonomic arousal that are accompanied by catastrophic thinking and are not directly caused by substance use or a medical condition. The DSM-IV-TR requires recurrent unexpected panic attacks plus at least 1 month of persistent concern about experiencing additional attacks, worry about the implications or consequences of attacks, or a significant change in behavior related to attacks to establish the diagnosis of panic disorder. The DSM-IV-TR criteria require that at least 4 of 13 criteria must be present to diagnose a “full” panic attack. When fewer than 4 of the 13 symptoms of a panic attack are present, this is referred to as “limited symptom attack.” Agoraphobia is a fear of places or situations from which escape might be difficult or in which help may be unavailable in the event of a panic attack or panic symptoms. The ICD-10 criteria for panic disorder are similar to the DSM criteria but do not specify a threshold beyond recurrent attacks (33). This section addresses three important areas for the clinician when assessing panic disorder: screening and assessment tools, comorbid psychiatric disorders, and associated medical conditions.
SCREENING AND ASSESSMENT TOOLS
The diagnosis of panic disorder is largely clinical in nature; yet the clinician may find some of the following screening and assessment tools useful and practical in the clinical setting. In the primary care setting, screening may be initiated with the two questions related to panic disorder from the five-question Anxiety and Depression Detector (34). These questions are:
In the last 3 months
| 1. | “Did you ever have a spell or an attack when all of a sudden you felt frightened, anxious or very uneasy?” and | ||||
| 2. | “Would you say that you have been bothered by ‘nerves’ or feeling anxious or on edge?” | ||||
These two questions have been reported to yield a high sensitivity and modest specificity and can be used for screening. The Anxiety Disorder Association of America has posted an online panic disorder self-test based on DSM-IV that can be used for self-report (35). In the psychiatric setting, assessment tools such as the Beck Anxiety Inventory may also be used for similar initial assessment. An online free html version is available (36). Although this is not a specific tool for assessment of panic disorder, it can point toward the severity of anxiety symptoms in the patient. Apart from monitoring the frequency and severity of panic attacks, the severity of agoraphobic avoidance and anticipatory anxiety may also be evaluated. The Panic Disorder Severity Scale (PDSS) and the Panic and Agoraphobia Scale (PAS) can be used to monitor the frequency and severity of panic attacks (37, 38). The Panic Disorder Severity Scale is a seven-item, interview-based scale for assessing the severity of panic disorder. Although not a diagnostic instrument, the PDSS provides a simple and efficient way to monitor panic disorder severity in patients in research and clinical settings for whom a diagnosis has been established (37). A self-report version of the scale has recently been tested and found to be reliable (39). More recently, another self-report scale, the Panic Disorder Self-Report has also been found to be valid and reliable (40). Structured instruments such as the Structured Clinical Interview for DSM-IV (SCID-IV) are often used in research settings (41).
ASSESSMENT OF MEDICAL CONDITIONS
Medical conditions may be associated with panic and other anxiety symptoms and need to be explored. Some of these disorders are pheochromocytoma, hyperthyroidism, supraventricular tachycardia, and Ménière's disease, among others (42).
Both hyper- and hypothyroidism can be associated with anxiety unaccompanied by other signs or symptoms. For this reason, it is imperative that all patients complaining of anxiety undergo routine thyroid function tests, including the evaluation of the level of thyroid-stimulating hormone. It is also important to note that thyroid disorders may initiate or trigger panic attacks. More importantly, as these panic attacks may get cued to other stimuli, even after the primary thyroid disease is corrected, panic attacks may continue unless treated specifically. Hyperparathyroidism can also present with anxiety symptoms and thus obtaining a serum calcium level may be desired (6, 43).
Cardiac conditions such as paroxysmal atrial tachycardia can be ruled out using an electrocardiogram (ECG) or, at times, 24-hour monitoring, if required. Similarly, over the years, there has been a lot of interest in the relationship of mitral valve prolapse to panic disorder. Although patients with mitral valve prolapse may complain of palpitations, chest pain, and lightheadedness, symptoms of a full-blown panic attack are rare. There have been reports of an underlying autonomic nervous system dysfunction or intermittent high catecholamine levels in patients with both mitral valve prolapse and panic disorder that may further highlight this connection. Interestingly, however, screening of patients with mitral valve prolapse has not revealed an increase in frequency of panic disorder compared with that in the general population (6, 43).
Pheochromocytoma is a rare tumor of the adrenal medulla that results in episodic bursts of catecholamines. These bursts are associated with intermittent elevated blood pressures, anxiety, flushing, and tremulousness. If suspected, a 24-hr urine sample should be collected and evaluated for catecholamine metabolites. Vestibular nerve disorders can also be associated with episodic vertigo, lightheadedness, and anxiety and may warrant a consultation with an ear, nose, and throat specialist or a neurologist (6, 43).
ASSESSMENT OF COMORBID PSYCHIATRIC CONDITIONS
Apart from a thorough assessment of comorbid medical disorders that may imitate panic or anxiety symptoms, various psychiatric disorders with predominant anxiety symptoms need to be distinguished from panic disorder for appropriate management. One of the common clinical conundrums is the association of panic-like symptoms with depression (44). Patients with depression can have frank panic attacks and thus manifest with symptoms and signs of anxiety. Similarly, patients who have a long-standing untreated or inadequately treated panic disorder have a poor quality of life and can become depressed over time. Although both these disorders can often be comorbid, the clinician may find it helpful to differentiate between the two. Some of the key points that may be helpful in such an assessment include the following:
| •. | Patients with predominant anxiety symptoms may not have the all of the vegetative symptoms seen in depression—they may have initial insomnia but not early morning awakening, they may not lose their appetite, and they may have minimal diminution in interest in activities (6, 44). The temporal onset of symptoms is also different—in patients with predominant panic disorder, anxiety attacks may be recalled initially followed by a feeling of depression; in contrast, primarily depressed patients will have an initial onset of depressive symptomatology that will be followed by anxiety. Furthermore, it has also been reported that patients suffering from atypical depression commonly have panic attacks although it is rarely associated with agoraphobia. | ||||
| •. | Patients with symptoms of posttraumatic stress disorder can be distinguished from those with panic disorder by the presence of a preexisting trauma and association with symptoms of avoidance, reexperiencing, and hyperarousal (45). | ||||
| •. | Patients with somatization disorder present with predominantly somatic symptoms that are persistently reported compared with the episodic nature of symptoms in panic disorder (43). | ||||
| •. | Patients with comorbid agoraphobia may present with fears of leaving home; they can be distinguished from those with paranoia and frank psychosis by the absence of positive psychotic symptoms and formal thought disorder (6, 43). | ||||
| •. | Also, as mentioned previously, substance abuse or withdrawal symptoms can also present with sudden onset of anxiety or panic symptoms. These can be distinguished by a temporal association between the substance abuse/withdrawal and onset of symptoms (6, 46). | ||||
ASSESSMENT IN THE ELDERLY
There is very limited literature on the subject of panic disorder in the geriatric population. As a result, most recommendations regarding assessment of panic disorder are derived and extrapolated from the adult literature. Flint et al. (47) have reported a decline in panic attacks in elderly individuals; however, it is important not to dismiss the significance of such anxiety symptoms in this population. Although the diagnostic criteria of panic disorder are similar to those in the general adult population, its presentation may vary in elderly individuals. Panic attacks in this population may be more reactive to transient situations or life changes (48). Many times elderly individuals may not complain of anxiety symptoms but focus on physical symptoms (49). They may not elaborate on their subjective apprehensive states but rather discuss bodily dysfunction. These complaints can force the clinician to delve into extensive medical investigations when the etiology may be more functional. On the contrary, because elderly individuals are more predisposed to having a medical comorbidity, it is imperative not to dismiss their physical complaints either. As a result, panic disorder has not been very well studied and more research on the subject is needed.
Apart from the variability in quality of symptoms for panic disorder in this population, the frequency and severity of reporting of symptoms may vary as well. Sheikh et al. (50) reported that elderly individuals with panic disorder report less severe and fewer panic symptoms, less anxiety and arousal, and higher levels of functioning compared to middle-aged patients with panic disorder. Furthermore, elderly patients with late-onset panic disorder may report less distress with panic symptoms compared with older patients with early-onset panic disorder (50). It may take quite a few panic attacks along with insignificant laboratory results in elderly patients to lead to a diagnosis of panic disorder. The medical comorbidities that may present with panic-like symptoms are similar to those mentioned in the adult population as listed in Table 3 and should be thoroughly assessed, especially in this older population.
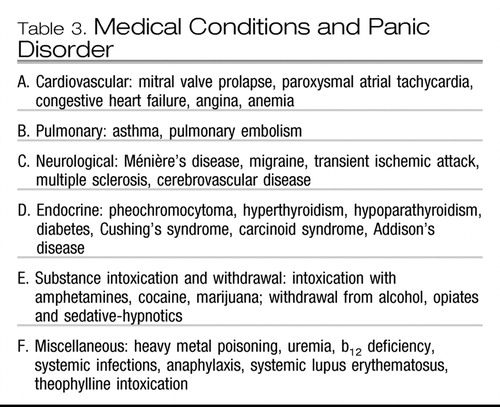 |
Table 3. Medical Conditions and Panic Disorder
To the best of the author's knowledge, there are no specific rating scales available for assessment of severity and diagnosis of panic disorder in the geriatric population, especially because panic disorder has not been very well studied in this age group and possibly also owing to a decline in panic attacks in the population. One of the newly developed scales, the Geriatric Anxiety Inventory (GAI) has recently been shown to measure common symptoms of anxiety in older adults. It consists of 20 items that can be answered in a dichotomous manner, which is “agree/disagree.” The GAI can be self-rated or administered by a trained health professional. The GAI, however, was not designed to diagnose specific anxiety disorders but rather to assess the severity of anxiety symptoms across a range of presentations in older adults (51). Clinicians also use some other assessment tools such as the Hamilton Anxiety Scale and Beck Anxiety Inventory for monitoring the anxiety symptoms that are often comorbid with both psychiatric and medical conditions. It is important to recognize and treat such comorbid anxiety disorders as they can have a significant impact on the quality of life in this population. In fact, it has been reported that such patients may also have a much increased risk of both suicidal attempts and completed suicides (52). In addition, there is also some evidence to suggest that late-onset panic attacks may be due to preexisting depression (48). Furthermore, anxiety may also be a predictor of decline in cognitive functions, which should be simultaneously evaluated (53).
The diagnosis of panic disorder is based on a thorough history (from both the patient and the patient's family or caregivers), mental state examination, physical examination, and investigations selected to screen for medical etiology that could be contributing to symptoms. Initial screening investigations may include a complete blood count, fasting serum glucose level, serum calcium level, thyroid function tests, and an ECG. Physicians should have a high index of suspicion for panic attacks in older patients with multiple episodic physical symptoms that are not explained by physical examination and investigations. In addition, symptoms such as derealization, depersonalization, and fear of losing control should also alert the clinician to the possibility of panic disorder.
CONCLUSIONS
Panic disorder is a common, often impairing, anxiety disorder that usually presents in late adolescence or early adulthood. However, an onset in childhood or in the geriatric age group should not be discounted without an adequate and thorough assessment. Clinicians should always screen their patients in all age groups for panic disorder, using some of the DSM-IV-TR-based screening aids. Patients with panic disorder should always be assessed for comorbid psychiatric disorders and causative medical illnesses that may present as panic attacks. Clinicians should also be aware of the variability in clinical presentations that may be associated with both the pediatric and geriatric age groups.
1 Roy-Byrne PP, Craske MG, Stein MB: Panic disorder. Lancet 2006; 368:1023–1032Crossref, Google Scholar
2 Marchesi C: Pharmacological management of panic disorder. Neuropsychiatr Dis Treat 2008; 4:93–106Crossref, Google Scholar
3 Hanisch LJ, Hantsoo L, Freeman EW, Sullivan GM, Coyne JC: Hot flashes and panic attacks: a comparison of symptomatology, neurobiology, treatment, and a role for cognition. Psychol Bull 2008; 134:247–269Crossref, Google Scholar
4 Perugi G, Frare F, Toni C: Diagnosis and treatment of agoraphobia with panic disorder. CNS Drugs 2007; 21:741–764Crossref, Google Scholar
5 Foldes-Busque G, Marchand A, Landry P: Early detection and treatment of panic disorder with or without agoraphobia: update. Can Fam Physician 2007; 53:1686–1693Google Scholar
6 Hollander E, Simeon D: Anxiety disorders, in The American Psychiatric Publishing Textbook of Neuropsychiatry and Behavioral Sciences, 5th ed. Edited by Yudofsky SC, Hales RE. Washington DC, American Psychiatric Publishing, 2008Google Scholar
7 Masi G, Pari C, Millepiedi S: Pharmacological treatment options for panic disorder in children and adolescents. Expert Opin Pharmacother 2006; 7:545–554Crossref, Google Scholar
8 Starcevic V: Treatment of panic disorder: recent developments and current status. Expert Rev Neurother 2008; 8:1219–1232Crossref, Google Scholar
9 Kessler RC, Wang PS: The descriptive epidemiology of commonly occurring mental disorders in the United States. Annu Rev Public Health 2008; 29:115–129Crossref, Google Scholar
10 Goodwin RD, Gotlib IH: Panic attacks and psychopathology among youth. Acta Psychiatr Scand 2004; 3:216–221Crossref, Google Scholar
11 Whitaker A, Johnson J, Shaffer D, Rapoport JL, Kalikow K, Walsh BT, Davies M, Braiman S, Dolinsky A: Uncommon troubles in young people: prevalence estimates of selected psychiatric disorders in a nonreferred adolescent population. Arch Gen Psychiatry 1990; 47:487–496Crossref, Google Scholar
12 Biederman J, Faraone SV, Marrs A, Moore P, Garcia J, Ablon S, Mick E, Gershon J, Kearns ME: Panic disorder and agoraphobia in consecutively referred children and adolescents. J Am Acad Child Adolesc Psychiatry 1997; 36:214–223Crossref, Google Scholar
13 Masi G, Favilla L, Mucci M, Millepiedi S: Panic disorder in clinically referred children and adolescents. Child Psychiatry Hum Dev 2000; 31:139–151Crossref, Google Scholar
14 Reinblatt SP, Riddle MA: The pharmacological management of childhood anxiety disorders: a review. Psychopharmacology (Berl) 2007; 191:67–86Crossref, Google Scholar
15 Masi G, Pari C, Millepiedi S: Pharmacological treatment options for panic disorder in children and adolescents. Expert Opin Pharmacother 2006; 7:545–554Crossref, Google Scholar
16 King NJ, Gullone E, Tonge BJ, Ollendick TH: Self-reports of panic attacks and manifest anxiety in adolescents. Behav Res Ther 1993; 31:111–116Crossref, Google Scholar
17 Diler RS: Panic disorder in children and adolescents. Yonsei Med J 2003; 44:174–179Crossref, Google Scholar
18 Nelles WB, Barlow DH: Do children panic? Clin Psychol Rev 1988; 8:359–372Crossref, Google Scholar
19 Self-Report for Childhood Anxiety Related Emotional Disorders (SCARED). http://www.wpic.pitt.edu/research/Google Scholar
20 Multidimensional Anxiety Scale for Children (MASC). http://www.mhs.com/Google Scholar
21 Spence Children's Anxiety Scale (SCAS). http://www2.psy.uq.edu.au/~sues/scas/index.htmlGoogle Scholar
22 The Preschool Anxiety Scale. http://www2.psy.uq.edu.au/∼sues/scas/preschool.htmGoogle Scholar
23 State-Trait Anxiety Inventory for Children (STAIC). http://www.mindgarden.com/products/staisch.htmGoogle Scholar
24 Anxiety Disorders in Children: A Test for Parents. http://www.adaa.org/GettingHelp/SelfHelpTests/selftest_children.aspGoogle Scholar
25 Anxiety Disorders in Adolescents: A Self-Test. http://www.adaa.org/GettingHelp/SelfHelpTests/selftest_GAD.aspGoogle Scholar
26 Beck Anxiety Inventory. http://www.harcourtassessment.comGoogle Scholar
27 Klein RG: Is panic disorder associated with childhood separation anxiety disorder?. Clin Neuropsychopharmacol 1995; 18(suppl 2):7–14Crossref, Google Scholar
28 Masi G, Mucci M, Millepiedi S, Poli P, Bertini N, Akiskal HS: Generalized anxiety disorder in children and adolescents. J Am Acad Child Adolesc Psychiatry 2004; 43:752–760Crossref, Google Scholar
29 Masi G, Mucci M, Millepiedi S: Separation anxiety in children and adolescents: epidemiology, diagnosis and management. CNS Drugs 2001; 15:93–104Crossref, Google Scholar
30 Battaglia M, Bertella M, Politi E, Bernardeschi L, Perna G, Gabriele A, Bellodi L: Age of onset of panic disorder: influence of familial liability to the disease and of childhood separation anxiety disorder. Am J Psychiatry 1995; 152:1362–1364Crossref, Google Scholar
31 Toren P, Eldar S, Cendor D, Wolmer L, Weizmean R, Zubadi R, Koren S: The prevalence of mitral valve prolapse in children with anxiety disorders. J Psychiatr Res 1999; 33:357–361Crossref, Google Scholar
32 Practice parameter for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry 2007; 46:267–283Crossref, Google Scholar
33 Neurotic, stress-related and somatoform disorders (F40–F48). http://www.who.int/classifications/apps/ICD/icd10online/Google Scholar
34 Means-Christensen AJ, Sherbourne CD, Roy-Byrne PP, Craske MG, Stein MB: Using five questions to screen for five common mental disorders in primary care: diagnostic accuracy of the Anxiety and Depression Detector. Gen Hosp Psychiatry 2006; 28:108–118Crossref, Google Scholar
35 Panic Disorder Self Test. http://www.adaa.org/GettingHelp/SelfHelpTests/selftest_Panic.aspGoogle Scholar
36 Beck Anxiety Inventory. www.carrettin.com/forms/Beck_Anxiety_Inventory.pdfGoogle Scholar
37 Shear MK, Brown TA, Barlow DH, Money R, Sholomskas DE, Woods SW, Gorman JM, Papp LA: Multicenter collaborative panic disorder severity scale. Am J Psychiatry 1997; 154:1571–1575Crossref, Google Scholar
38 Bandelow B: Panic and Agoraphobia Scale (P&A/PAS). http://wwwuser.gwdg.de/∼ukyp/pas.htmGoogle Scholar
39 Houck PR, Spiegel DA, Shear MK, Rucci P: Reliability of the self-report version of the panic disorder severity scale. Depress Anxiety 2002; 15:183–185Crossref, Google Scholar
40 Newman MG, Holmes M, Zuellig AR, Kachin KE, Behar E: The reliability and validity of the panic disorder self-report: a new diagnostic screening measure of panic disorder. Psychol Assess 2006; 18:49–61Crossref, Google Scholar
41 Structured Clinical Interview for DSM Disorders (SCID-IV). http://www.scid4.org/Google Scholar
42 American Psychiatric Association: Practice Guideline for the Treatment of Patients with Panic Disorder. Am J Psychiatry 1998; 155(May suppl):1–60Crossref, Google Scholar
43 Sadock BJ, Sadock VA, Editors: Kaplan and Sadock's Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry, 10th ed. Philadelphia, Lippincott Williams & Wilkins, 2007, p. 593Google Scholar
44 Simon NM, Fischmann D: The implications of medical and psychiatric comorbidity with panic disorder. J Clin Psychiatry 2005; 4:8–15Google Scholar
45 McNally RJ: Panic and posttraumatic stress disorder: implications for culture, risk, and treatment. Cogn Behav Ther 2008; 37:131–134Crossref, Google Scholar
46 Zimmermann P, Wittchen HU, Höfler M, Pfister H, Kessler RC, Lieb R: Primary anxiety disorders and the development of subsequent alcohol use disorder: a 4-year community study of adolescents and young adults. Psychol Med 2003; 33:1211–1222Crossref, Google Scholar
47 Flint AJ, Cook JM, Rabins PV: Why is panic disorder less frequent in late-life? Am J Geriatr Psychiatry 1996; 4:96–109Crossref, Google Scholar
48 Flint AJ, Gagnon N: Diagnosis and management of panic disorder in older patients. Drugs Aging 2003; 20:881–891Crossref, Google Scholar
49 Ballenger JC: Unrecognized prevalence of panic disorder in primary care, internal medicine and cardiology. Am J Cardiol 1987; 60:39J–47JCrossref, Google Scholar
50 Sheikh JI, King RJ, Taylor CB; Comparative phenomenology of early-onset versus late-onset panic attacks: a pilot survey. Am J Psychiatry 1991; 148:1231–1233Crossref, Google Scholar
51 Pachana NA, Byrne GJ, Siddle H, Koloski N, Harley E, Arnold E: Development and validation of the Geriatric Anxiety Inventory. Int Psychogeriatr 2007; 1:103–114Crossref, Google Scholar
52 Khan A, Leventhal RM, Khan S, Brown WA: Suicide risk in patients with anxiety disorders: a meta-analysis of the FDA database. J Affect Disord 2002; 68:183–190Crossref, Google Scholar
53 Sinoff G, Werner P: Anxiety disorder and accompanying subjective memory loss in the elderly as a predictor of future cognitive decline. Int J Geriatr Psychiatry 2003; 18:951–959Crossref, Google Scholar