Ask the Expert: Personality Disorder Treatment
I have been treating patients with borderline personality disorder for 25 years with a traditional psychotherapy approach, and my patients get better over time. I have read so much about dialectical behavior therapy; is it a more effective approach for these patients?
Your question is particularly important and one that many practitioners ask. Dialectical behavior therapy (DBT) is an extremely valuable treatment strategy for many patients with borderline personality disorder (BPD), and it was the first “manualized” therapy for BPD that was studied in randomized controlled trials (RCTs), demonstrating its beneficial effects for these patients (1, 2).
It is important to recognize that patients who meet DSM-IV-TR diagnostic criteria for BPD are not a single homogeneous group. The polythetic system defines the diagnostic threshold for BPD as any five of the nine criteria for BPD, which results in 256 different combinations of criteria that meet the diagnostic threshold. It is no surprise, then, that treatment studies do not support a “one size fits all” pattern. When colleagues ask me questions such as “Are you a Kernbergian, a Kohutian, or a Fonagian?” I generally reply by saying “that's the wrong question—you first need to describe the borderline patient you have in mind, and then we'll think about which treatment approach might be best for that patient.” Even then, it seems probable that a given patient might benefit from more than one type of psychotherapy, and many variables determine the type of therapy selected, such as patient preference, therapist preference (or special training), therapist availability, and the limits of insurance coverage. Plakun et al. (3) described a “Y” model of psychotherapy, emphasizing that many therapies have common core features (the stem of the “Y”) such as negotiating and maintaining a therapeutic alliance, and specific treatments have specialized features (the branches of the “Y”), such as a psychodynamic focus or a cognitive behavior focus (3).
Zanarini (4) recently reviewed psychotherapy for BPD, emphasizing that a strong RCT evidence base now exists for four types of therapy: mentalization-based therapy (MBT) (5, 6), transference-focused psychotherapy (TFP) (7), DBT, and schema-focused therapy (SFT) (8), and the good news is that all of them have been shown to be effective treatments for patients with BPD. Other forms of therapy are also being studied, such as cognitive behavior therapy (CBT) (9) and systems training for emotional predictability and problem solving (STEPPS) (10). Overall, meta-analyses have demonstrated efficacy for both cognitive behavior and psychodynamic approaches (11, 12).
In my opinion, there are key common features of these psychotherapeutic approaches to treatment of patients with BPD (Table 1). I believe that the two most important goals in treatment are 1) establishing a therapeutic alliance and 2) time. The therapeutic alliance does not imply a “warm and fuzzy” relationship. For example, Bateman and Fonagy (5, 6) stressed that the therapist needs to serve as the container for the patient's “alien self.” But the therapist must remain a steady vessel and never forget the attachment pathology that is so characteristic of patients with BPD and leads to their distrust of others and their consequent testing behavior in relationships with others (including the therapist). The second goal is time. For psychotherapy to work, it requires enough time to do so. I compare it to learning a second language, which activates brain systems involved in long-term learning and memory, with the potential to change the brain. A few drop-in sessions won't suffice!
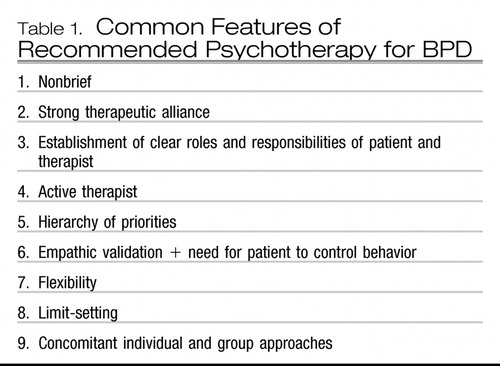 |
Table 1. Common Features of Recommended Psychotherapy for BPD
So to return to the question, I do not believe that DBT represents the only effective type of psychotherapy for BPD, although it is a very good one. Many therapists use a mix of cognitive and psychodynamic approaches, or they use different approaches at different stages of treatment. Adhering to a manualized approach may help therapists keep a good grip on the therapeutic rudder early in their career, and, if so, that's fine, because steering the boat to reach calm waters and dry land is essential!
1. Linehan MM, Heard HL, Armstrong HE: Naturalistic follow-up of a behavioral treatment for chronically parasuicidal borderline patients. Arch Gen Psychiatry 1993; 50:971–974 Crossref, Google Scholar
2. Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, Korslund KE, Tutek DA, Reynolds SK, Lindenboim N: Two-year randomized trial + follow-up of dialectical behavior therapy vs. therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry 2006; 63:757–766 Crossref, Google Scholar
3. Plakun EM, Sudak DM, Goldberg D: The Y model: an integrated, evidence-based approach to teaching psychotherapy competencies. J Psychiatr Pract 2009; 15:5–11 Crossref, Google Scholar
4. Zanarini MC: Psychotherapy of borderline personality disorder. Acta Psychiatr Scand 2009; 120:373–377 Crossref, Google Scholar
5. Bateman A, Fonagy P: Treatment of borderline personality disorder with psychoanalytically oriented partial hospitalization: an 18-month follow-up. Am J Psychiatry 2001; 158:36–42 Crossref, Google Scholar
6. Bateman A, Fonagy P: 8-Year follow-up of patients treated for borderline personality disorder: mentalization-based treatment versus treatment as usual. Am J Psychiatry 2008; 165:631–638 Crossref, Google Scholar
7. Clarkin JF, Levy KN, Lenzenweger MF, Kernberg OF: Evaluating three treatments for borderline personality disorder: a multiwave study. Am J Psychiatry 2007; 164:922–928 Crossref, Google Scholar
8. Giesen-Bloo J, van Dyck R, Spinhoven P, Spinhoven P, van Tilburg W, Dirksen C, van Asselt T, Kremers I, Nadort M, Arntz A: Outpatient psychotherapy for borderline personality disorder: randomized trial of schema-focused therapy vs transference-focused psychotherapy. Arch Gen Psychiatry 2006; 63:649–658 Crossref, Google Scholar
9. Davidson K, Norrie J, Tyrer P, Gumley A, Tata P, Murray H, Palmer S: The effectiveness of cognitive behavior therapy for borderline personality disorder: results from the Borderline Personality Disorder Study of Cognitive Therapy (BOSCOT) trial. J Pers Disord 2006; 20:450–465 Crossref, Google Scholar
10. Blum N, St. John D, Pfohl B, Stuart S, McCormick B, Allen J, Arndt S, Black DW: Systems training for emotional predictability and problem solving (STEPPS) for outpatients with borderline personality disorder: a randomized controlled trial and 1-year follow-up. Am J Psychiatry 2008;165:468–478 Crossref, Google Scholar
11. Leichsenring F, Leibing E: The effectiveness of psychodynamic therapy and cognitive behavior therapy in the treatment of personality disorders: a meta-analysis. Am J Psychiatry 2003; 160:1223–1232 Crossref, Google Scholar
12. Leichsenring F, Rabung S: Effectiveness of long-term psychodynamic psychotherapy: a meta-analysis. JAMA 2008; 300:1551–1565 Crossref, Google Scholar



