Practice Parameter for the Assessment and Treatment of Children and Adolescents With Substance Use Disorders
Abstract
This practice parameter describes the assessment and treatment of children and adolescents with substance use disorders and is based on scientific evidence and clinical consensus regarding diagnosis and effective treatment as well as on the current state of clinical practice. This parameter considers risk factors for substance use and related problems, normative use of substances by adolescents, the comorbidity of substance use disorders with other psychiatric disorders, and treatment settings and modalities.
(Reprinted with permission from the Journal of the American Academy of Child and Adolescent Psychiatry 2005; 44(6):609–621)
Alcohol and drug use is a common behavior among adolescents in the United States and other developed countries. A significant number of adolescents manifest problems with their substance use and may meet diagnostic criteria for a substance use disorder (SUD). The treatment of adolescent SUDs has begun to reflect the multifaceted nature of antecedents that lead to SUDs. These multiple problems need to be targeted for effective treatment. An empirical literature of treatment research for adolescents is emerging and provides clinicians with models and guidance for intervention with this often-difficult population.
METHODOLOGY
The list of references for this parameter was developed by searching PsycINFO, Medline, and Psychological Abstracts, by reviewing the bibliographies of book chapters and review articles; by asking colleagues for suggested source materials; and from the previous version of this parameter. The searches conducted in March 2003 used the following text words: substance abuse, adolescents, and treatment. The search covered the period 1990 to 2003 and yielded about 400 articles. Each of these references was reviewed, and only the most relevant or representative were included in this document.
DEFINITIONS
In this parameter, the term adolescents refers to older children and adolescents. Parent refers to a parent or legal guardian. The terminology in this practice parameter is consistent with that of the Diagnostic and Statistical Manual of Mental Disorders, 4th edition, text revision (DSM-IV-TR) (American Psychiatric Association, 2001). The term substance use disorders encompasses both substance abuse and substance dependence under the DSM-IV-TR category of substance-related disorders. SUDs are defined for alcohol, amphetamine (or amphetamine-like), caffeine, cannabis, cocaine, hallucinogens, inhalants, nicotine, opioids, phencyclidine (or phencyclidine-like), and sedative, hypnotic, or anxiolytic agents.
Although the DSM-IV-TR diagnoses of substance abuse and substance dependence assist clinicians in identifying adolescents with pathological patterns of substance use, the DSM-IV-TR criteria, developed for adults, have not been established as applicable to adolescents (Martin and Winters, 1998). While DSM-IV-TR remains the guide for determining substance use-related pathology in adolescents, it is important to recognize the frequent differences between the most common manifestations of the diagnoses of substance abuse and dependence in adolescents versus adults. While substance use is a necessary prelude to abuse or dependence and early onset of regular use further increases the risk of SUDs, substance use per se is not sufficient for a diagnosis of abuse or dependence.
The diagnosis of substance abuse requires evidence of a maladaptive pattern of substance use with clinically significant levels of impairment or distress. Impairment means an inability to meet major role obligations leading to reduced functioning in one or more major areas of life, risk-taking behavior, an increase in the likelihood of legal problems due to possession, and exposure to hazardous situations. Substance dependence requires a substantial degree of involvement with a substance as evidenced by the adolescent's meeting at least three criteria from a group of seven criteria such as withdrawal, tolerance, and loss of control over use.
CLINICAL PRESENTATION
Despite similarities to adults in physical size and abilities, most adolescents have not obtained mature levels of cognitive, emotional, social, or physical growth. They are challenged by the developmental tasks of forming a separate identity and preparing for appropriate societal and individual roles including job, marriage, and family. Within a developmental context, adolescents experiment with a wide range of attitudes and behaviors including the use of psychoactive substances. Most adolescents experiment with using substances such as alcohol and cigarettes, and a portion of them later advance to the use of marijuana; a smaller portion proceed to the use of other drugs (Kandel, 2002). The early onset of substance use and a more rapid progression through the stages of substance use are among the risk factors for the development of SUDs (Robins and McEvoy, 1990).
Youths who present with substance use and frequent intoxication often manifest significant levels of acute change in mood, cognition, and behavior (Bukstein and Tarter, in press). Behavioral changes may include disinhibition, lethargy, hyperactivity or agitation, somnolence, and hypervigilance. Changes in cognition may include impaired concentration, changes in attention span, and perceptual and overt disturbances in thinking such as delusions. Mood changes can range from depression to euphoria. The manifestations of substance use and intoxication vary with the type of substance(s) used, the amount used during a given time period, the setting and context of use, and a host of characteristics of the individual such as experience with the substance, expectations of drug effect, and the presence or absence of other psychopathology.
A hallmark of SUDs in adolescents is impairment in psychosocial and academic functioning (Martin and Winters, 1998). Impairment can include family conflict or dysfunction, interpersonal conflict, and academic failure. Associated characteristics include deviant and risk-taking behavior and comorbid psychiatric disorders such as conduct disorder, attention-deficit/hyperactivity disorder (ADHD), and mood, anxiety, and learning disorders (Bukstein et al., 1989; King et al., 2000; Lewinsohn et al., 1993). Almost all psychoactive substances, including those available to adults such as alcohol and nicotine, are illegal for adolescents to obtain, possess, and use. Some of the negative consequences of substance use for adolescents follow from the illegal nature of these substances rather than from their actual use.
The course of SUDs in adolescents is variable (Jaffe and Simkin, 2002; Jaffe and Solhkhah, 2004). Adolescents with abuse often decrease or discontinue use in late adolescence or early adulthood, while those with dependence and more risk factors are more likely to continue to meet criteria for one or more SUDs.
EPIDEMIOLOGY
Although the use of many substances among adolescents has declined substantially in recent years, substances such as opiates, LSD, inhalants, and steroids have shown periodic increases among youths in the past several decades (University of Michigan, 2003). In community studies, the lifetime diagnosis of alcohol abuse ranged from 0.4% in the Great Smoky Mountain Study (Costello et al., 1996) to 9.6% in the National Comorbidity Study (Kessler et al., 1994). The lifetime diagnosis of alcohol dependence ranged from 0.6% (Costello et al., 1996) to 4.3% in the Oregon Adolescent Depression Project (Lewinsohn et al., 1996). The lifetime prevalence of drug abuse or dependence has ranged from 3.3% in 15-year-olds to 9.8% in 17- to 19-year-olds (Kashani et al., 1987; Reinherz et al., 1993). It is notable that the age at which experimentation begins has been gradually declining, especially for inhalants.
RISK FACTORS
The literature on the development of substance use and SUDs in adolescents has identified an assortment of individual, peer, family, and community risk factors (Brook et al., 1989; Newcomb, 1997). These risk factors reflect both genetic and environmental influences (Kendler et al., 1999; Weinberg et al., 1998). Put in a developmental context, genetic predispositions to affective, cognitive, and behavioral dysregulation and other temperamental deviations are exacerbated by family and peer factors and the developmental issues of puberty leading to substance use and pathological use (Dawes et al., 2000; Tarter et al., 1999). Psychopathology, especially in the form of early onset of disruptive behavior disorders and mood and anxiety disorders, may be associated with the etiology of SUDs (Armstrong and Costello, 2002; Loeber, 1988).
Developmental factors that contribute to early use or to continuing use include common adolescent feelings of being invulnerable, issues of autonomy, and peer influences or “peer pressure.” Emerging evidence suggests that childhood sexual abuse and other traumatic life events may be risk factors for later SUDs (Kendler et al., 2000). Children and preadolescents are particularly susceptible to cultural factors such as media promotion of substance use, which may influence the initial use of such gateway substances as tobacco (Resnik, 1990; Saffer, 2002).
PREVENTION
Most prevention efforts are based on various theoretical models of adolescent substance use/abuse development. Research has established a number of empirically based prevention interventions that primarily involve strengthening resilience factors and reducing risk factors for the development of SUDs (National Institute on Drug Abuse, 2003). Early intervention for psychopathology in youths at risk of SUDs is critical to prevent early-onset substance use and SUDs.
RECOMMENDATIONS
Each recommendation in this parameter is identified as falling into one of the following categories of endorsement, indicated by an abbreviation in brackets following the statement. These categories indicate the degree of importance or certainty of each recommendation.
[MS] Minimal standards are recommendations that are based on substantial empirical evidence (such as wellcontrolled, double-blind trials) or overwhelming clinical consensus. Minimal standards are expected to apply more than 95% of the time, i.e., in almost all cases. When the practitioner does not follow this standard in a particular case, the medical record should indicate the reason.
[CG] Clinical guidelines are recommendations that are based on empirical evidence (such as open trials, case studies) and/or strong clinical consensus. Clinical guidelines apply approximately 75% of the time. These practices should always be considered by the clinician, but there are exceptions to their application.
[OP] Options are practices that are acceptable but not required. There may be insufficient empirical evidence to support recommending these practices as minimal standards or clinical guidelines. In some cases, they may be the perfect thing to do, but in other cases, they should be avoided. If possible, the practice parameter will explain the pros and cons of these options.
[NE] Not endorsed refers to practices that are known to be ineffective or contraindicated.
The recommendations of this parameter are based on a thorough review of the literature as well as clinical consensus. The following coding system is used to indicate the nature of the research that supports the recommendations.
[rdb] Randomized, double-blind clinical trial is a study of an intervention in which subjects are randomly assigned to either treatment or control groups and both subjects and investigators are blind to the assignments.
[rct] Randomized clinical trial is a study of an intervention in which subjects are randomly assigned to either treatment or control groups.
[ct] Clinical trial is a prospective study in which an intervention is made and the results are followed longitudinally.
CONFIDENTIALITY
Recommendation 1. The clinician should observe an appropriate level of confidentiality for the adolescent during the assessment and treatment [MS]
Adolescents are more likely to provide truthful information if they believe that their information, at least detailed information, will not be shared. Before the adolescent interview, the clinician should review exactly what information the clinician is obliged to share and with whom. Although it is obvious to the clinician that a court-ordered evaluation means a full report to the judge or probation officer, the adolescent may not be aware of this. The clinician should explicitly inform the adolescent of this requirement. Typically, a clinician should inform the adolescent that a threat of danger to self or others will force the clinician to inform a responsible adult, usually the parents. The clinician should be knowledgeable about local and federal laws that limit what information may be released. Most states have confidentiality laws that restrict the information that the clinician is allowed to share with anyone unless the adolescent provides consent. This includes information about deviant behavior such as selling drugs, who sells the adolescent drugs, and peer behaviors. The clinician should encourage and support the adolescent's revealing the extent of substance use and other problems to parents. In other cases, the clinician should discuss what information that the adolescent will allow the clinician to reveal such as a general recommendation for treatment or impressions rather than a detailed report of specific deviant and substance use behaviors.
SCREENING
Recommendation 2. The mental health assessment of older children and adolescents requires screening questions about the use of alcohol and other substances of abuse [MS]
In the face of problems in one or more domains of adolescent functioning, clinicians and educational professionals who work with youths often need to screen for the need for more comprehensive evaluation. At the very least, screening involves asking about substance use. Asking about quantity and frequency, the presence of adverse consequences of use, and the adolescent's attitude toward use are basic lines of screening inquiry. Several examples of screening instruments with established psychometric properties are listed in Table 1.
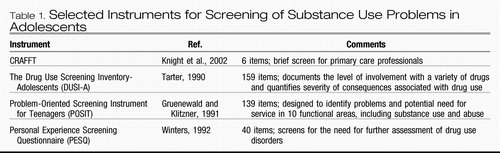 |
Table 1. Selected Instruments for Screening of Substance Use Problems in Adolescents
EVALUATION
Recommendation 3. If the screening raises concerns about substance use, the clinician should conduct a more formal evaluation to determine the quantity and frequency of use and consequences of use for each substance used and whether the youth meets criteria for SUD(s) [MS]
The goal of the evaluation is to determine whether the adolescent is using one or more substances, what effects substance use has on various domains of the adolescent's psychosocial functioning, and whether the problem fits diagnostic criteria for substance abuse or dependence. To be considered a disorder, substance use must produce some level of dysfunction in one or more domains of the adolescent's life. These include psychiatric/behavioral, family, school/vocational, recreational/leisure, and medical domains (Rahdert, 1991; Tarter, 1990). Because of the covert nature of substance use, optimal assessment often requires information from a variety of sources including the adolescent, parents (or other caregivers), other family members, school, any involved social agencies, and previous treatment records.
The attitude of the clinician should be nonjudgmental and flexible regarding the order of the interview elements to ensure a valid report of substance use and associated problems.
The parent should be able to provide information about a family history of SUDs and other psychiatric disorders, family functioning, stressors and supports, and community resources and risks.
Detailed assessment of the adolescent's substance use behavior is an essential element of the interview. Inquiry into patterns of use should include information about the age at onset and progression of use for specific substances; circumstances, frequency, and variability of use; and the types of agents used. The clinician should ask about both direct and indirect consequences of use in the domains of family, school/vocational, social, and psychological functioning and medical problems. The interviewer should also inquire about the context of use, which pertains to the adolescent's view of substance use; the adolescent's expectancies of use; the usual times and places of substance use; peer attitudes and use patterns; common behavioral or emotional antecedents and consequences of use; and the adolescent's overall social milieu. Such an inquiry can take the form of a functional analysis, considering both antecedents and consequences of the substance use behaviors. Finally, the clinician should ask about the adolescent's view of his or her substance use as a potential problem, document past or current attempts to control or stop substance use, and review the criteria for substance abuse and dependence (substance specific). Evaluating the adolescent's readiness for treatment or stage of change may help determine the initial treatment goals or level of care.
The differential diagnosis of adolescent SUDs requires consideration that the reported domains of dysfunction attributed to substance use may actually be due to premorbid or concurrent problems such as disruptive behavior disorders, family issues, or academic problems. The frequent comorbidity of SUDs and other psychiatric disorders necessitates a comprehensive review of past and present psychopathology including a review of psychiatric symptoms and treatment history. Riggs and Davies (2002) suggest a timeline approach to sort out the relationship between comorbid psychopathology, substance use, and developmental events and to assist in formulating a differential diagnosis and comprehensive treatment plan.
The interview with the adolescent also includes elements common to all assessments of emotional and behavioral problems of adolescents (American Academy of Child and Adolescent Psychiatry, 1997). A comprehensive developmental, social, and medical history is a part of any complete assessment involving adolescents (Winters, 2001). Particularly important is a review of human immunodeficiency virus risk factors including sexual and other high-risk behaviors. Clinicians may use a variety of structured interviews and rating scales with established psychometric properties to supplement interview information (see Table 2 for examples).
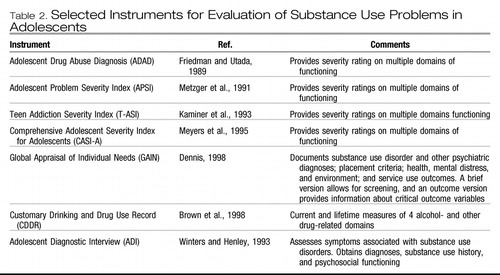 |
Table 2. Selected Instruments for Evaluation of Substance Use Problems in Adolescents
Recommendation 4. Toxicology, through the collection of bodily fluids or specimens, should be a routine part of the formal evaluation and ongoing assessment of substance use both during and after treatment [MS]
Toxicological tests of bodily fluids, usually urine but also blood, and hair samples to detect the presence of specific substances should be part of the formal evaluation and the ongoing assessment of substance use (Table 3). The optimal use of urine screening requires proper collection techniques including visualization of obtaining the sample, evaluation of positive results, and a specific plan of action should the specimen be positive for the presence of substance(s) (Casavant, 2002; Cole, 1997). The clinician should establish rules regarding the confidentiality of the results before testing. Because of the limited time that a drug will remain in the urine and possible adulteration, a negative result of urine testing does not indicate that the youth does not use drugs.
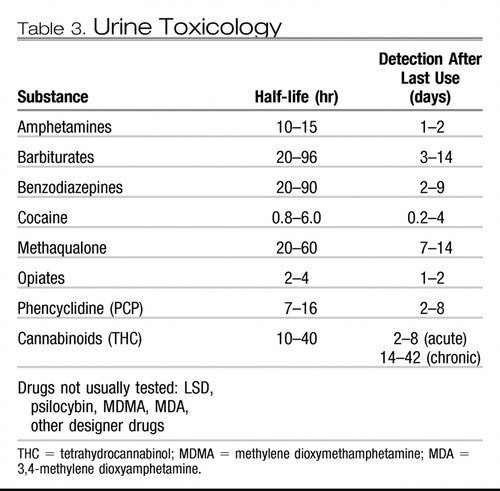 |
Table 3. Urine Toxicology
TREATMENT
Recommendation 5. Adolescents with SUDs should receive specific treatment for their substance use [MS]
Reviews of the literature on adolescent treatment outcome have concluded that treatment is better than no treatment (Deas and Thomas, 2001; Williams and Chang, 2000). In the year after treatment, patients reported decreased heavy drinking, marijuana and other illicit drug use, and criminal involvement as well as improved psychological adjustment and school performance (Grella et al., 2001; Hser et al., 2001). Longer duration of treatment is associated with several favorable outcomes. Pretreatment factors associated with poorer outcomes (usually substance use and relapse to use) are nonwhite race, increased seriousness of substance use, criminality, and lower educational status. The intreatment factors predictive of outcome are time in treatment, involvement of family, use of practical problem solving, and provision of comprehensive services such as housing, academic assistance, and recreation. Posttreatment variables that are thought to be the most important determinants of outcome include association with nonusing peers and involvement in leisure time activities, work, and school. Variables reported to be most consistently related to successful outcome are treatment completion, low pretreatment use, and peer and parent social support and nonuse of substances.
In terms of empirical support for specific treatment modalities, family therapy approaches have the most supporting evidence (Stanton and Shadish, 1997; Williams and Chang, 2000), although individual approaches such as cognitive-behavioral therapy (CBT), both alone and with motivational enhancement, have shown to be efficacious (Azrin et al., 2001 [rct]; Dennis et al., 2004 [rct]; Kaminer et al., 1998b, 1999 [rct]; Waldron et al., 2001 [rct]). Community reinforcement approaches using contingency contracting and vouchers also appear to be promising (Azrin et al., 1994 [ct]; Corby et al., 2000 [ct]; Godley et al., 2002 [rct]; Kaminer, 2000). Selfsupport groups can be encouraged as adjuncts to these treatment modalities.
The primary goal of the treatment of adolescents with SUDs is achieving and maintaining abstinence from substance use. While abstinence should remain the explicit, long-term goal of treatment, a realistic view recognizes both the chronicity of SUDs in some populations of adolescents and the self-limited nature of substance use and substance use-related problems in others. Given these considerations, harm reduction may be an interim, implicit goal of treatment. Included in the concept of harm reduction is a reduction in the use and adverse effects of substances, a reduction in the severity and frequency of relapses, and improvement in one or more domains of the adolescent's functioning (e.g., academic performance or family functioning). While adolescents may not be initially motivated to stop substance use, the attainment of skills to deal with substance use may provide the adolescent with greater self-efficacy to not only reduce use but also ultimately move toward the goal of abstinence. Although harm reduction may be an interim goal of treatment, “controlled use” of any nonprescribed substance of abuse should never be an explicit goal in the treatment of adolescents. Control of substance use should not be the only goal of treatment. A broad concept of rehabilitation involves targeting associated problems and domains of functioning for treatment. Integrated interventions that concurrently deal with coexisting psychiatric and behavioral problems, family functioning, peer and interpersonal relationships, and academic/vocational functioning not only will produce general improvements in psychosocial functioning but most likely will yield improved outcomes in the primary treatment goal of achieving and maintaining abstinence.
Ongoing assessment of outcomes is important. The critical variables regarding current substance use are the use of specific substances during and after treatment with reference to the number of days of use per month, average amount per occasion, and maximum amount per occasion. Assessment of outcomes may also include determining the youth's compliance with treatment and involvement in 12-step programs.
Based on the combination of empirical research and current clinical consensus, the clinician dealing with adolescents with SUDs should develop a treatment plan that uses modalities that target (1) motivation and engagement; (2) family involvement to improve supervision, monitoring, and communication between parents and adolescent; (3) improved problem solving, social skills, and relapse prevention; (4) comorbid psychiatric disorders through psychosocial and/or medication treatments; (5) social ecology in terms of increasing prosocial behaviors, peer relationships, and academic functioning; and (6) adequate duration of treatment and follow-up care.
Recommendation 6. Adolescents with SUDs should be treated in the least restrictive setting that is safe and effective [MS]
Treatment of adolescents with SUDs can take place at one of several levels of care, reflecting intensity of treatment and restriction of movement (American Academy of Child and Adolescent Psychiatry, 2001). Factors affecting the choice of treatment setting include the following: (1) the need to provide a safe environment and the ability of the adolescent to care for him- or herself; (2) motivation and willingness of the adolescent and his or her family to cooperate with treatment; (3) the adolescent's need for structure and limit-setting that cannot be provided in a less restrictive environment; (4) the existence of additional medical or psychiatric conditions; (5) the availability of specific types of treatment settings for adolescents; (6) the adolescent's and his or her family's preferences for a particular setting; and (7) treatment failure in a less restrictive setting or level of care. Although residential programs, including therapeutic communities (Jainchill et al., 2000), have a place in the range of setting options, community intervention settings, if feasible, may offer optimal generalization of treatment gains. Even in the community, alternative sites such as home and school are being increasingly used (Brown, 2001; Wagner and Waldron, 2001).
Recommendation 7. Family therapy or significant family/parental involvement in treatment should be a component of treatment of SUDs [MS]
Family interventions are critical to the success of any treatment approach for adolescents with SUDs (Stanton and Shadish, 1997; Waldron, 1997) because a number of family-related factors, such as parental substance use or abuse, poor parent-child relationships, low perceived parental support, poor communication, and poor parent supervision and management of the adolescent's behavior, have been identified as risk factors for the development of substance abuse among adolescents. Three domains of predictors that have figured prominently in longitudinal studies of the etiology of adolescent substance use and SUDs are particularly relevant: characteristics of the parent-child relationship; parental effectiveness; and parental SUDs. Conflict between parents and adolescents, insufficient parental monitoring, inconsistent or otherwise ineffective discipline, child abuse/neglect, and parental alcoholism or other substance abuse have all been found to be robust correlates and predictors of adolescent substance use and SUDs (Hawkins et al., 1992).
Although there are many approaches to family intervention for substance abuse treatment, they have common goals: providing psychoeducation about SUDs, which decreases familial resistance to treatment and increases motivation and engagement; assisting parents and family to initiate and maintain efforts to get the adolescent into appropriate treatment and achieve abstinence; assisting parents and family to establish or reestablish structure with consistent limit-setting and careful monitoring of the adolescent's activities and behavior; improving communication among family members; and getting other family members into treatment and/or support programs.
Family therapy is the most studied modality in the treatment of adolescents with SUDs. Based on the limited number of comparative studies, outpatient family therapy appears to be superior to other forms of outpatient treatment (Deas and Thomas, 2001; Waldron, 1997; Williams and Chang, 2000). Among the forms of family therapy having support based on controlled studies are functional family therapy (Alexander et al., 1990 [rct]; Friedman, 1989 [rct]), brief strategic family therapy (Szapocznik et al., 1983 [rct], 1988 [rct]), multisystemic therapy (Henggeler et al., 1991 [rct], 2002 [rct]), family systems therapy (Joanning et al., 1992 [rct]), and multidimensional family therapy (Dennis et al., 2002 [rct]; Liddle et al., 2001 [rct]). An integrated behavioral and family therapy model that combines a family systems model and CBT also appears efficacious (Waldron et al., 2001 [rct]).
Despite the importance of family interventions, treatment can be effective without participation of the adolescent (Dennis et al., 2004; Waldron et al., 2001). Similarly, interventions with the adolescent alone (e.g., CBT or CBT plus Motivational Enhancement Therapy [MET]) are also effective (Dennis et al., 2004; Kaminer and Burleson, 1999; Kaminer et al., 1998).
Recommendation 8. Treatment programs and interventions should develop procedures to minimize treatment dropout and to maximize motivation, compliance, and treatment completion [CG]
Treatment completion is the treatment variable most consistently related to positive outcome (Alford et al., 1991; Hser et al., 2001; Williams and Chang, 2000). Related variables are motivation and compliance, which are also related to better outcomes (Cady et al., 1996). Adolescent perceptions can also contribute to whether the youth will be engaged in treatment; this suggests that specialized, adolescent-focused engagement interventions are necessary.
Modifications of motivational interviewing or enhancement techniques for adolescents have shown promise for both evaluation and treatment based on limited treatment studies (Colby et al., 1998 [rct]; Monti et al., 1999 [rct], 2001). This nonjudgmental, nondirective strategy is designed to move the adolescent to a “stage of change” in which the youth is more receptive to treatment or behavior change. Motivational interviewing and other brief interventions may serve to heighten motivation, increase self-efficacy, and provide personalized feedback and education tailored to specific substances and comorbid problems such as psychiatric disorders.
Specific engagement procedures have been incorporated as part of many family-based interventions (Dakof et al., 2001 [rct]; Diamond et al., 1999; Santisteban et al., 1996 [rct]; Szapocznik et al., 1988 [rct]; Waldron, 1997 [rct]; Waldron et al., 2001 [rct]). Other family-based treatments such as multidimensional family therapy (Rowe et al., 2002) and multisystemic therapy (Henggeler et al., 1996; Randall et al., 2001) also have strong engagement goals and components.
Recommendation 9. Medication can be used when indicated for the management of craving and withdrawal and for aversion therapy [OP]
Medications used to target alcohol-related cravings (e.g., naltrexone, acamprosate, ondansetron) are increasingly used among adults and have been effective in case reports in adolescents (Solhkhah and Wilens, 1998). Their efficacy in adolescents has yet to be tested in controlled trials. These and aversive agents such as disulfiram could be considered for use in treatment-resistant adolescents.
Similarly, the use of medications to treat alcohol, benzodiazepine, or opiate withdrawal using medications, such as benzodiazepines (alcohol) and clonidine and buprenorphine (opiates), is not based on empirical research in adolescents but rather on research and experience with adults. Clinicians should use caution in considering pharmacological treatment for adolescents with comorbid SUDs and psychiatric disorders. The presence of SUDs or substance use may increase the potential for intentional or unintentional overdose with some psychotropic medications, especially in combination with some substances of abuse.
Recommendation 10. Treatment should encourage and develop peer support, especially regarding the nonuse of substances [CG]
Having a supportive environment, especially parents and peers who do not use substances, is important for optimal outcomes (Brown et al., 2001; Myers et al., 1995).
A controversial element of traditional treatment programs is the widespread use of group treatment. There is substantial evidence that group treatment can have significant negative effects on outcomes (Dishion et al., 2001). Emerging data suggest that this iatrogenic effect may be limited to more deviant, conduct-disordered youths who nevertheless make up a substantial portion of the adolescent SUD treatment population. Other studies show positive effects for group modalities (Dennis et al., 2002 [rct]; Kaminer and Burleson, 1999 [rct]; Waldron et al., 2001 [rct]). Clinicians should take caution when forming groups for treatment and should consider alternative family-based or other modalities for more deviant youths.
Recommendation 11. Twelve-step approaches may be used as a basis for treatment. Attendance at Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) groups is an adjunct to professional treatment of SUDs and should be encouraged [CG]
Twelve-step approaches, using AA and NA as a basis for treatment, are perhaps the most common approaches for treatment and treatment programs in the United States. Attendance in aftercare treatment or self-support groups (e.g., AA or NA) is related to positive outcomes in several studies of adolescent SUD treatment (Alford et al., 1991; Williams and Chang, 2000; Winters et al., 2000). Several other studies have found that attendance at self-support or aftercare groups is associated with higher rates of abstinence and other measures of improved outcome, when compared with those not participating in such groups after treatment (Brown et al., 1994).
Twelve-step programs can be defined as having adolescents work on specific steps toward recovery, attendance at self-support groups (AA or NA), and obtaining the assistance of a sponsor who is another person in recovery from substance use problems. Developmentally appropriate, specific 12-step programs and self-support groups offer several benefits including a recovering (i.e., nonsubstance-using) peer group, available sponsors, and other types of support (Jaffe, 1990, 2001). Although 12-step programs may be effective for many adolescents, they have not been subject to controlled clinical trials.
Recommendation 12. Programs/interventions should attempt to provide comprehensive services in other domains (e.g., vocational, recreational, medical, family, and legal) [CG]
Programs with more comprehensive services such as vocational counseling, recreational activities, and medical services (including birth control) have better outcomes than programs without those services (Hser et al., 1999; Williams and Chang, 2000). Per the success of multisystemic therapy, programs that deal with the social ecology or total life circumstances of the adolescent are likely to produce more lasting benefits than those that do not.
COMORBIDITY
Recommendation 13. Adolescents with SUDs should receive thorough evaluation for comorbid psychiatric disorders [MS]
Significant rates of adolescents with coexisting SUDs and psychiatric disorders (disruptive behavior disorders, mood disorders, and anxiety disorders) are reported in both clinical and general populations (Armstrong and Costello, 2002; Grella et al., 2001; Lewinsohn et al., 1993; Simkin, 2004). Some psychiatric disorders such as disruptive behavior disorders and depressive disorders may increase the risk of the development of SUDs. Although researchers and clinicians have proposed the concept of adolescents using illicit substances as a form of self-medication for dysphoria or other psychiatric symptoms, no definitive studies are available (Bukstein and Tarter, in press). Furthermore, the comorbidity of psychiatric disorders, particularly conduct disorder and, to a lesser extent, major depressive disorder, may have an effect on substance use and related problems at both baseline and follow-up and may impair an adolescent's ability to effectively engage in treatment (Riggs and Whitmore, 1999). Evidence suggests that depression increases the rate and rapidity of relapse (Cornelius et al., 2003). When compared with youths with SUDs with no comorbidities, the 63% of youths with comorbid disorders were more likely to be alcohol or other drug dependent and have more problems with family, school, and criminal involvement; they were more likely to use marijuana and hallucinogens and engage in delinquent behavior in the 12 months after treatment (Grella et al., 2001).
Disruptive behavior disorders are the most common psychiatric disorders diagnosed in adolescents with SUDs. Conduct disorder, including the component of aggression, usually precedes and accompanies adolescent SUD (Huizinga and Elliot, 1981; Loeber, 1988). ADHD is also often present in youths with SUDs (Wilens et al., 1994). Several studies have also linked SUDs with learning disabilities and sensory processing problems in adolescents (Tapert et al., 2002).
Mood disorders, particularly depression, frequently have an onset both preceding and consequent to the onset of substance use and SUDs in adolescents (Armstrong and Costello, 2002). The prevalence of depressive disorders in these studies of clinical populations ranged from 24% to more than 50%. SUDs among adolescents are also a risk factor for suicidal behaviors, including ideation, attempts, and completed suicide (Crumley, 1990; Lewinsohn et al., 1996).
A number of studies of clinical populations show high rates of anxiety disorders, especially posttraumatic stress disorder and social phobia, among youths with SUDs, ranging from 7% to more than 40% (Clark et al., 1995; Grella et al., 2001). Bulimia nervosa is also frequently associated with adolescents having SUDs (von Ranson et al., 2002). SUDs are very common among individuals, especially the young and chronically impaired, who have a diagnosis of schizophrenia (Kutcher et al., 1992).
Recommendation 14. Comorbid conditions should be appropriately treated [MS]
It is essential to treat psychiatric disorders that are comorbid with SUDs (Physician Leadership on National Drug Policy, 2002). Although the effects of integrated mental health and SUD treatment await more empirical study, the optimal treatment of adolescents with SUDs and psychiatric comorbidity presumably involves an integration of treatment modalities rather than merely concurrent or consecutive treatment with specific modalities for either SUD or psychiatric disorder(s) (Riggs and Davies, 2002).
Many cognitive-behavioral modalities (CBT) effective with adolescents with conduct disorder also are relevant for youths with coexisting SUDs (Kazdin, 1995). CBT can include elements directed toward substance use such as relapse prevention but also generic issues such as social skills, anger control, and problem solving.
Recent emerging research and experience suggest that pharmacotherapy can be used safely and effectively in adolescents with SUDs (Bukstein and Kithas, 2002; Solhkhah and Wilens, 1998). Open trials with pemoline and bupropion for ADHD and fluoxetine for depression have shown promise (Riggs et al., 1996 [ct], 1997 [ct], 1998 [ct]; Cornelius et al., 2001 [ct]). More recently, a double-blind, placebo-controlled trial of a stimulant medication demonstrated the efficacy of medication improving ADHD symptoms in adolescents with comorbid ADHD and SUD. This study also demonstrated that medication treatment of ADHD alone, without specific SUD or other psychosocial treatment, did not decrease substance use (Riggs et al., 2004 [rdb]). Lithium, in a randomized, controlled trial (Geller et al., 1998 [rdb]), and selective serotonin reuptake inhibitors, in open trials (Cornelius et al., 2001 [ct]; Riggs et al., 1997 [ct]), have produced significant improvements in adolescents with SUDs and comorbid mood disorders.
Some commonly used pharmacological agents, such as psychostimulants and benzodiazepines, have inherent abuse potential. The risk of abuse of a therapeutic agent by the adolescent, his or her peer group, or family members should prompt a thorough assessment of the risk of this outcome (e.g., history of abuse of the agent, family/parental history of substance abuse or antisocial behavior). Often, parental or adult supervision of medication administration can alleviate concerns about potential abuse. The clinician should also consider alternative agents to psychostimulants, such as atomoxetine and bupropion, with a lower potential for abuse. The newer long-acting stimulant preparations may offer less potential for abuse or diversion due to their form of administration and the ability to more easily monitor and supervise once-daily dosing. However, their abuse potential has yet to be fully ascertained. Although many anxiety symptoms or disorders in adolescents can be treated successfully with psychosocial methods such as behavior therapy, the use of selective serotonin reuptake inhibitors, tricyclic antidepressants, or buspirone is preferred over the use of benzodiazepines.
AFTERCARE
Recommendation 15. Programs and interventions should provide or arrange for posttreatment aftercare [CG]
SUDs are often chronic disorders requiring ongoing intervention. Participation in aftercare services after treatment in a program is related to improved outcomes (Williams and Chang, 2000). Adolescents attending more intensive aftercare programs involving case management and community reinforcement were more likely than those who did not receive these services to be abstinent from marijuana and reduce their alcohol use at 3 months post-discharge (Godley et al., 2001 [rct], 2002 [rct]). After the acute treatment for substance use, ongoing attention should be paid to comorbid psychopathology and other comprehensive needs of the adolescent and his or her family. Self-support groups such as AA and NA are often an element of aftercare.
SCIENTIFIC DATA AND CLINCIAL CONSENSUS
Practice parameters are strategies for patient management, developed to assist clinicians in psychiatric decision making. American Academy of Child and Adolescent Psychiatry practice parameters, based on evaluation of the scientific literature and relevant clinical consensus, describe generally accepted approaches to assess and treat specific disorders or to perform specific medical procedures. These parameters are not intended to define the standard of care, nor should they be deemed inclusive of all proper methods of care or exclusive of other methods of care directed at obtaining the desired results. The clinician, after considering all the circumstances presented by the patient and his or her family, the diagnostic and treatment options available, and available resources, must make the ultimate judgment regarding the care of a particular patient.
This parameter was developed by Oscar G. Bukstein, M.D., and the Work Group on Quality Issues: William Bernet, M.D., and Oscar G. Bukstein, M.D., Co-Chairs, and Valerie Arnold, M.D., Joseph Beitchman, M.D., Jon Shaw, M.D., R. Scott Benson, M.D., Joan Kinlan, M.D., John McClellen, M.D., and Saundra Stock, M.D. AACAP staff: Kristin Kroeger Ptakowski.
A group of invited experts also reviewed the parameter. The Work Group on Quality Issues thanks William Arroyo, M.D., Judith Cohen, M.D., Michael A. Dawes, M.D., Deborah Deas, M.D., Mark Godley, Ph.D., Susan Godley, Ph.D., Scott Henggeler, Ph.D., Steven Jaffe, M.D., Yifrah Kaminer, M.D., Howard Liddle, Ph.D., Robert Milan, M.D., Paula D. Riggs, M.D., Cynthia Rowe, Ph.D., Deborah Simkin, M.D., Jose Szapocznik, Ph.D., and Naimah Weinberg, M.D.
This parameter was reviewed at the member forum at the 2002 annual meeting of the American Academy of Child and Adolescent Psychiatry.
During January to April 2004, a consensus group reviewed and finalized the content of this practice parameter. The consensus group consisted of representatives of relevant AACAP components as well as independent experts: William Bernet, M.D., Chair; Oscar G. Bukstein, M.D., author of the parameter; Saundra Stock, M.D., and Joseph Beitchman, M.D., representatives of the Work Group on Quality Issues; Thomas F. Anders, M.D., representative of the AACAP Council; Steven L. Jaffe, M.D., and Shashi Bhatia, M.D., representatives of the AACAP Assembly of Regional Organizations; Ramon Solhkhah, M.D., chair of the AACAP Committee on Substance Abuse and Addiction; Deborah R. Simkin, M.D., former chair of the AACAP Committee on Substance Abuse and Addictions; and Kristin Kroeger Ptakowski, Director of Clinical Affairs, AACAP.
This practice parameter was approved by AACAP Council in June 2004. This practice parameter is available on the Internet (www.aacap.org).
Alexander JF, Waldon HB, Newberry AM, Liddle N (1990), The functional family therapy model. In: Family Therapy for Adolescent Drug Abuse, Friedman AS, Granick S, eds. Lexington, MA: Lexington Books, pp 183– 200Google Scholar
Alford GS, Koehler RA, Leonard J (1991). Alcoholics anonymous-narcotics anonymous model inpatient treatment of chemically dependent adolescents: a 2-year outcome study. J Stud Alcohol 52: 118– 126Crossref, Google Scholar
American Academy of Child and Adolescent Psychiatry (1997), Practice parameters for the psychiatric assessment of children and adolescents. J Am Acad Child Adolesc Psychiatry 36: 4S– 20SCrossref, Google Scholar
American Academy of Child and Adolescent Psychiatry (2001), Child and Adolescent Level of Care Utilization System (CALOCUS) for Psychiatric and Addiction Services. Washington, DC: AACAPGoogle Scholar
American Psychiatric Association (2001), Diagnostic and Statistic Manual of Mental Disorders, 4th Edition, Text Revision (DSM-IV-TR). Washington, DC: American Psychiatric PressGoogle Scholar
Armstrong TD, Costello EJ (2002), Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. J Consult Clin Psychol 70: 1224– 1239Crossref, Google Scholar
Azrin NH, Donohue B, Besalel VA (1994). Youth drug abuse treatment: a controlled outcome study. J Child Adolesc Subst Abuse 3: 1– 16Crossref, Google Scholar
Azrin NH, Donohue B, Teichner GA, Crum T, Howell J, DeCato LA (2001), A controlled evaluation and description of individual-cognitive problem solving and family-behavior therapies in dually-diagnosed conduct-disordered and substance-dependent youth. J Child Adolesc Subst Abuse 11: 1– 43Crossref, Google Scholar
Brook JS, Nomura C, Cohen P (1989), A network of influences on adolescent drug involvement: neighborhood, school, peer, and family. Genet Soc Gen Psychol Monogr 115: 125– 145Google Scholar
Brown SA (2001), Facilitating change for adolescent alcohol problems: a multiple options approach. In: Innovations in Adolescent Substance Abuse Interventions, Wagner, EF, Waldron, HB, eds. Amsterdam: Pergamon/ Elsevier Science, pp 169– 187Crossref, Google Scholar
Brown SA, D'Amico EJ, McCarthy DM, Tapert SF (2001). Four-year outcomes from adolescent alcohol and drug treatment. J Stud Alcohol 62: 381– 388Crossref, Google Scholar
Brown SA, Myers MG, Lippke L, Tapert SF, Stewart DG, Vik PW (1998). Psychometric evaluation of the Customary Drinking and Drug Use Record (CDDR): a measure of adolescent alcohol and drug involvement. J Stud Alcohol 59: 427– 438Crossref, Google Scholar
Brown SA, Myers MG, Mott MA, Vik PW (1994), Correlates of success following treatment for adolescent substance abuse. Appl Prev Psychol 3: 61– 73Crossref, Google Scholar
Bukstein O, Kithas J (2002). Adolescent substance use disorders. In: Child Adolescent Psychopharmacology, Rosenberg D, Davanzo PA, Gershon S, eds. New York: Marcel Dekker, pp 675– 710Google Scholar
Bukstein OG, Brent DA, Kaminer Y (1989). Comorbidity of substance abuse and other psychiatric disorders in adolescents. Am J Psychiatry 146: 1131– 1141Crossref, Google Scholar
Bukstein OG, Tarter RE (in press), Substance use disorders in children and adolescents. In: Textbook of Pediatric Neuropsychiatry, 2nd ed. Coffey E, ed. New York: American Psychiatric PressGoogle Scholar
Cady ME, Winters KC, Jordan DA, Solberg KB, Stinchfield RD (1996). Motivation to change as a predictor of treatment outcome for adolescent substance abusers. J Child Adolesc Sub Abuse 5: 73– 91Crossref, Google Scholar
Casavant MJ (2002). Urine drug screening in adolescents. Pediatr Clin North Am 49: 317– 327Crossref, Google Scholar
Clark DB, Bukstein OG, Smith MG, Kaczynski N, Mezzich AC, Donovan JE (1995). Identifying anxiety disorders in adolescents hospitalized for alcohol abuse or dependence. Psychiatr Serv 46: 618– 620Crossref, Google Scholar
Colby SM, Monti P, Barnett N et al. (1998). Brief motivational interviewing in a hospital setting for adolescent smoking: a preliminary study. J Consult Clin Psychol 66: 574– 578Crossref, Google Scholar
Cole EJ (1997). New developments in biological measures of drug prevalence. In: Validity of Self-Reported Drug Use: Improving the Accuracy of Survey Estimates NIDA Research Monograph 167, Harrison L, Hughes, A, eds. Rockville, MD: NIDA, pp 108– 130Google Scholar
Corby EA, Roll JM, Ledgerwood DM, Schuster CR (2000). Contingency management interventions for treating the substance abuse of adolescents: a feasibility study. Exp Clin Psychopharmacol 8: 371– 376Crossref, Google Scholar
Cornelius JR, Bukstein OG, Birmaher B et al. (2001). Fluoxetine in adolescents with major depression and an alcohol use disorder: an open label trial. Addict Behav 26: 735– 739Crossref, Google Scholar
Cornelius JR, Maisto SA, Martin CS et al. (2003). Major depression associated with earlier alcohol relapse in treated teens with AUD. Addict Behav 28: 381– 386Crossref, Google Scholar
Costello JE, Angold A, Burns BJ et al. (1996). The smoky, mountains study of youth: goals, design, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psychiatry 53: 1129– 1136Crossref, Google Scholar
Crumley FE (1990). Substance abuse and adolescent suicidal behavior. JAMA 263: 3051– 3056Crossref, Google Scholar
Dakof GA, Tejeda M, Liddle HA (2001). Predictors of engagement in adolescent drug abuse treatment. J Am Acad Child Adolesc Psychiatry 40: 274– 281Crossref, Google Scholar
Dawes MA, Antelman SM, Vanyukov MM et al. (2000). Developmental sources of variation in liability to adolescent substance use disorders. Drug Alcohol Depend 6: 3– 14Crossref, Google Scholar
Deas D, Thomas SE (2001). An overview of controlled studies of adolescent substance abuse treatment. Am J Addict 10: 178– 189Crossref, Google Scholar
Dennis ML (1998). Global Appraisal of Individual Needs (GAIN) Manual: Administration, Scoring and Interpretation (prepared with funds from CSAT TI 11320). Bloomington, IL: Lighthouse PublicationsGoogle Scholar
Dennis N, Godley SH, Diamond G et al. (2004). The Cannabis Youth Treatment (CYT) study: main findings from two randomized trials. J Subst Abuse Treat 27: 197– 213Crossref, Google Scholar
Dennis ML, Titus JC, Diamond G et al. (2002). The Cannabis Youth Treatment (CYT) experiment: rationale, study design, and analysis plans. Addiction 97: 16– 34Crossref, Google Scholar
Diamond GM, Liddle HA, Hogue A. Dakof GA (1999). Alliance-building interventions with adolescents in family therapy: a process study. Psychother Theory Res Pract Train 36: 355– 368Crossref, Google Scholar
Dishion T, Poulin F, Burraston B (2001). Peer group dynamics associated with iatrogenic effects in group interventions with high-risk young adolescents. In: The Role of Friendship in Psychological Adjustment. New Directions for Child and Adolescent Development, No. 91, Nangle DW, Erdley CA, eds. San Francisco: Jossey-Bass, pp 79– 92Google Scholar
Friedman AS, Utada A (1989). A method for diagnosing and planning the treatment of adolescent drug abusers (the Adolescent Drug Abuse Diagnosis [ADAD] Instrument). J Drug Educ 19: 285– 312Crossref, Google Scholar
Geller B, Cooper TB, Sun K et al. (1998). Double-blind and placebocontrolled study of lithium for adolescent bipolar disorders with secondary substance dependency. J Am Acad Child Adolesc Psychiatry 37: 171– 178Crossref, Google Scholar
Godley SH, Godley M, Dennis M (2001). The assertive aftercare protocol for adolescent substance abusers. In: Innovations in Adolescent Substance Abuse Interventions, Wagner EF, Waldron HB, eds. Amsterdam: Pergamon, pp 313– 331Crossref, Google Scholar
Godley MD, Godley SH, Dennis ML, Funk R, Passetti LL (2002). Preliminary outcomes from the assertive continuing care experiment for adolescents discharged from residential treatment. J Subst Abuse Treat 23: 21– 32Crossref, Google Scholar
Grella CE, Hser Y, Joshi V, Rounds-Bryant J (2001). Drug treatment outcomes for adolescents with comorbid mental and substance use disorders. J Nerv Ment Dis 189: 384– 392Crossref, Google Scholar
Hall JA, Richardson B, Spears J, Rembert JK (1998). Validation of the POSIT: comparing drug using and abstaining youth. J Child Adolesc Subst Abuse 8: 29– 61Crossref, Google Scholar
Hawkins JD, Catalano RF, Miller JY (1992). Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood:Implications for substance abuse prevention. Psychol Bull 112: 64– 105Crossref, Google Scholar
Henggeler SW, Borduin CM, Melton GB et al. (1991). Effects of multisystemic therapy on drug use and abuse in serious juvenile offenders: a progress report from two outcome studies. Fam Dynamics Addict Q 1: 40– 51Google Scholar
Henggeler SW, Clingempeel WG, Brondino MJ, Pickrel SG (2002). Fouryear follow up of multisystemic therapy with substance abusing and substance-dependent juvenile offenders. J Am Acad Child Adolesc Psychiatry 41: 868– 874Crossref, Google Scholar
Henggeler SW, Pickrel SG, Brondino MJ, Crouch JL (1996). Eliminating (almost) treatment dropout of substance abusing or dependent delinquents through home-based multisystemic therapy. Am J Psychiatry 153: 427– 428Crossref, Google Scholar
Hser Y, Grella CE, Hubbard RL et al. (2001). An evaluation of drug treatments for adolescents in 4 US cities. Arch Gen Psychiatry 58: 689– 695Crossref, Google Scholar
Hser Y, Joshi V, Anglin MD, Fletcher B (1999). Predicting posttreatment cocaine abstinence for first-time admissions and treatment repeaters. Am J Public Health 89: 666– 671Crossref, Google Scholar
Huizinga D, Elliot DS (1981). A Longitudinal Study of Drug Use and Delinquency in a National Sample of Youth: An Assessment of Causal Order. Project Report No. 16, A National Youth Study. Boulder, CO: Behavioral Research InstituteGoogle Scholar
Jaffe SL (1990), Step Workbook for Adolescent Chemical Dependency Recovery: A Guide To The First Five Steps. American Academy of Child and Adolescent Psychiatry. Washington, DC: American Psychiatric PressGoogle Scholar
Jaffe S (2001). Adolescent Substance Abuse Intervention Workbook: Taking a First Step. Washington, DC: American Psychiatric PressGoogle Scholar
Jaffe SL, Simkin DR (2002). Alcohol and drug abuse in children and adolescents. In: Child and Adolescent Psychiatry: A Comprehensive Textbook, Lewis M, ed. Philadelphia: Lippincott Williams & Wilkins, pp 895– 911Google Scholar
Jaffe SL, Solhkhah R (2004). Substance abuse disorders. In: Textbook of Child and Adolescent Psychiatry, Wiener JM, Dulcan MK, eds. Washington, DC: American Psychiatric Press pp 795– 812Google Scholar
Jainchill N, Hawke J, De Leon G, Yagelka J (2000), Adolescents in therapeutic communities: one-year posttreatment outcomes. J Psychoactive Drugs 32: 81– 94Crossref, Google Scholar
Joanning H, Quinn W, Thomas F, Mullen R (1992), Treating adolescent drug abuse: a comparison of family system therapy, group therapy and family drug education. J Marital Fam Ther 18: 345– 356Crossref, Google Scholar
Kaminer Y (2000), Contingency management reinforcement procedures for adolescent substance abuse. J Am Acad Child Adolesc Psychiatry 39: 1324– 1326Crossref, Google Scholar
Kaminer Y, Burleson JA (1999), Psychotherapies for adolescent substance abusers: 15-month follow-up of a pilot study. Am J Addict 8: 114– 119Crossref, Google Scholar
Kaminer Y, Burleson JA, Blitz C, Sussman J, Rounsaville BJ (1998), Psychotherapies for adolescent substance abusers: a pilot study. J Nerv Ment Dis 186: 684– 690Crossref, Google Scholar
Kaminer Y, Wagner E, Plummer B, Seifer R (1993), Validation of the Teen Addiction Severity Index (T-ASI): Preliminary Findings. Am J Addict 2: 250– 254Google Scholar
Kandel D (2002), Stages and Pathways of Drug Involvement: Examining the Gateway Hypothesis. Cambridge, UK: Cambridge University PressGoogle Scholar
Kashani JH, Beck NC, Hoeper EW et al. (1987), Psychiatric disorders in a community sample of adolescents. Am J Psychiatry 144: 584– 589Crossref, Google Scholar
Kazdin AE (1995), Conduct Disorder, 2nd ed. Newbury Park, CA: SageGoogle Scholar
Kendler KS, Bulik CM, Silberg J, Hettema JM, Myers J, Prescott CA (2000), Childhood sexual abuse and adult psychiatric and substance use disorders in women: an epidemiological and cotwin control analysis. Arch Gen Psychiatry 57: 953– 959Crossref, Google Scholar
Kendler KS, Karkowski LM, Corey LA, Prescott CA, Neale MC (1999), Genetic and environmental risk factors in the etiology of illicit drug initiation and subsequent misuse in women. Br J Psychiatry 175: 351– 356Crossref, Google Scholar
Kessler RC, McGonagle KA, Zhao S et al. (1994), Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Study. Arch Gen Psychiatry 51: 8– 19Crossref, Google Scholar
King RD, Gaines LS, Lambert EW, Summerfelt WT, Bickman L (2000), The co-occurrence of psychiatric substance use diagnoses in adolescents in different service systems: frequency, recognition, cost, and outcomes. J Behav Health Serv Res 27: 417– 430Crossref, Google Scholar
Knight JR, Sherritt L, Shrier LA, Harris SK, Change G (2002), Validity of the CRAFFT substance abuse screening test among adolescent clinic patients. Arch Pediatr Adolesc Med 156: 607– 614Crossref, Google Scholar
Kutcher S, Kachur E, Marton P et al. (1992), Substance abuse among adolescents with chronic mental illnesses: a pilot study of descriptive and differentiating features. Can J Psychiatry 37: 428– 431Crossref, Google Scholar
Lewinsohn PM, Hops H, Roberts RE, Seeley JR (1993), Adolescent psychopathology: 1. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. J Abnorm Psychol 102: 133– 144Crossref, Google Scholar
Lewinsohn PM, Rohde P, Seeley JR (1996), Alcohol consumption in high school adolescents: frequency of use and dimensional structure of associated problems. Addiction 91: 375– 390Crossref, Google Scholar
Liddle HA, Dakof GA, Parker K, Diamond GS, Barrett K, Tejeda M (2001), Multidimensional family therapy for adolescent substance abuse: results of a randomized clinical trial. Am J Drug Alcohol Abuse 27: 651– 687Crossref, Google Scholar
Loeber R (1988), Natural histories of conduct problems, delinquency and associated substance use. In: Advances in Clinical Child Psychology, Volume 11, Lahey BB, Kazdin AE, eds. New York: Plenum, pp 73– 124Crossref, Google Scholar
Martin CS, Winters KC (1998), Diagnosis and assessment of alcohol use disorders among adolescents. Alcohol Health Res World 22: 95– 105Google Scholar
Metzger D, Kushner H, McLellan AT (1991), Adolescent Problem Severity Index. Philadelphia: University of PennsylvaniaGoogle Scholar
Meyers K, McLellan AT, Jaeger JL, Pettinati A (1995), The development of the Comprehensive Addiction Severity Index for Adolescents (CASI-A): an interview for assessing multiple problems of adolescents. J Subst Abuse Treat 12: 181– 193Crossref, Google Scholar
Monti PM, Colby SM, Barnett NP et al. (1999), Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. J Consult Clin Psychol 67: 989– 994Crossref, Google Scholar
Monti PM, Colby SM, O'Leary TA (2001), Adolescents, Alcohol, and Substance Abuse: Reaching Teens through Brief Interventions. New York: GuilfordGoogle Scholar
Myers MG, Brown SA, Mott MA (1995), Preadolescent conduct disorder behaviors predict relapse and progression of addiction for adolescent alcohol and drug abusers. Alcohol Clin Exp Res 19: 1528– 1536Crossref, Google Scholar
National Institute on Drug Abuse (NIDA) (2003), Preventing Drug Use Among Children and Adolescents: A Research-Based Guide: A Research-Based Guide for Parents, Educators, and Community Leaders, 2nd ed. Rockville, MD: NIDA/NIHGoogle Scholar
Newcomb MD (1997), Psychosocial predictors and consequences of drug use: a developmental perspective within a prospective study. J Addict Dis 16: 1– 89Crossref, Google Scholar
Physician Leadership on National Drug Policy (2002). Adolescent Substance Abuse: A Public Health Priority. Providence, RI: Physician Leadership on National Drug PolicyGoogle Scholar
Rahdert E (1991), The Adolescent Assessment and Referral System Manual. DHHS Publication No. (ADM) 91-1735. Rockville, MD: National Institute on Drug AbuseGoogle Scholar
Randall J, Henggeler SW, Cunningham PB, Rowland MD, Swenson C (2001), Adapting multisystemic therapy to treat adolescent substance abuse more effectively. Cognit Behav Practice 8: 359– 366Crossref, Google Scholar
Reinherz HZ, Giaconia RM, Lefkowitz ES, Pakiz B, Frost AK (1993), Prevalence of psychiatric disorders in a community population of older adolescents. J Am Acad Child Adolesc Psychiatry 32: 369– 377Crossref, Google Scholar
Resnik H (1990), Youth and Drugs: Society's Mixed Messages. Rockville, MD: Office for Substance Abuse Prevention, U.S. Department of Health and Human ServicesGoogle Scholar
Riggs PD, Davies R (2002), A clinical approach to treatment of depression in adolescents with substance use disorders and conduct disorder. J Am Acad Child Adolesc Psychiatry 41: 1253– 1255Crossref, Google Scholar
Riggs PD, Hall SK, Mikulich-Gilbertson SK, Lohman M, Kayser A (2004), A randomized controlled trial of pemoline for attention-deficit/hyperactivity disorder in substance-abusing adolescents. J Am Acad Child Adolesc Psychiatry 43: 420– 429Crossref, Google Scholar
Riggs PD, Leon SL, Mikulich SK, Pottle LC (1998), An open trial of bupropion for ADHD in adolescents with substance use disorders and conduct disorder. J Am Acad Child Adolesc Psychiatry 37: 1271– 1278Crossref, Google Scholar
Riggs PD, Mikovich SK, Coffman LM, Crowley TJ (1997). Fluoxetine in drug-dependent delinquents with major depression: an open trial. J Child Adolesc Psychopharmacol 7: 87– 95Crossref, Google Scholar
Riggs PD, Thompson LL, Mikulich SK, Whitmore EA, Crowley TJ (1996), An open trial of pemoline in drug-dependant delinquents with attentiondeficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 35: 1018– 1024Crossref, Google Scholar
Riggs PD, Whitmore EA (1999), Substance use disorders and disruptive behavior disorders. In: Disruptive Behavior Disorders in Children and Adolescents. Review of Psychiatry Series. Hendren RL, ed. Washington, DC: American Psychiatric Press, pp 133– 173Google Scholar
Robins LN, McEvoy L (1990), Conduct problems as predictors of substance abuse. In: Straight and Devious Pathways from Childhood to Adulthood, Robins LN, Rutter M, eds. Cambridge, England: Cambridge University Press, pp 182– 204Google Scholar
Rowe CL, Liddle HA, McClintic K, Quille T (2002), Integrative treatment development: multidimensional family therapy for adolescent substance abuse. In: Comprehensive Handbook of Psychotherapy, Kaslow F, Lebow J, eds. New York: John Wiley & Sons, pp 133– 161Google Scholar
Saffer H (2002), Alcohol advertising and youth. J Stud Alcohol 4: 173– 181Crossref, Google Scholar
Santisteban DA, Szapocznik J, Perez-Vidal A, Kurtines WM, Murray EJ, LaPerriere A (1996), Efficacy of intervention for engaging youth and families into treatment and some variables that may contribute to differential effectiveness. J Fam Psychol 10: 35– 44Crossref, Google Scholar
Simkin D (2004), Adolescent substance abuse. In: Kaplan and Sadock's Comprehensive Textbook of Psychiatry, Sadock BJ, Sadock VA, eds. Philadelphia: Lippincott Williams & Wilkins, pp 3470– 3491Google Scholar
Solhkhah R, Wilens TE (1998), Pharmacotherapy of adolescent alcohol and other drug use disorders. Alcohol Health Res World 22: 122– 125Google Scholar
Stanton MD, Shadish WR (1997), Outcome, attrition, and family-couples treatment for drug abuse: a meta-analysis and review of the controlled, comparative studies. Psychol Bull 122: 170– 191Crossref, Google Scholar
Szapocznik J, Kurtines WM, Foote FH, Perez-Vidal A, Hervis O (1983), Conjoint versus one-person family therapy: some evidence for the effectiveness of conducing family therapy through one person. J Consult Clin Psychol 51: 889– 899Crossref, Google Scholar
Szapocznik J, Perez-Vidal A, Briskman AL, Foote FH, Santisteban D, Hervis O (1988), Engaging adolescent drug abusers and their families in treatment. J Consult Clin Psychol 56: 552– 557Crossref, Google Scholar
Tapert SF, Baratta BS, Abrantes BA, Brown SA (2002), Attention dysfunction predicts substance involvement in community youth. J Am Acad Child Adolesc Psychiatry 141: 690– 686Google Scholar
Tarter RE (1990), Evaluation and treatment of adolescent substance abuse: a decision tree method. Am J Drug Alcohol Abuse 6: 1– 46Crossref, Google Scholar
Tarter RE, Vanyukov M, Giancola P et al. (1999), Etiology of early age onset substance use disorder: a maturational perspective. Dev Psychopathol 11: 657– 683Crossref, Google Scholar
University of Michigan (2003), 2003 Monitoring the Future Survey. Ann Arbor: Institute for Social ResearchGoogle Scholar
von Ranson KM, Iacono WG, McGue M (2002), Disordered eating and substance use in an epidemiological sample: I. Associations within individuals. Int J Eat Disord 31: 389– 403Crossref, Google Scholar
Wagner EF, Waldron HB (2001), Innovations in Adolescent Substance Abuse Interventions. Amsterdam: Pergamon/Elsevier ScienceGoogle Scholar
Waldron HB (1997), Adolescent substance abuse and family therapy outcome: a review of randomized trials. In: Advances in Clinical Child Psychology, Volume 19, Ollendick TH, Prinz RJ, eds. New York: Plenum, pp 199– 234Crossref, Google Scholar
Waldron HR, Slesnick N, Brody JL, Turner CW, Peterson TR (2001), Treatment outcomes for adolescent substance abuse at 4- and 7-month assessments. J Consult Clin Psychol 69: 802– 813Crossref, Google Scholar
Weinberg NZ, Rahdert E, Colliver JD, Glantz MD (1998), Adolescent substance abuse: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry 37: 252– 261Crossref, Google Scholar
Wilens TE, Biederman J, Spencer TJ, Frances RJ (1994), Comorbidity of attention-deficit disorder and psychoactive substance use disorders. Hosp Comm Psychiatry 45: 421– 435Google Scholar
Williams RJ, Chang SY (2000), A comprehensive and comparative review of adolescent substance abuse treatment outcome. Clin Psychol Sci Pract 7: 138– 166Crossref, Google Scholar
Winters KC (1992), Development of an adolescent substance abuse screening questionnaire. Addict Behav 17: 479– 490Crossref, Google Scholar
Winters KC (2001), Assessing adolescent substance use problems and other areas of functioning: state of the art. In: Adolescents, Alcohol, and Substance Abuse: Reaching Teens Through Brief Interventions, Monti PM, Colby SM, O'Leary TA, eds. New York: Guilford, pp 80– 108Google Scholar
Winters K, Henly G (1993), Adolescent Diagnostic Interview (ADI) Manual. Los Angeles: Western Psychological Services.Google Scholar
Winters KC, Stinchfield RD, Opland E (2000), The effectiveness of the Minnesota Model approach in the treatment of adolescent drug abusers. Addiction 65: 601– 612Crossref, Google Scholar
Note from the FOCUS Editors:
This guideline references drugs for which important revised regulatory information has been released. See FDA Website: www.fda.gov/default.htm
Atomoxetine (Strattera)
September/29/2005 http://www.fda.gov/cder/drug/infopage/atomoxetine/default.htm
FDA Alert [9/2005]: Suicidal Thinking in Children and Adolescents
The Food and Drug Administration (FDA) directed Eli Lilly (Lilly) to revise the labeling for Strattera to include a boxed warning and additional warning statements regarding an increased risk of suicidal thinking in children and adolescents being treated with this drug. In addition, a Medication Guide will be prepared to provide directly to patients, their families, and caregivers information about the risks mentioned above. The Medication Guide is intended to be distributed by the pharmacist with each prescription or refill of a medication.
Strattera is currently approved in the United States to treat ADHD in children, adolescents, and adults.
Strattera has not been studied in children under 6 years of age.
Suicidality in Children and Adolescents Being Treated With Antidepressant Medications
October 15, 2004 http://www.fda.gov/cder/drug/antidepressants/SSRIPHA200410.htm
Today the Food and Drug Administration (FDA) directed manufacturers of all antidepressant drugs to revise the labeling for their products to include a boxed warning and expanded warning statements that alert health care providers to an increased risk of suicidality (suicidal thinking and behavior) in children and adolescents being treated with these agents, and to include additional information about the results of pediatric studies. FDA also informed these manufacturers that it has determined that a Patient Medication Guide (MedGuide), which will be given to patients receiving the drugs to advise them of the risk and precautions that can be taken, is appropriate for these drug products. These labeling changes are consistent with the recommendations made to the Agency at a joint meeting of the Psychopharmacologic Drugs Advisory Committee and the Pediatric Drugs Advisory Committee on September 13–14, 2004.
Pemoline Tablets and Chewable Tablets (Cylert)
FDA Alert [10/24/2005]: Liver Injury Risk and Market Withdrawal http://www.fda/gov/cder/drug/InfoSheets/HCP/pemolineHCP.htm
The Agency (FDA) has concluded that the overall risk of liver toxicity from Cylert and generic pemoline products outweighs the benefits of this drug. In May 2005, Abbott chose to stop sales and marketing of Cylert in the U.S. All generic companies have also agreed to stop sales and marketing of this product (Pemoline tablets and chewable tablets). Cylert is a central nervous system stimulant indicated for the treatment of Attention Deficit Hyperactivity Disorder (ADHD). This product is considered second line therapy for ADHD because of its association with life threatening hepatic failure (see BOXED WARNING in product label and patient package insert, available athttp://www.fda.gov/cder/foi/label/2003/016832s022_017703s018lbl.pdf



