Illness Management and Recovery: A Review of the Research
Abstract
Illness management is a broad set of strategies designed to help individuals with serious mental illness collaborate with professionals, reduce their susceptibility to the illness, and cope effectively with their symptoms. Recovery occurs when people with mental illness discover, or rediscover, their strengths and abilities for pursuing personal goals and develop a sense of identity that allows them to grow beyond their mental illness. The authors discuss the concept of recovery from psychiatric disorders and then review research on professional-based programs for helping people manage their mental illness. Research on illness management for persons with severe mental illness, including 40 randomized controlled studies, indicates that psychoeducation improves people’s knowledge of mental illness; that behavioral tailoring helps people take medication as prescribed; that relapse prevention programs reduce symptom relapses and rehospitalizations; and that coping skills training using cognitive-behavioral techniques reduces the severity and distress of persistent symptoms. The authors discuss the implementation and dissemination of illness management programs from the perspectives of mental health administrators, program directors, people with a psychiatric illness, and family members.
In recent years, interest in identifying and implementing evidence-based practices for mental health services has been growing (1, 2). Criteria used to determine whether a practice is supported by research typically include all of the following: standardized interventions examined in studies that use experimental designs, similar research findings obtained from different investigators, and objective assessment of broadly accepted important outcomes, such as reducing symptoms and improving social and vocational functioning (3, 4). On the basis of these criteria, several psychosocial treatments for persons with severe mental illness are supported by evidence, including assertive community treatment (5), supported employment (6), family psychoeducation (7), and integrated treatment for mental illness and concomitant substance abuse (8). The standardization and dissemination of evidence-based practices is expected to improve outcomes for the broader population of people who use mental health services (9).
In this article, we examine the research that supports interventions for helping people collaborate with professionals in managing their mental illness while pursuing their personal recovery goals. We begin by defining illness management. Next, we discuss the concept of recovery and the role of illness management in aiding the recovery process. We then review research on illness management programs, and we conclude by considering issues involved in the dissemination and implementation of these programs.
Defining illness management
The practice in medicine of professionals teaching persons with medical diseases and their families about the diseases in order to improve adherence to recommended treatments and to manage or relieve persistent symptoms and treatment side effects has a long history (10–12). Education-based approaches are especially common in the treatment of chronic illnesses such as diabetes, heart disease, and cancer. In the mental health field, didactic methods for educating people have been referred to as psychoeducation (13–15). Other methods, especially cognitive-behavioral strategies, have also been used to help people learn how to manage their mental illnesses more effectively.
People with psychiatric disorders can be given information and taught skills by either professionals or peers to help them take better care of themselves. Although the goals of professional-based and peer-based teaching are similar, we distinguish between them for practical reasons. Professional-based intervention is conducted in the context of a therapeutic relationship in which the teacher—or the organization to which the teacher belongs, such as a community mental health center—is responsible for the overall treatment of the individual’s psychiatric disorder. In contrast, peer-based intervention is conducted in the context of a relationship in which the teacher—or the organization to which the teacher belongs, such as a peer support center —usually does not have formal responsibility for the overall treatment of the individual’s disorder. Given this distinction, the relationship between a professional and the person with a mental illness may be perceived as hierarchical, because the professional assumes responsibility for the person’s treatment, whereas the relationship between a peer and the person with a mental illness is less likely to be perceived as hierarchical, because the peer does not assume such responsibility. This distinction is crucial among individuals with psychiatric disorders who have advocated for self-help and peer-based services as alternatives to, or in addition to, traditional professional-based services (16–18).
Another reason for distinguishing interventions delivered by professionals from those provided by peers is that most professionals do not have serious psychiatric disorders—in contrast, by definition, to peers. Thus when teaching others how to manage their mental illness, peers are able to convey the lessons they have learned from personal experience, whereas professionals cannot. This places peers in a unique position of being able to teach “self” management skills to other persons with a mental illness.
To recognize these differences, we propose a distinction between professional-based services and peer-based services aimed at helping people deal with their psychiatric disorders. We define illness management as professional-based interventions designed to help people collaborate with professionals in the treatment of their mental illness, reduce their susceptibility to relapses, and cope more effectively with their symptoms. We suggest that illness self-management be used to refer to peer-facilitated services aimed at helping people cope more effectively with their mental illness and facilitating people’s ability to take care of themselves. In this article we focus on the substantial body of controlled research addressing the effectiveness of illness management. Although a variety of illness self-management programs have been developed (19–22), rigorous controlled research evaluating the effects of these programs has not been completed.
Recovery
Illness management programs have traditionally provided information and taught strategies for adhering to treatment recommendations and minimizing symptoms and relapses. However, many programs go beyond this focus on psychopathology and strive to improve self-efficacy and self-esteem and to foster skills that help people pursue their personal goals. Enhanced coping and the ability to formulate and achieve goals are critical aspects of rehabilitation and are in line with the recent emphasis on recovery in the mental health self-help movement. We briefly address the relevance of illness management to recovery here.
According to Anthony (23), “Recovery involves the development of new meaning and purpose in one’s life as one grows beyond the catastrophic effects of mental illness.” Recovery refers not only to short-term and long-term relief from symptoms but also to social success and personal accomplishment in areas that the person defines as important (24–26). Recovery has been conceptualized as a process, as an outcome, and as both (27–30). What is critical about recovery is the personal meaning that each individual attaches to the concept. Common themes of recovery are the development of self-confidence, of a self-concept beyond the illness, of enjoyment of the world, and of a sense of well-being, hope, and optimism (31–34).
Critical to people’s developing hope for the future and formulating personal recovery goals is helping them gain mastery over their symptoms and relapses. Basic education about mental illness facilitates their ability to regain control over their lives and to establish more collaborative and less hierarchical relationships with professionals (16, 35–37). Although relapses and rehospitalizations are important learning opportunities (38–40), prolonged periods of severe symptoms can erode a person’s sense of well-being, and avoiding the disruption associated with relapses is a common recovery goal (30, 41). Improvement in coping with symptoms and the stresses of daily life is another a common theme of recovery, because such improvement allows people to spend less time on their symptoms and more time pursuing their goals (27, 30, 42). Thus illness management and recovery are closely related, with illness management focused primarily on minimizing people’s symptoms and relapses and recovery focused primarily on helping people develop and pursue their personal goals.
Research on illness management
Although illness management and recovery are intertwined, almost all the available treatment research pertains to illness management. Thus we confined our research review to studies of illness management programs. Because extensive research has been conducted on illness management, we confined our review to randomized clinical trials. We also limited our review to programs that addressed schizophrenia, bipolar disorder, and the general group of severe or serious mental illnesses, excluding studies that focused on major depression or borderline personality disorder. Studies included in this review were identified through a combination of strategies, including literature searches on PsycINFO and MEDLINE, inspection of previous reviews, and identification of studies presented at conferences.
With respect to outcomes, we examined the effects of different interventions on two proximal outcomes and three distal outcomes. The proximal outcomes are knowledge of mental illness and using medication as prescribed. The distal outcomes are relapses and rehospitalizations, symptoms, and social functioning or other aspects of quality of life. Distal outcomes are of inherent interest because they are defined in terms of the nature of the mental illness and associated problems. Proximal outcomes are of interest because they are related to important distal outcomes. Specifically, knowledge of mental illness is critical to the involvement of people with psychiatric disorders as informed decision makers in their own treatment (14, 15). Using medication as prescribed is important because medications are effective for preventing symptom relapses and rehospitalizations for persons with severe mental illness (43, 44), yet many people do not take medications (45), and nonadherence accounts for a significant proportion of relapses and inpatient treatment costs (46). Although adherence to medication regimens is important in and of itself, illness management approaches involve forming partnerships between clinicians and persons with a mental illness in order to determine the services each person needs, including medication, and respecting patients’ rights to make decisions about their own treatment (36).
The literature review was divided into five areas: broad-based psychoeducation programs, medication-focused programs, relapse prevention, coping skills training and comprehensive programs, and cognitive-behavioral treatment of psychotic symptoms.
Broad-based psychoeducation programs
Most broad-based programs, summarized in Table 1, provided information to people about their mental illness, including symptoms, the stressvulnerability model, and treatment. Among the four controlled studies, all but one (47) provided at least eight sessions of psychoeducation. Follow-up periods ranged from ten days (15) to two years (48). Three of the controlled studies found that psychoeducation improved knowledge about mental illness (15, 47, 48); one did not (49). In two studies, improved knowledge had no effect on taking medication as prescribed (47, 49); one study reported improved adherence (48).
In summary, research on broad-based psychoeducation indicates that it increases participants’ knowledge about mental illness but does not affect the other outcomes studied. This finding may not be surprising: similar didactic information given to families of persons with schizophrenia has been found to increase their knowledge but not to affect their behavior (50, 51). The reason for this may be that didactic information does not consider beliefs and illness representations already held by recipients (52). Nevertheless, psychoeducation remains important because access to information about mental illness is crucial to people’s ability to make informed decisions about their own treatment, and psychoeducation is the foundation for more comprehensive programs (as reviewed below).
Medication-focused programs
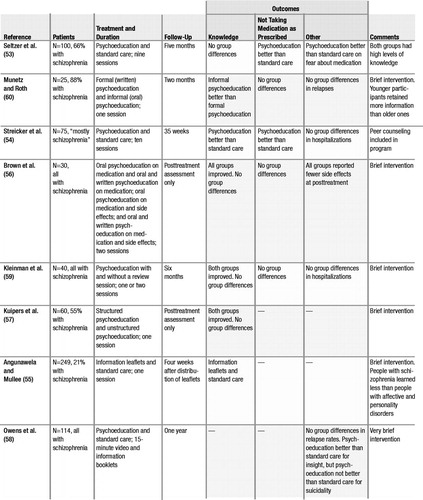
Studies that strove to foster collaboration between people with a mental illness and professionals regarding taking medication used psychoeducational or cognitive-behavioral approaches or a combination of the two.
Psychoeducation about medication involves providing information about the benefits and the side effects of medication and teaching strategies for managing side effects, so that people can make informed decisions about taking medication. These programs, summarized in Table 2, tended to be brief, with only two of eight programs (53, 54) lasting more than one or two sessions. Three studies conducted posttreatment-only follow-up assessments (55–57), and five studies conducted follow-ups after the end of treatment (53, 54, 58–60). Most of the studies reported that participants increased their knowledge about medication. However, three studies reported no group differences in taking medication as prescribed (56, 59, 60); a fourth study reported improvements (53); and a fifth study reported deterioration in taking medication (54). The three studies that found no differences in taking medication as prescribed compared different psychoeducational methods (56, 59, 60). Only one study that assessed medication adherence included a no-treatment control group (54); this study found that clients who received psychoeducation were more likely than clients who received no psychoeducation to discontinue medication. A somewhat disconcerting finding was reported in the only other study with a no-treatment control group (58). This study found that psychoeducation increased clients’ insight into their illness but also increased clients’ suicidality; psychoeducation had no influence on other symptoms or on relapse rates. In summary, research on the effects of psychoeducation about medication indicates that it improves knowledge about medication, but little evidence indicates that it improves taking medication as prescribed or affects other areas of functioning.
Cognitive-behavioral programs that focused on medication used one of several techniques: behavioral tailoring, simplifying the medication regimen, motivational interviewing, or social skills training. Behavioral tailoring involves working with people to develop strategies for incorporating medication into their daily routine—for example, placing medication next to one’s toothbrush so it is taken before brushing one’s teeth (61). Behavioral tailoring may also include simplifying the medication regimen, such as taking medication once or twice a day instead of more often. Motivational interviewing, based on the approach developed for the treatment of substance abuse (62), involves helping people articulate personally meaningful goals and exploring how medication may be useful in achieving those goals. Social skills training involves teaching people skills to improve their interactions with prescribers, such as how to discuss medication side effects (63).
Cognitive-behavioral programs for medication are summarized in Table 3. All four studies of behavioral tailoring found improvements in taking medication as prescribed (61, 64–66), as did the one study that evaluated the effect of simplifying the medication regimen (67). One study of motivational interviewing (68) also reported an increase in taking medication as prescribed, as well as fewer symptoms and relapses and improved social functioning. One broad-based cognitive-behavioral program also reported lower rates of rehospitalization (69). The two studies that examined social skills training were limited. One of these studies found that skills training had no effect on knowledge about medication, but medication adherence was not directly assessed (70). The other study showed that psychoeducation and skills training improved knowledge and social skills in medication-related interactions, but it did not assess taking medication as prescribed (71).
Thus controlled research, which has focused mainly on individuals with schizophrenia, provides the strongest support for the effects of cognitive-behavioral methods (chiefly, behavioral tailoring) for increasing their taking of medication as prescribed, whereas psychoeducation alone has limited, if any, impact. The strong effects of behavioral tailoring on taking medication, compared with the weak effects of psychoeducation, suggest that memory problems, which are common in schizophrenia (72), may interfere with taking medication as prescribed and that behavioral tailoring may work by helping people develop their own cues to take medication, thereby compensating for cognitive impairments.
Most of the programs reviewed were response-based, with little effort made to understand the psychology of why people did not take medication as prescribed. This is very different from the theoretical position in health psychology, in which complex models such as the health belief model and the theory of planned action have been developed to understand health-related behavior. Preliminary studies investigating medication self-administration have used the concept of psychological reactance, which is a motivational state that can develop when a person perceives a threat to his or her personal freedom (73). In an analogue study, reactance-prone individuals rated themselves as being less likely to take medication if their freedom of choice was restricted, whereas no effect of freedom of choice was seen in non–reactance-prone participants (74). In a study of people with schizophrenia or schizoaffective disorder, individuals with higher psychological reactance who perceived taking medication as a threat to their freedom of choice were less likely to have taken medication as prescribed in the past (75). Motivational interviewing may provide one strategy for improving people’s understanding of medication and addressing their concerns about taking medication, while respecting their decision about whether or not to use medication. However, only one controlled study has evaluated the effects of motivational interviewing on taking medication as prescribed, and this study is in need of replication.
Relapse prevention
Controlled studies of relapse prevention programs are summarized in Table 4. Relapse prevention programs focus on teaching people how to recognize environmental triggers and early warning signs of relapse and taking steps to prevent further symptom exacerbations (76–81). These programs also teach stress management skills. Because a person may not be fully aware that a relapse is happening (82, 83), two of the five relapse prevention programs included groups to train relatives to help in the identification of early warning signs of relapse (76, 78).
The five studies of relapse prevention programs all showed decreases in relapse or rehospitalization. These findings are consistent with the findings of a large, uncontrolled study of 370 people with severe mental illness in which teaching the early warning signs of relapse was associated with better outcomes, including fewer relapses and rehospitalizations and lower treatment costs (84). This benefit of involving relatives in relapse prevention programs is consistent with research that shows that family intervention is effective in preventing relapses (7).
Coping skills training and comprehensive programs
Controlled studies of coping skills training and comprehensive programs are summarized in Table 5. Coping programs aim to increase people’s ability to deal with symptoms or stress or with persistent symptoms (85–90). Comprehensive programs incorporate a broad array of illness management strategies, including psychoeducation, relapse prevention, stress management, coping strategies, and goal setting and problem solving (91–94).
The four studies of coping skills were quite different, both in the methods employed and in the targets of the intervention. Leclerc and colleagues (85) taught an integrative coping skills approach based on Lazarus and Folkman’s model of coping (95, 96), which emphasizes the importance of cognitive appraisal in perceiving threat. Lecomte and colleagues (86) addressed general coping skills through building up participants’ sense of empowerment. Schaub (87) and Schaub and Mueser (88) taught skills for managing stress and persistent symptoms, combined with basic psychoeducation about schizophrenia. Despite the differences in the programs, all the coping skills programs employed cognitive-behavioral techniques and produced uniformly positive results in reducing symptom severity. Thus research evidence shows that coping skills training is effective.
The three studies of comprehensive programs—that is, those using a broad range of techniques—are somewhat difficult to compare because they differed in the clinical methods used. Atkinson and coworkers (91) evaluated a program that combined morning educational presentations and afternoon sessions in which problem solving was applied to the educational topics. Hogarty and associates (92, 93) evaluated the effects of personal therapy, a broad-based approach incorporating psychoeducation, stress management, and development of adaptive coping skills to promote social reintegration, and compared these effects with the effects of supportive therapy. They found that personal therapy prevented relapses only for people living with families. However, people receiving personal therapy improved in social functioning, whether they were living at home or not. Hornung and colleagues (94) examined the effects of different combinations of psychoeducation, problem-solving training, and key-person counseling (such as counseling family members) and found that people who received all three had fewer relapses over five years. These three studies suggest that comprehensive programs improve the outcome of schizophrenia, but the differences between programs preclude any definitive conclusions about which approaches may be most effective.
Cognitive-behavioral treatment of psychotic symptoms
Over the past 50 years, since the early work of Beck (97), cognitive-behavioral therapy has been used to help clients with psychotic symptoms cope more effectively with the distress associated with symptoms or to reduce symptom severity. Cognitive-behavioral approaches to psychosis include teaching coping skills, such as distraction techniques to reduce preoccupation with symptoms (98), and modifying clients’ dysfunctional beliefs about the illness, the self, or the environment (99). In recent years, several manuals have been developed for cognitive-behavioral therapy for psychosis (100–102).
Over the past decade, eight controlled studies of time-limited cognitive-behavioral therapy for psychosis have been conducted—six in England (89, 90, 103–112), one in Canada (113), and one in Italy (114). Because several comprehensive reviews of this research (115), including two meta-analyses (116, 117), have recently been published, we do not review the results of these studies in detail here. The consistent finding across these studies has been that cognitive-behavioral treatment is more effective than supportive counseling or standard care in reducing the severity of psychotic symptoms. Furthermore, studies that assess negative symptoms, such as social withdrawal and anhedonia, also report beneficial effects from cognitive-behavioral therapy on these symptoms.
Summary of research
The results of controlled research indicate that when illness management is conceptualized as a group of specific interventions, it is an evidence-based practice. The core components of illness management and the evidence supporting them can be summarized as follows. With respect to the more proximal outcomes, three studies (15, 47, 48) found that psychoeducation was effective at increasing knowledge about mental illness, and a fourth (49) did not. Similarly, all four studies of behavioral tailoring found that it was effective in improving the taking of medication as prescribed (61, 64–66). In terms of the more distal outcomes, all five studies of training in relapse prevention found that it reduced relapses and rehospitalizations (76–81), all four studies of teaching coping skills found that it reduced the severity of symptoms (85–88), and all eight studies of cognitive-behavioral treatment of persistent psychotic symptoms reported that it reduced the severity of psychotic symptoms (89, 103, 107–109, 112–114). Although some studies of coping skills training differed in the symptoms they targeted, they all employed time-limited, cognitive-behavioral interventions. Thus psychoeducation, behavioral tailoring for medication, training in relapse prevention, and coping skills training employing cognitive-behavioral techniques are strongly supported components of illness management. Confidence in these findings is bolstered by the fact that the majority of the studies cited above were based on treatment manuals, and all except the studies by Schaub (87) and Schaub and Mueser (88) and the study by Tarrier and colleagues (89, 112) were conducted by different groups of investigators.
The three studies of comprehensive illness management (91–94) suggest emerging evidence of the effectiveness of such programs. Improvements were seen in several important areas, such as social adjustment (92, 93) and quality of life (91). However, the differences between the components of the programs and their target outcomes preclude the drawing of any definitive conclusions about them.
Although the results of these studies support several components of illness management, the studies’ limitations should be acknowledged. First, most research has focused on persons with schizophrenia, which limits the findings’ generalizability. Second, few replications of standardized interventions have been published. Third, most research examines the effects of teaching illness management, with less attention paid to recovery. Although coping and symptom relief are important aspects of recovery (27, 30, 42), little controlled research has examined the effect of interventions on the broader dimensions of recovery, such as developing hope, meaning, and a sense of purpose in one’s life.
Implementation and dissemination issues
Strategies for implementing and disseminating evidence-based practices are critical to keeping these practices from languishing on the academic shelf and yielding little effect in routine mental health settings. Some illness management strategies, including psychoeducation, behavioral tailoring to address willingness to take medication as prescribed, relapse prevention skills, and cognitive-behavioral treatment of persistent symptoms, are available in some settings, but no empirically supported programs are in widespread use. Generic strategies for implementing new psychiatric treatment and rehabilitation programs have been described elsewhere (118). We consider implementation and dissemination issues from the perspectives of four stakeholders: mental health system administrators, program directors, people with mental illness, and family members of people with mental illness. As virtually no controlled data are available on specific strategies for disseminating and implementing new programs, the recommendations provided below are based on the experiences of the authors and other reports in the literature.
Mental health system administrators
Several issues are relevant for administrators attempting to implement illness management approaches, including the selection or development of manuals, monitoring adherence to the model, policies and procedures, and funding.
Although the research supports several practices for teaching illness management, the specific components have not previously been conceptualized and standardized as a unitary package or manual, except in the context of comprehensive programs that go well beyond what the evidence supports. The availability of a treatment manual is critical for broad-scale implementation of a practice. The identification of critical practice components for illness management, supported by research, may facilitate the development of such a manual.
Policies supporting illness management as a core capacity in a service system are important for implementing such programs (119). These policies include the development of program standards that identify illness management as a specific service modality and require it as a necessary capacity in contracts with service providers and managed care entities. Compared with other evidence-based practices, illness management services are not expensive, nor do they require major organizational restructuring to implement. In fact, clinicians routinely work to help people with mental illness improve their capacity to manage their illness and achieve their personal goals. The identification and standardization of core ingredients of illness management will allow clinicians to do what they are already trying to do in a more organized, systematic, and effective manner.
Both the clinic and the rehabilitation options in state Medicaid plans can be used to support illness management services if the services are led by traditionally credentialed staff. When partnerships are sought between clinical staff and peer facilitators as leaders in teaching illness management skills, available resources must support curriculum development and implementation must include ways to accomplish this expansion. Although research has not examined the effects of partnerships between professionals and peers in providing illness management skills, the overlap in curriculum between the programs reviewed here and peer-based illness self-management programs (20) suggests that such collaborations should be considered. Many states that have implemented these initiatives have used combinations of federal block grant funds, Community Action Grants from the Center for Mental Health Services, and legislatively appropriated county and state funds.
The continuity of an illness management program is strengthened by the development of a leadership group that meets regularly and is composed of people with mental illness, their family members, mental health service providers, and mental health service administrators. Such a group can review the progress of the program, develop evaluation plans, assist in addressing system barriers, and create policies as needed to support the program. Finally, such a group can facilitate the regular meeting of providers of illness management training to share teaching experiences, provide mutual support, and assist in curriculum refinement.
Mental health program directors
Program directors need to select a curriculum that successfully integrates psychosocial and medical approaches to illness management. If the approach that is adopted involves people with psychiatric disorders as peer educators, a variety of policies and procedures need to be in place. These include supporting the employment of peers, practices that support reasonable accommodations for employees with disabilities, and supervision to help ensure appropriate boundaries between staff, peer-staff, and the people with mental illness who are the focus of treatment.
Another consideration is whom to target for illness management. Many program directors extend the opportunity to anyone who wants to attend, regardless of symptoms or rehabilitation status, on the grounds that desire to participate is the most important criterion for selection.
Program directors may find it helpful to integrate illness management principles throughout their organization. Case managers, therapists, crisis clinicians, and prescribing psychiatrists all have important roles in helping people use skills and in reinforcing management concepts. As with other service initiatives, the effect of illness management education is enhanced when the organization adopts its principles widely. Offering ongoing training rather than one-time courses can enhance the impact of illness management education. In addition, teaching a curriculum in short segments that are often repeated can be successful.
People with mental illness and their family members
The potential effect of illness management initiatives on people with mental illness is significant. Although the benefits of learning how to manage one’s illness and make progress toward recovery are compelling, people report that recovery is hard work (26, 120). The switch from being a passive recipient of care to an active partner is very challenging. People with psychiatric disorders and their relatives may feel justifiably ambivalent about these approaches (121). For example, a person learning about ways that others cope with symptoms may consider it a personal failure if he or she uses these methods but continues to experience symptoms. Programs that adopt fail-safe principles, such as unconditional support, zero exclusion, and easy reentry, support individuals’ own recoveries and prevent people from internalizing a sense of failure.
Family members may be concerned that educational approaches will be used in lieu of established medical and psychosocial treatments. Family members may consider the idea of recovery unrealistic, or they may be concerned that their relative is not ready to assume a more responsible role in treatment. Whether or not the person lives with relatives, relatives are likely to have a significant, although perhaps a subtly perceived, role in their family member’s attitude toward recovery. Thus it is critical that the family understand and be involved in illness management education and that they appreciate its relevance to recovery.
Conclusions
It is now widely recognized that people with mental illness can participate actively in their own treatment and can become the most important agents of change for themselves. Illness management skills, ranging from greater knowledge of psychiatric illness and its treatment to coping skills and relapse prevention strategies, play a critical role in people’s recovery from mental illness. Research on illness management has thus far focused on programs developed and run by professionals. This research provides support for illness management programs and guidance on their effective components. Similar research on peer-based illness self-management programs may inform professional-based services and lead to collaborative efforts.
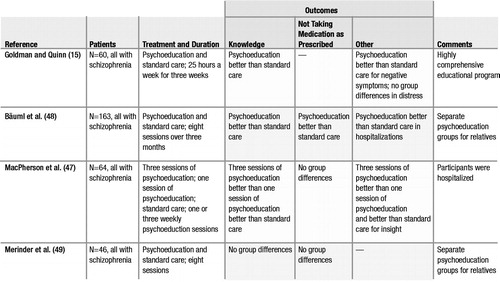 |
Table 1. Randomized Controlled Trials of Broad-Based Psychoeducation Programs
 |
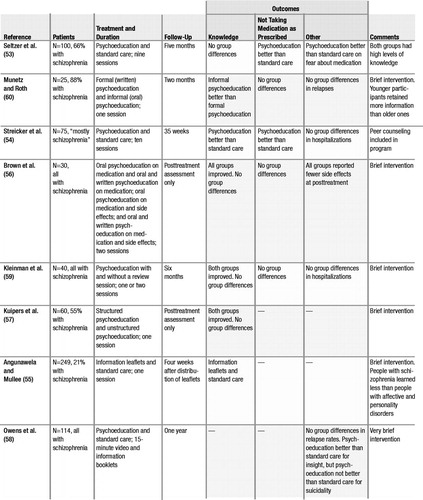 |
Table 2. Randomized Controlled Trials of Psychoeducation Programs Focused on Medication
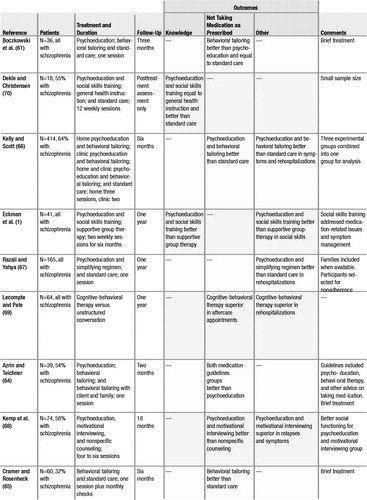 |
Table 3. Randomized Controlled Trials of Cognitive-Behavioral Programs Focused on Medication
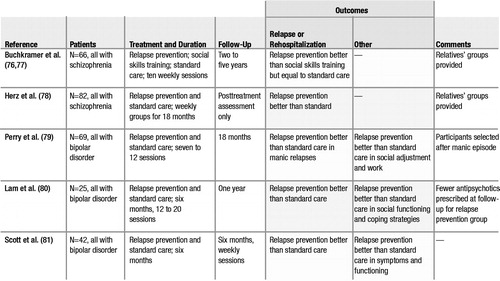 |
Table 4. Randomized Controlled Trials of Relapse Prevention Programs
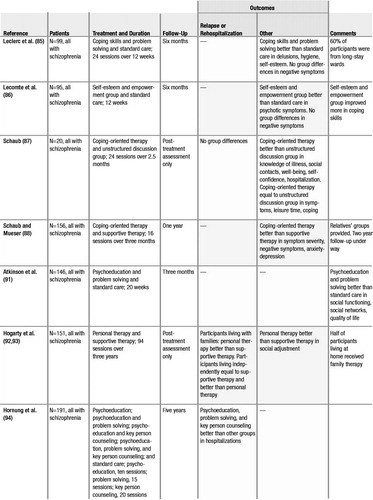 |
Table 5. Randomized Controlled Trials of Coping Skills Training and Comprehensive Programs
1 Drake RE, Goldman HH, Leff HS, et al: Implementing evidence-based practices in routine mental health service settings. Psychiatric Services 52:179–182, 2001Crossref, Google Scholar
2 Lehman AF, Steinwachs DM: Translating research into practice: the Schizophrenia Patient Outcomes Research Team (PORT) treatment recommendations. Schizophrenia Bulletin 24:1–10, 1998Crossref, Google Scholar
3 Chambless DL, Ollendick TH: Empirically supported psychological interventions: controversies and evidence. Annual Review of Psychology 52:685–716, 2001Crossref, Google Scholar
4 Weisz JR, Hawley KM, Pilkonis PA, et al: Stressing the (other) three Rs in search for empirically supported treatments: review procedures, research quality, relevance to practice, and the public interest. Clinical Psychology: Science and Practice 7:243–258, 2000Crossref, Google Scholar
5 Bond GR, Drake RE, Mueser KT, et al: Assertive community treatment for people with severe mental illness: critical ingredients and impact on clients. Disease Management and Health Outcomes 9:141–159, 2001Crossref, Google Scholar
6 Bond GR, Drake RE, Becker DR, et al: Effectiveness of psychiatric rehabilitation approaches for employment of people with severe mental illness. Journal of Disability Policy Studies 10:18–52, 1999Crossref, Google Scholar
7 Pitschel-Walz G, Leucht S, Bäuml J, et al: The effect of family interventions on relapse and rehospitalization in schizophrenia: a meta-analysis. Schizophrenia Bulletin 27:73–92, 2001Crossref, Google Scholar
8 Drake RE, Essock SM, Shaner A, et al: Implementing dual diagnosis services for clients with severe mental illness. Psychiatric Services 52:469–476, 2001Crossref, Google Scholar
9 Torrey WC, Drake RE, Dixon L, et al: Implementing evidence-based practices for persons with severe mental illnesses. Psychiatric Services 52:45–55, 2001Crossref, Google Scholar
10 Hanson RW: Physician-patient communication and compliance, in Compliance: The Dilemma of the Chronically Ill. Edited by Gerber KE, Nehemkis AM. New York, Springer, 1986Google Scholar
11 Masur FT: Adherence to health care regimens, in Medical Psychology: Contributions to Behavioral Medicine. Edited by Prokop CK, Bradley LA. New York, Academic Press, 1981Google Scholar
12 Swezey RL, Swezey AM: Educational theory as a basis for patient education. Journal of Chronic Diseases 29:417–422, 1976Crossref, Google Scholar
13 Anderson CM, Reiss DJ, Hogarty GE: Schizophrenia and the Family. New York, Guilford, 1986Google Scholar
14 Daley DC, Bowler K, Cahalane H: Approaches to patient and family education with affective disorders. Patient Education and Counseling 19:162–174, 1992Crossref, Google Scholar
15 Goldman CR, Quinn FL: Effects of a patient education program in the treatment of schizophrenia. Hospital and Community Psychiatry 39:282–286, 1988Google Scholar
16 Chamberlin J: On Our Own: Patient-Controlled Alternatives to the Mental Health System. New York, Hawthorne, 1978Google Scholar
17 Frese FJ, Davis WW: The consumer-survivor movement, recovery, and consumer professionals. Professional Psychology: Research and Practice 28:243–245, 1997Crossref, Google Scholar
18 Segal SP, Silverman C, Temkin T: Empowerment and self-help agency practice for people with mental disabilities. Social Work 38:705–712, 1993Google Scholar
19 Baxter EA, Diehl S: Emotional stages: consumers and family members recovering from the trauma of mental illness. Psychiatric Rehabilitation Journal 21:349–355, 1998Crossref, Google Scholar
20 Copeland ME: Wellness Recovery Action Plan. Brattleboro, Vt, Peach Press, 1997Google Scholar
21 Low AA: Mental Health Through Will-Training: A System of Self Help in Psychotherapy as Practiced by Recovery, Incorporated, 7th ed. Boston, Christopher Publishing House, 1957Google Scholar
22 Spaniol L, Koehler M, Hutchinson D: The Recovery Workbook: Practical Coping and Empowerment Strategies for People With Psychiatric Disability. Boston, Center for Psychiatric Rehabilitation, Sargent College of Allied Health Professions, Boston University, 1994Google Scholar
23 Anthony WA: Recovery from mental illness: the guiding vision of the mental health service system in the 1990s. Psychosocial Rehabilitation Journal 16:11–23, 1993Crossref, Google Scholar
24 Deegan P: Recovery: the lived experience of rehabilitation. Psychosocial Rehabilitation Journal 11:11–19, 1988Crossref, Google Scholar
25 Fisher DB: Humanizing the recovery process. Resources 4:5–6, 1992Google Scholar
26 Leete E: How I perceive and manage my illness. Schizophrenia Bulletin 15:197–200, 1989Crossref, Google Scholar
27 Beale V, Lambric T: The Recovery Concept: Implementation in the Mental Health System: A Report by the Community Support Program Advisory Committee. Columbus, Ohio, Department of Mental Health, Office of Consumer Services, 1995Google Scholar
28 Carling PJ: Recovery as the Core of Our Work: The Challenge to Mental Health Systems and Professionals. Presented at the New Hampshire Partners for Change Conference on Recovery held Sept 5, 1997, in Nashua, NHGoogle Scholar
29 Ralph RO: Review of Recovery Literature: A Synthesis of a Sample of Recovery Literature, 2000. Portland, Maine, University of Southern Maine, Edmund S. Muskie Institute of Public Affairs, 2000Google Scholar
30 Ralph RO: Recovery. Psychiatric Rehabilitation Skills 4:480–517, 2000Crossref, Google Scholar
31 Carpinello SE, Knight E, Markowitz F, et al: The development of the Mental Health Confidence Scale: a measure of self-efficacy in individuals diagnosed with mental disorders. Psychiatric Rehabilitation Journal 23:236–243, 2000Crossref, Google Scholar
32 Corrigan PW, Giffort D, Rashi, F, et al: Recovery as a psychological construct. Community Mental Health Journal 35:231–240, 1999Crossref, Google Scholar
33 DeMasi ME, Markowitz FE, Videka-Sherman L, et al: Specifying Dimensions of Recovery. Presented at the annual National Conference on State Mental Health Agency Services Research and Program Evaluation held Dec 8–10, 1996, in Arlington, VaGoogle Scholar
34 Ralph RO, Lambert D: Needs Assessment Survey of a Sample of AMHI Consent Decree Class Members. Portland, Maine, University of Southern Maine, Edmund S. Muskie Institute of Public Affairs, 1996Google Scholar
35 Campbell J: How consumers/survivors are evaluating the quality of psychiatric care. Evaluation Review 21:357–363, 1997Crossref, Google Scholar
36 Corrigan PW, Liberman RP, Engle JD: From noncompliance to collaboration in the treatment of schizophrenia. Hospital and Community Psychiatry 41:1203–1211, 1990Google Scholar
37 Scott A: Consumers/survivors reform the system, bringing a “human face” to research. Resources 5:3–6, 1993Google Scholar
38 Boisen AT: The Exploration of the Inner World. New York, Harper and Brothers, 1962Google Scholar
39 Dabrowski K: Positive Disintegration. Boston, Little, Brown, 1964Google Scholar
40 Miller JS: Mental illness and spiritual crisis: implications for psychiatric rehabilitation. Psychosocial Rehabilitation Journal 14:29–45, 1990Crossref, Google Scholar
41 Carpinello SE, Knight E, Jatulis LL: A Study of the Meaning of Self-Help, Self-Help Group Processes, and Outcomes. Presented at the annual meeting of the National Association of State Mental Health Program Directors (NASMHPD) held July 12–14, 1992, in Arlington, VaGoogle Scholar
42 Copeland ME: Living Without Depression and Manic Depression. Oakland, Calif, New Harbinger, 1994Google Scholar
43 Davis JM, Barter JT, Kane JM: Antipsychotic drugs, in Comprehensive Textbook of Psychiatry, vol 5. Edited by Kaplan HI, Sadock BJ. Baltimore, Williams & Wilkins, 1989Google Scholar
44 Goodwin FK, Jamison KR: Manic Depressive Illness. New York, Oxford University Press, 1990Google Scholar
45 Fenton WS, Blyler CR, Heinssen RK: Determinants of medication compliance in schizophrenia: empirical and clinical findings. Schizophrenia Bulletin 23:637–651, 1997Crossref, Google Scholar
46 Weiden PJ, Dixon L, Frances A, et al: Neuroleptic noncompliance in schizophrenia, in Advances in Neuropsychiatry and Psychopharmacology: Schizophrenia Research. Edited by Tamminga CA, Schulz SC. New York, Raven, 1991Google Scholar
47 MacPherson R, Jerrom B, Hughes A: A controlled study of education about drug treatment in schizophrenia. British Journal of Psychiatry 168:709–717, 1996Crossref, Google Scholar
48 Bäuml J, Kissling W, Pitschel-Walz G: Psychoedukative gruppen für schizophrene Patienten: Einfluss auf Wissensstand und Compliance. Nervenheilkunde 15:145–150, 1996Google Scholar
49 Merinder L-B, Viuff AG, Laugesen HD, et al: Patient and relative education in community psychiatry: a randomized controlled trial regarding its effectiveness. Social Psychiatry and Psychiatric Epidemiology 34:287–294, 1999Crossref, Google Scholar
50 Barrowclough C, Tarrier N, Watts S, et al: Assessing the functional value of relatives’ reported knowledge about schizophrenia: a preliminary study. British Journal of Psychiatry 151:1–8, 1987Crossref, Google Scholar
51 Tarrier N, Barrowclough C, Vaughn C, et al: The community management of schizophrenia: a controlled trial of a behavioural intervention with families. British Journal of Psychiatry 153:532–542, 1988Crossref, Google Scholar
52 Tarrier N, Barrowclough C: Providing information to relatives about schizophrenia: some comments. British Journal of Psychiatry 149:458–463, 1986Crossref, Google Scholar
53 Seltzer A, Roncari I, Garfinkel P: Effect of patient education on medication compliance. Canadian Journal of Psychiatry 25:638–645, 1980Crossref, Google Scholar
54 Streicker SK, Amdur M, Dincin J: Educating patients about psychiatric medications: failure to enhance compliance. Psychosocial Rehabilitation Journal 9:15–28, 1986Crossref, Google Scholar
55 Angunawela II, Mullee MA: Drug information for the mentally ill: a randomised controlled trial. International Journal of Psychiatry in Clinical Practice 2:121–127, 1998Crossref, Google Scholar
56 Brown CS, Wright RG, Christensen DB: Association between type of medication instruction and patients’ knowledge, side effects, and compliance. Hospital and Community Psychiatry 38:55–60, 1987Google Scholar
57 Kuipers J, Bell C, Davidhizar R, et al: Knowledge and attitudes of chronic mentally ill patients before and after medication education. Journal of Advanced Nursing 20:450–456, 1994Crossref, Google Scholar
58 Owens DGC, Carroll A, Fattah S, et al: A randomized, controlled trial of a brief interventional package for schizophrenic outpatients. Acta Psychiatrica Scandinavica 103:362–369, 2001Crossref, Google Scholar
59 Kleinman I, Schachter D, Jeffries J, et al: Effectiveness of two methods for informing schizophrenic patients about neuroleptic medication. Hospital and Community Psychiatry 44:1189–1191, 1993Google Scholar
60 Munetz MR, Roth LH: Informing patients about tardive dyskinesia. Archives of General Psychiatry 42:866–871, 1985Crossref, Google Scholar
61 Boczkowski J, Zeichner A, DeSanto N: Neuroleptic compliance among chronic schizophrenic outpatients: an intervention outcome report. Journal of Consulting and Clinical Psychology 53:666–671, 1985Crossref, Google Scholar
62 Miller WR, Rollnick S: Motivational Interviewing: Preparing People to Change Addictive Behavior. New York, Guilford, 1991Google Scholar
63 Eckman TA, Liberman RP, Phipps CC, et al: Teaching medication management skills to schizophrenic patients. Journal of Clinical Psychopharmacology 10:33–38, 1990Crossref, Google Scholar
64 Azrin NH, Teichner G: Evaluation of an instructional program for improving medication compliance for chronically mentally ill outpatients. Behaviour Research and Therapy 36:849–861, 1998Crossref, Google Scholar
65 Cramer JA, Rosenheck R: Enhancing medication compliance for people with serious mental illness. Journal of Nervous and Mental Disease 187:53–55, 1999Crossref, Google Scholar
66 Kelly GR, Scott JE: Medication compliance and health education among outpatients with chronic mental disorders. Medical Care 28:1181–1197, 1990Crossref, Google Scholar
67 Razali MS, Yahya H: Compliance with treatment in schizophrenia: a drug intervention program in a developing country. Acta Psychiatrica Scandinavica 91:331–335, 1995Crossref, Google Scholar
68 Kemp R, Kirov G, Everitt B, et al: Randomised controlled trial of compliance therapy: 18-month follow-up. British Journal of Psychiatry 173:271–272, 1998Google Scholar
69 Lecompte D, Pele I: A cognitive-behavioral program to improve compliance with medication in patients with schizophrenia. International Journal of Mental Health 25: 51–56, 1996Crossref, Google Scholar
70 Dekle D, Christensen L: Medication management [letter]. Hospital and Community Psychiatry 41:96–97, 1990Google Scholar
71 Eckman TA, Wirshing WC, Marder SR, et al: Technique for training schizophrenic patients in illness self-management: a controlled trial. American Journal of Psychiatry 149:1549–1555, 1992Crossref, Google Scholar
72 Saykin AJ, Gur RC, Gur RE, et al: Neuropsychological function in schizophrenia: selective impairment in memory and learning. Archives of General Psychiatry 48:618–624, 1991Crossref, Google Scholar
73 Brehm JW: A Theory of Psychological Reactance. New York, Academic Press, 1966Google Scholar
74 Sellwood W, Tarrier N: Reactance and the induction of non-compliance with antipsychotic medication: an analogue study. Manchester, England, University of Manchester, Academic Division of Clinical Psychology, 2001Google Scholar
75 Moore A, Sellwood W, Stirling J: Compliance and psychological reactance in schizophrenia. British Journal of Clinical Psychology 39:287–296, 2000Crossref, Google Scholar
76 Buchkremer G, Fiedler P: Kognitive vs. handlungsorientierte Therapie [Cognitive vs action-oriented treatment]. Nervenarzt 58:481–488, 1987Google Scholar
77 Lewandowski L, Buchkremer G, Stark M: Das Gruppenklima und die Therapeut-Patient-Baziehung bei zwei Gruppentherapiestrategien für schizophrene Patienten: ein Beitrag zur Klärung differentieller Therapieeffeckre. Psychotherapie Psychosomatik Medizinische Psychologie 44:115–121, 1994Google Scholar
78 Herz MI, Lamberti JS, Mintz J, et al: A program for relapse prevention in schizophrenia: a controlled study. Archives of General Psychiatry 57:277–283, 2000Crossref, Google Scholar
79 Perry A, Tarrier N, Morriss R, et al: Randomised controlled trial of efficacy of teaching patients with bipolar disorder to identify early symptoms of relapse and obtain treatment. British Medical Journal 318:149–153, 1999Crossref, Google Scholar
80 Lam DH, Bright J, Jones S, et al: Cognitive therapy for bipolar illness: a pilot study of relapse prevention. Cognitive Therapy and Research 24:503–520, 2000Crossref, Google Scholar
81 Scott J, Garland A, Moorhead S: A pilot study of cognitive therapy in bipolar disorders. Psychological Medicine 31:459–467, 2001Crossref, Google Scholar
82 Amador X, Strauss D, Yale S, et al: Awareness of illness in schizophrenia. Schizophrenia Bulletin 17:113–132, 1991Crossref, Google Scholar
83 Amador XF, Gorman JM: Psychopathologic domains and insight in schizophrenia. Psychiatric Clinics of North America 21:27–42, 1998Crossref, Google Scholar
84 Novacek J, Raskin R: Recognition of warning signs: a consideration for cost-effective treatment of severe mental illness. Psychiatric Services 49:376–378, 1998Crossref, Google Scholar
85 Leclerc C, Lesage AD, Ricard N, et al: Assessment of a new rehabilitative coping skills module for persons with schizophrenia. American Journal of Orthopsychiatry 70:380–388, 2000Crossref, Google Scholar
86 Lecomte T, Cyr M, Lesage AD, et al: Efficacy of a self-esteem module in the empowerment of individuals with schizophrenia. Journal of Nervous and Mental Disease 187:406–413, 1999Crossref, Google Scholar
87 Schaub A: Cognitive-behavioural copingorientated therapy for schizophrenia: a new treatment model for clinical service and research, in Cognitive Psychotherapy of Psychotic and Personality Disorders: Handbook of Theory and Practice. Edited by Perris C, McGorry PD. Chichester, England, John Wiley & Sons, 1998Google Scholar
88 Schaub A, Mueser KT, Coping-Oriented Treatment of Schizophrenia and Schizoaffective Disorder: Rationale and Preliminary Results. Presented at the annual convention of the Association for the Advancement of Behavior Therapy held Nov 16–19, 2000, in New OrleansGoogle Scholar
89 Tarrier N, Beckett R, Harwood S, et al: A trial of two cognitive behavioral methods of treating drug-resistant residual psychotic symptoms in schizophrenic patients: I. outcome. British Journal of Psychiatry 162: 524–532, 1993Crossref, Google Scholar
90 Tarrier N, Sharpe L, Beckett R, et al: A trial of two cognitive behavioural methods of treating drug-resistant residual psychotic symptoms in schizophrenia patients: II. treatment-specific changes in coping and problem-solving skills. Psychiatry and Psychiatric Epidemiology 28:5–10, 1993Crossref, Google Scholar
91 Atkinson JM, Coia DA, Gilmour WH, et al: The impact of education groups for people with schizophrenia on social functioning and quality of life. British Journal of Psychiatry 168:199–204, 1996Crossref, Google Scholar
92 Hogarty GE, Greenwald D, Ulrich RF, et al: Three year trials of personal therapy among schizophrenic patients living with or independent of family: II. effects of adjustment on patients. American Journal of Psychiatry 154:1514–1524, 1997Crossref, Google Scholar
93 Hogarty GE, Kornblith SJ, Greenwald D, et al: Three year trials of personal therapy among schizophrenic patients living with or independent of family: I. description of study and effects on relapse rates. American Journal of Psychiatry 154:1504–1513, 1997Crossref, Google Scholar
94 Hornung WP, Feldman R, Klingberg S, et al: Long-term effects of a psychoeducational psychotherapeutic intervention for schizophrenic outpatients and their key-persons: results of a five-year follow-up. European Archives of Psychiatry and Clinical Neuroscience 249:162–167, 1999Crossref, Google Scholar
95 Folkman S, Chesney M, McKusick L, et al: Translating coping theory into an intervention, in The Social Context of Coping. Edited by Eckenrode J. New York, Plenum, 1991Google Scholar
96 Lazarus RS, Folkman S: Stress, Appraisal, and Coping. New York, Springer, 1984Google Scholar
97 Beck AT: Successful outpatient psychotherapy with a schizophrenic with a delusion based on borrowed guilt. Psychiatry 15: 305–312, 1952Crossref, Google Scholar
98 Tarrier N: Management and modification of residual positive psychotic symptoms, in Innovations in the Psychological Management of Schizophrenia. Edited by Birchwood M, Tarrier, N. Chichester, England, John Wiley & Sons, 1992Google Scholar
99 Perris C: Cognitive Therapy With Schizophrenic Patients. New York, Guilford, 1989Google Scholar
100 Chadwick P, Birchwood M, Trower P: Cognitive Therapy for Delusions, Voices, and Paranoia. Chichester, England, John Wiley & Sons, 1996Google Scholar
101 Fowler D, Garety P, Kuipers E: Cognitive Behaviour Therapy for Psychosis: Theory and Practice. Chichester, England, John Wiley & Sons, 1995Google Scholar
102 Kingdon DG, Turkington D: Cognitive-Behavioral Therapy of Schizophrenia. New York, Guilford, 1994Google Scholar
103 Drury V, Birchwood M, Cochrane R, et al: Cognitive therapy and recovery from acute psychosis: a controlled trial: I. impact on psychotic symptoms. British Journal of Psychiatry 169:593–601, 1996Crossref, Google Scholar
104 Drury V, Birchwood M, Cochrane R, et al: Cognitive therapy and recovery from acute psychosis: a controlled trial: II. impact on recovery time. British Journal of Psychiatry 169:602–607, 1996Crossref, Google Scholar
105 Garety P, Fowler D, Kuipers E, et al: London–East Anglia randomised controlled trial of cognitive-behavioural therapy for psychosis: II. predictors of outcome. British Journal of Psychiatry 171:420–426, 1997Crossref, Google Scholar
106 Kuipers E, Garety P, Fowler D, et al: London –East Anglia randomised controlled trial of cognitive-behavioural therapy for psychosis: I. effects of the treatment phase. British Journal of Psychiatry 171: 319–327, 1997Crossref, Google Scholar
107 Kuipers E, Fowler D, Garety P, et al: London–East Anglia randomised controlled trial of cognitive-behavioural therapy for psychosis: III. follow-up and economic evaluation at 18 months. British Journal of Psychiatry 173:61–68, 1998Crossref, Google Scholar
108 Lewis S, Tarrier N, Haddock G, et al: Randomized Controlled Trial of Cognitive-Behaviour Therapy in Early Schizophrenia: 18-Month Outcomes. Presented at the International Conference on Psychological Treatments for Schizophrenia held Sept 6–7, 2001, in Cambridge, EnglandGoogle Scholar
109 Sensky T, Turkington D, Kingdon D, et al: A randomized controlled trial of cognitivebehavioral therapy for persistent symptoms in schizophrenia resistant to medication. Archives of General Psychiatry 57:165–172, 2000Crossref, Google Scholar
110 Tarrier N, Yusupoff L, Kinney C, et al: Randomised controlled trial of intensive cognitive behaviour therapy for patients with chronic schizophrenia. British Medical Journal 317:303–307, 1998Crossref, Google Scholar
111 Tarrier N, Wittkowski A, Kinney C, et al: Durability of the effects of cognitive-behavioural therapy in the treatment of chronic schizophrenia: 12-month follow-up. British Journal of Psychiatry 174:500–504, 1999Crossref, Google Scholar
112 Tarrier N, Kinney C, McCarthy E, et al: Two-year follow-up of cognitive-behavioral therapy and supportive counseling in the treatment of persistent symptoms in chronic schizophrenia. Journal of Consulting and Clinical Psychology 68:917–922, 2000Crossref, Google Scholar
113 Rector NA, Seeman MV, Segal ZV: Cognitive therapy for schizophrenia: treatment outcomes and follow-up effects from the Toronto Trial Study. Presented at the annual meeting of the American Psychiatric Association held May 15–20, 1999, in ChicagoGoogle Scholar
114 Pinto A, La Pia S, Mennella R, et al: Cognitive-behavioral therapy and clozapine for clients with treatment-refractory schizophrenia. Psychiatric Services 50: 901–904, 1999Crossref, Google Scholar
115 Garety PA, Fowler D, Kuipers E: Cognitive-behavioral therapy for medicationresistant symptoms. Schizophrenia Bulletin 26:73–86, 2000Crossref, Google Scholar
116 Gould RA, Mueser KT, Bolton E, et al: Cognitive therapy for psychosis in schizophrenia: a preliminary meta-analysis. Schizophrenia Research 48:335–342, 2001Crossref, Google Scholar
117 Rector NA, Beck AT: Cognitive behavioral therapy for schizophrenia: an empirical review. Journal of Nervous and Mental Disease 189:278–287, 2001Crossref, Google Scholar
118 Corrigan PW, Steiner L, McCracken SG, et al: Strategies for staff dissemination of evidence-based practices for people with serious mental illness. Psychiatric Services 52:1598–1606, 2001Crossref, Google Scholar
119 Jacobson N, Curtis L: Recovery as policy in mental health services: strategies emerging from the states. Psychiatric Rehabilitation Journal 23:333–341, 2000Crossref, Google Scholar
120 Deegan PE, Affa C: Coping With Voices: Self-Help Strategies for People Who Hear Voices That Are Distressing. Lawrence, Mass, National Empowerment Center, 1995Google Scholar
121 Baxter EA, Diehl S: Emotional stages: consumer and family members recovering from the trauma of mental illness. Psychiatric Rehabilitation Journal 21:349–355, 1998Crossref, Google Scholar



