Diagnosis and Treatment of Anxiety
Abstract
Anxiety disorders are highly prevalent, disabling conditions. The diagnoses of anxiety disorders are continually undergoing revision. In clinical treatment and research, both dimensional and structural diagnoses can be used, depending on the situation. Recently, emphasis has been placed on neuroimaging and genetic research as they apply to specific treatment sites. Although this research generally has not yet produced new treatments or diagnostic procedures, it has provided a more comprehensive understanding of how genetic, biological, and stress factors interact to shape the symptoms of anxiety. Anxiety disorders can be treated effectively with cognitive-behavioral and psychopharmacological interventions. Because these interventions target different symptoms, combinations of the different strategies need to be further studied. Alternative treatment strategies are widely used and continue to develop, but thus far they have not shown efficacy comparable to mainstream treatments. Treatment algorithms for anxiety disorders should be developed that can be used easily in primary care settings, and such algorithms should emphasize the management of functional impairment in patients with anxiety disorders.
Anxiety disorders constitute the largest group of psychiatric disorders as well as the most prevalent (1), yet they have not received the broad recognition that other major syndromes, such as mood disorders and psychotic disorders, have received. Even 20 years after the Epidemiologic Catchment Area study first revealed the true prevalence of this group of disorders (2), they remain poorly recognized and treated. Anxiety disorders reduce productivity and increase morbidity, mortality, and alcohol and drug abuse in a large segment of the population (3–5).
In recent years, however, many developments have occurred in the study of anxiety. The most significant among them are reviewed here in order to help clinicians better understand and treat anxiety disorders.
Table 1 lists the anxiety disorders that are included in DSM-IV-TR (6). Posttraumatic stress disorder (PTSD) was the topic of the Summer 2003 issue of Focus and will not be discussed in this issue.
Clinical context
Diagnostic dilemmas
Epidemiological research on anxiety over the past decade has served to refine the categorical diagnoses of anxiety disorders through succeeding editions of the DSM. As the data from the National Comorbidity Survey indicate, however, comorbidity is common with this group of disorders (1). In some disorders, such as generalized anxiety disorder, comorbidity is the rule rather than the exception (7). In many other anxiety disorders, it is not unusual for two or more diagnosable conditions to coexist or for there to be some symptomatic overlap between an anxiety disorder and subsyndromal states, especially symptom overlap between different anxiety disorders and between anxiety and depression (8).
Because of this extensive comorbidity and the absence of specific etiological factors and specific treatments, researchers suggested that a dimensional model might be more useful for studying and treating these conditions (9). In the dimensional approach, the disorder is seen as a complex of coexisting symptomatic dimensions, such as panic, anticipation, obsessiveness, and avoidance. Each of these dimensions can be used in research to correlate hypothetical, biological, or genetic factors. Each dimension also may require a distinct biological or psychological treatment approach (e.g., behavioral treatment for panic or specific medication for treatment of obsessive trends). One of the fruitful ways of making a dimensional diagnosis is to analyze psychometric rating scales that have been designed to measure personality characteristics or symptoms of a specific condition. The comparative usefulness of dimensional and categorical diagnoses is a highly debated issue in research and in clinical practice. Both approaches are acceptable, depending on the circumstances. For example, the categorical diagnosis of obsessive-compulsive disorder (OCD) may be more useful in a clinical discussion of a patient, whereas a dimensional delineation of “obsessiveness” may be more useful in research seeking a gene responsible for this symptom.
Similarities between disorders and categorical/dimensional perspectives led to the introduction of the term “spectrum disorders,” a phrase initially developed for OCD (10). This conceptualization was helpful in evaluating similar responses to pharmacological and psychological treatments, and it led to the development of other spectrums, including social anxiety, panic-agoraphobic, and posttraumatic spectrum disorders (11–13). Although this approach is useful, it may be overinclusive and misleading, as it lumps together disorders that have little in common (such as pathological gambling and body dysmorphic disorders in OCD spectrum).
Dimensional/categorical diagnosis is usually produced by cross-sectional observation. However, the diagnostic presentation may be better understood as a psychopathological process. For example, obsessive and compulsive symptoms are related, since compulsions are usually designed to counteract a threat, and anxiety is associated with obsessive thought. In medical diseases, symptoms usually represent a combination of a noxious agent and the body’s reaction to its presence. Psychiatric symptoms may behave the same way. Thus, anxiety disorders may be viewed as a sequential process of the emergence of initial symptoms and inadequate mental or behavioral attempts to deal with the perceived problem.
For example, panic disorder (see Table 2) may start as an initial devastating panic attack that leads to an increased concern about personal health and safety. This concern then leads to a medical workup, which initially calms the fear. However, worry and anticipation of another, imminent attack persist because of an abnormal catastrophic perception of the events that created the situation, and no amount of reassurance is enough to allay the patient’s fears. This leads to an increase in “safety” coping behaviors, such as having repeated medical examinations, carrying a cell phone, and having a “safe” person around at all times. Unfortunately, since absolute “safety” can never be found, these behaviors become more and more extensive and unreasonable and induce more anxiety, starting the vicious cycle of the disorder and leading to even more inappropriate coping, such as agoraphobic avoidance, eventually resulting in despair and depression.
Most of the anxiety disorders follow this process, although different stages may predominate in different disorders (e.g., ritualistic behavior is more characteristic of OCD, and avoidance predominates in social anxiety disorder). Understanding the process of the disorder and the core fears and coping strategies may lead to more precise diagnosis and help in the biological and psychological management of the disorder. Lack of such an understanding may lead to the misdiagnosis of an anxiety disorder as another one with a similar presentation. For example, in public speaking phobia, the patient may have a fear of being evaluated, which is more a component of social anxiety disorder, or a fear of mispronouncing words, which is more OCD-like. Both will result in avoidance of social situations, but the two would be managed differently.
Biological and psychological factors
To effectively treat an anxiety disorder, the clinician must understand how the condition emerges and what factors contribute to its maintenance. One of the major advances in anxiety research in recent years is our better understanding of the interplay of genetic, biological, and stress factors in the presentation of anxiety disorders. Study of the genetic underpinnings of anxiety disorders using the most modern techniques have yet to identify a gene or even multiple gene solutions for any single anxiety disorder, although some interesting findings have been reported for OCD and agoraphobia (14, 15). However, family and twin studies suggest that some genetic components may be shared between different anxiety disorders, depression, and alcohol and drug abuse (16). Currently, it is not clear what exactly is inherited in anxiety disorders.
One possibility is that abnormal cognitions could be the inherited factor. Cognitive theory assigns primary importance to abnormal or “catastrophic” cognitions as an underlying mechanism of all of the anxiety disorders. Most of the cognitive strategies for treatment and research were developed long ago. Recently, there has been a shift to the recognition of abnormal information processing in anxiety disorders. In a majority of anxiety disorders, information about threat is processed in a very peculiar way. Patients typically catalog the information in excessive detail or divide the information into “good” and “bad,” with no gray area in between, and later question whether or not the threat exists. Under these circumstances, the only safe way to deal with the situation is to consider the worst-case scenario (i.e., using catastrophic cognition) and then act to protect oneself against the danger.
Stress also plays a major role in the pathology of anxiety disorders, and in PTSD it is the main etiological factor. Although the role of stress is less apparent in other anxiety disorders, patients can often date the onset of their disorder to a strong stress event or to a period of continuous, persistent stress. It is well known that anxiety disorders are stress dependent. For example, increased stress usually accounts for relapses in chronic anxiety conditions such as generalized anxiety disorder. Recent findings also indicate that stress produced by an event or by a persistent and chronic disorder is capable of causing secondary biological changes in specific brain structures (17, 18).
The relationship between biological factors, genetic factors, and stress is a complex one. Catastrophic stresses, such as those associated with PTSD, can produce a disorder even in the absence of damage to the brain or a genetic predisposition to the disorder. At the same time, damage to the brain or heightened genetic vulnerability, as in the case of patients who have multiple relatives suffering from an anxiety disorder, can be a cause of anxiety with minimal or no stress. Most patients, however, are in between these extremes, and typically there is some interplay of the various factors. Clinicians need to address this complex interplay of factors in order to have a complete picture of the patient’s psychopathology and to develop a sound treatment plan. This approach calls for a revision or expansion of axis IV of DSM-IV-TR to account for the acuity, severity, and duration of stress.
Chronic stress in patients with anxiety and mood disorders can cause dysregulation of the hypothalamic-pituitary-adrenal axis (18). In addition, acute and chronic stress causes an elevation in glutamate levels that can cause secondary toxicity in some parts of the brain, such as the hippocampus, which can account for the reduction of hippocampal volume seen in patients with PTSD (19). Biological investigations of the stress system in anxiety disorders are scarce, and more research in this area is needed. Such research is complicated by the fact that chronic psychiatric illnesses such as OCD, generalized anxiety disorder, and PTSD frequently lead to decreases in functioning (e.g., loss of job or relationships), which can produce the secondary stress.
Biological factors are of primary importance in anxiety disorders. Anxiety disorders can occur in the context of medical illness, for example. The list of medical conditions that should be considered in the differential diagnosis of anxiety disorder is extensive (see Table 3). The clinician should consider the possibility of an intricate, manifold relationship between medical illnesses and anxiety disorders. Metabolic or autonomic abnormalities caused by an illness could produce the syndrome of anxiety—for example, hyperthyroidism could produce panic attacks. The symptoms of a medical illness could serve as a trigger for anxiety, such as the sensation of an abnormal heartbeat in arrhythmia triggering a panic attack. Sometimes the medical illness mimics the anxiety disorder, as with perseveration in mental retardation and OCD. Finally, medical illness and an anxiety disorder could simply coexist. Among the most interesting interactions between medical illness and anxiety disorders studied in recent years are the pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS) observed in a subset of OCD patients (20).
In recent years, the main thrust of biological research has shifted increasingly from peripheral measures of autonomic and neurochemical parameters to the use of neuroimaging techniques to directly identify reactivity and neurochemistry of live brain in anxiety disorders. This research on neuronal circuits is generally developed around models of anxiety and fears that were proposed earlier by basic scientists (21, 22). A synthesis of current data has been attempted for panic (23) and OCD (24), although the puzzle has not been completed.
Anxiety disorders are an especially appropriate target for neuroimaging research, because a specific symptom provocation can often be employed. Excellent reviews of neuroimaging experiments in anxiety have been published (25, 26), although to date the data remain limited. As discussed earlier, every anxiety disorder may be viewed as an interplay of initial anxiety, abnormal information processing, and inadequate coping strategies. In the contemporary model of anxiety, specific neuronal circuits are responsible for alarm reactions, processing of threat information, and behavioral coping (Table 4). Alarm circuits include the amygdala, periaqueductal gray matter, and the hippocampus area. A disturbance of these circuits produces a lower threshold for alarm reactions such as spontaneous panic attacks. These circuits may be responsible for a quick-learning response to a threat. Information processing circuits are probably closely associated with the cingulum and cortico-striatal systems, which are typically affected in OCD. Abnormalities in coping are very likely governed by large cortical networks and hence will be difficult to tease apart. The above-mentioned models attempt to simplify very complex brain circuitry that will probably be extensively studied over the next several decades before a solid understanding emerges of how the brain processes and deals with threat.
The postulated circuits are governed by multiple neurotransmitter systems, with gamma-aminobutyric acid (GABA) and glutamate the most prominent among them. Three major neurotransmitter systems—serotonin, dopamine, and norepinephrine—have been extensively studied in normal and pathological anxiety states. The significance of these systems is clear from the fact that most of the effective treatments of anxiety affect one or several of the systems. It is clear, however, that anxiety disorders are not a result of a simple deficiency of one of the neurotransmitters. The accumulated body of research shows that the networks governed by these transmitters have extensive interrelationships, multiple feedback mechanisms, and complex receptor structures. This complexity can explain the unpredictable and sometimes paradoxical responses to medication. A new avenue of research involving other, more specific neurotransmitter systems has been fruitful in elucidating their function in anxiety but thus far has not produced any new treatments.
Treatment strategies and evidence
Initial treatment algorithms
In the past decade, mainstream psychological and pharmacological treatments of anxiety disorders have been developed and tested. The initial algorithm is similar for all major anxiety disorders (27, 28). The typical algorithm is presented in Figure 1. In general, one must choose between cognitive behavior treatment and a selective serotonin reuptake inhibitor (SSRI); another SSRI is tried if the first one does not work or is not tolerated. None of the SSRIs has shown superiority to the others, and the choice of an SSRI is usually based on side effect profile (Table 5), pharmacokinetic and pharmacodynamic properties, and drug-drug interactions. The use of SSRIs in anxiety disorders has been carefully reviewed (29). The principle of “start low and go slow” applies when SSRIs are used in the management of anxiety—that is, start with about half of the dose used in depression and use a slow titration, changing the dose no more than once a week. Discontinuation of SSRIs has not been well studied but should be done very gradually and, if possible, in parallel with cognitive behavior therapy.
Cognitive behavior therapy
Cognitive behavior therapy is important in the treatment of anxiety disorders and deserves a more extensive discussion than can be provided here. Any contemporary clinician who works with patients with anxiety disorders should know the elements of cognitive behavior therapy. The therapy is usually disorder specific, although it shares many features between the disorders. Manuals are available for all of the anxiety disorders, and references to them can be found on the Anxiety Disorders Association of America Web site (www.adaa.org).
Cognitive behavior therapy starts with an extensive assessment and education for the patient on the principles and goals of therapy. Homework assessment and intervention tasks are a common and often required component of the therapy. The core of the therapy consists of cognitive restructuring that is aimed at changing pathological catastrophic or overgeneralized thinking, followed by exposure and response prevention tasks. Exposure and response prevention, which requires close patient-therapist collaboration, essentially consists of exposure to impulses, images, feelings, or situations the patient fears while preventing the patient from using his or her abnormal coping strategies, such as rituals, mental distractions, and escape. A variety of treatment strategies have been developed over the years, including gradual exposure to fear-producing stimuli (internal or external) or immediate and forceful exposures to the worst feared situation (referred to as flooding). During the response prevention phase, provoked anxiety usually decreases over a period of 2 hours, permitting the patient to develop more rational thinking as well as more adequate coping strategies.
These treatments are very effective. Some papers describe response rates in excess of 80% in panic disorder (30). A response can sometimes be achieved within a six-session program (31). Randomized clinical trials have shown cognitive behavior therapy to be superior to medication (32). Cognitive behavior therapy can also be helpful in withdrawing patients from antidepressants and benzodiazepines, and ongoing cognitive behavior therapy is associated with fewer relapses over time (33, 34). Why, then, is cognitive behavior therapy not always used instead of medication? The answer is that for cognitive behavior therapy to be given, the patient must agree to it. Some patients reject it because it frequently provokes more anxiety, especially during the initial phases of therapy. Some reject it because they have a bias against psychological interventions or consider their symptoms to be the result of a medical illness. Cost, along with the generally poor insurance coverage of cognitive behavior therapy, is another reason for patients to reject the treatment. Finally, many patients have difficulty finding trained behavior therapists, since most psychology programs produce graduates who prefer insight-oriented treatment to cognitive behavior therapy.
Management of nonresponse to treatment
Patients who do not respond to initial therapy with an SSRI or cognitive behavior therapy are treated with other antidepressants that have a broader mechanism of action, such as venlafaxine and clomipramine. These medications act on more than one neurotransmitter system, and some meta-analytic data suggest that they may be more effective in the treatment of depression and OCD (35). Benzodiazepines are generally avoided except in the treatment of acute states or treatment-resistant chronic conditions.
There is little clinical evidence on what to do after the few initial steps of the treatment, although the past few years have seen more testing of combined treatment strategies at the initial and later steps of the typical algorithm (32, 36).
In recent years some clinical evidence has been produced that supports the use of two groups of medications that show efficacy at later stages of treatment of anxiety disorders, namely, GABA-ergic antiepileptics and atypical antipsychotics. In multiple case reports, nearly every antiepileptic, and especially valproate and gabapentin, has been described as an effective tool in treating anxiety disorders. The evidence for efficacy in the treatment of anxiety is even stronger for atypical antipsychotics, as demonstrated in placebo-controlled trials in which OCD was specifically studied (37). Polypharmacy is becoming the rule rather than the exception, especially for complex and treatment-resistant cases.
Combining cognitive behavior therapy and medication
Some studies have shown that medication treatment does not confer any additional benefits to cognitive behavior therapy, whereas other studies have shown that joint treatment with cognitive behavior therapy and medication can be an effective approach (38). It makes sense to combine these two effective strategies, for some patients at least, since the two modalities probably have different primary targets. With medication treatment, the primary targets are alarm reactivity and abnormal information processing and cognitive appraisal of the threat. While improvements in these areas could lead to secondary behavior changes, it is unlikely that any of the pharmacological agents currently in use directly affect complex behaviors such as avoidance. In fact, extensive compulsions and avoidance are among the best predictors of nonresponse to SSRIs (39). Furthermore, medications that reduce alarm frequently also cause sedation or a reduction in general alertness, thus limiting the tolerable dose of any antianxiety medication. Strong episodic responses that are cued to specific phobic situations can still break through and create considerable discomfort even in sedated patients.
Cognitive behavior therapy, by contrast, largely targets abnormal coping strategies. Modification of abnormal behaviors leads to secondary changes in cognitions and to a resetting of the alarm to a lower level. Understanding these processes can help in the rational use of combined treatment. For example, a physician working with a behavioral therapist may want to “undertreat” anxiety to leave room for a behavioral intervention. Another consideration is to avoid use of medication strategies that have been shown to interfere with learning (e.g., large as-needed doses of benzodiazepines or the use of other sedating medications). It is of paramount importance that each of the health care professionals treating the patient know their treatment targets, the limitations of their treatment, and the roles and responsibilities of the others involved. Frequent communication among treatment team members is a must, especially during the initiation or discontinuation of treatment. For example, medication may need to be stabilized before cognitive behavior therapy begins and withdrawn before it ends. Some patients may not need medication treatment at all, and some would not be able to process the information necessary to achieve success in behavioral treatment without medication. The complexity of combined treatment can hardly be re-created experimentally, which may explain why it was not found to be superior in some studies.
Shifting treatment to primary care settings
In the managed care environment, most treatment of anxiety disorders occurs in primary care settings. Primary care physicians notoriously underrecognize and undertreat anxiety. However, they increasingly prescribe SSRIs to manage emotional distress of all sorts. Because SSRIs are often prescribed in inadequate doses for an inadequate duration and side effects are often managed only by discontinuation of the treatment, psychiatrists are currently seeing patients who have more severe, treatment-resistant anxiety disorders and frequently are disenchanted with the medication.
Another problem of primary care is a lack of understanding of behavioral strategies and hence low referral rates to mental health professionals. In the past five years, efforts have been made to develop comprehensive treatments for panic disorder that can be delivered in the primary care setting. One recent study, for example, tested such an algorithm for the treatment of panic disorder (40). Such studies reflect the current trend of psychiatrists becoming more like consultants to primary care physicians, assisting them in formulating correct initial management plans and taking over the management of more severe and treatment-resistant cases.
Management of treatment resistance
In managing treatment-resistant anxiety it is important to start with a reevaluation of the patient. All the factors discussed above are important, including diagnosis, comorbidity, and the interplay of biological, cognitive, and stress factors. Inadequate coping strategies, on the part of both the patient and the patient’s family, need to be reviewed. Medication doses and duration of the initial treatments need to be examined. Initially, a more intensive course of cognitive behavior therapy in combination with an adequate trial of an SSRI, a serotonin and norepinephrine reuptake inhibitor (SNRI), or a combination of these may be needed to confirm a treatment-resistant disorder. After that, treatment may progress to a combination of an SSRI with an antiepileptic or an atypical antipsychotic, especially if a comorbid bipolar or psychotic disorder is suspected (41, 42). Later, partial hospitalization in specialized centers with more extensive cognitive behavior therapy and medication management could be recommended (43). While other forms of therapy have not demonstrated efficacy in the treatment of anxiety disorders, they may be helpful for patients with chronic anxiety in order to address personality issues.
Questions and controversy
Experimental treatments
Treatments of anxiety disorders other than combinations of conventional treatments, off-label use of antiepileptics, antipsychotic agents, and more intensive cognitive behavior therapy programs are largely experimental. Most of the promising medication treatments, such as intravenous clomipramine, intravenous citalopram, and oral morphine for OCD, are under investigation (41). Many other treatments targeting more specific neurotransmitter systems have failed. Electroconvulsive therapy and transcranial magnetic stimulation seem to have only limited value. Vagus nerve stimulation and deep brain stimulation are under investigation, although no clear evidence of efficacy has been produced. Neurosurgery or deep brain stimulation should be considered only in the treatment of intractable OCD in which the suffering of the patient and the family is unbearable (44). Neurostimulation and neurosurgical methods need to proceed carefully, since there is always controversy about possible treatment abuse and “mind control.”
Alternative treatments
In recent years, many alternative treatment strategies for anxiety disorders have emerged (45). Thus far, however, they have not shown efficacy comparable to mainstream treatments. Nevertheless, given that some 8% of anxiety patients are using them, clinicians should be aware that some of their patients might be trying an alternative treatment concurrently with mainstream treatment. Such treatments include herbal medications (most commonly, St. John’s wort), vitamins, and different types of magnetic and EEG synchronizing devices. Clinicians should educate their patients on the fact that “herbal” is not equivalent to “safe.” Some herbal treatments can cause serious side effects and interactions with mainstream treatments (e.g., SSRIs can interact with St. John’s wort). Eastern medicine, such as Chinese, ayurvedic, and Tibetan approaches, offers anxiety relief as a part of a complex healing process. More research is needed on the interplay of these treatments with their Western counterparts. At the same time, there are new developments in psychological treatments for anxiety that utilize some components of the Eastern approaches—for example, the use of “mindfulness” and meditation as an alternative to cognitive behavior therapy, and computer-assisted “virtual” exposure techniques. More exploration of the efficacy of these alternative strategies for anxiety disorders is needed.
Focus on functional status
Although treatment can relieve anxiety symptoms in many patients, the residual symptoms still have an impact on the patients’ functioning. The research has demonstrated that even subclinical anxiety can produce disability, sometimes exceeding that seen in other severe mental illnesses (43, 46). In addition, chronic, persistent anxiety disorders have a significant impact on the patient’s life, creating deficiencies in social and work skills. Yet there are no clear interventions or programs that focus on rehabilitation and the restoration of function in patients with anxiety disorders. As discussed above, stress is an important factor in the emergence and maintenance of anxiety syndromes. Patients who need to return to the workforce would experience increased stress, which may provoke a reemergence of the symptoms, resulting once again in a decrease in productivity and possibly the loss of employment. More research and development are needed to address this issue and to develop strategies that use focused interventions to address functional status.
Conclusions
Effective treatments for anxiety disorders have been developed, and algorithms for treatment have been shaping up in recent years. Anxiety disorders are treatable. However, more work needs to be done, not least in further merging our developing knowledge of biological mechanisms of anxiety with treatment strategies in order to better predict and improve treatment response. We also need to learn how to better administer our current efficacious treatments in real-life health care settings. Furthermore, we need to test alternative treatment strategies, which continue to emerge, and to identify their place in the treatment and prevention of anxiety disorders. We need to maintain our efforts to treat patients whose anxiety is resistant to current treatment strategies. Finally, we need to focus early on the functional aspects of the human response to mental illness and find ways to manage it effectively. All of these measures will improve the care we give people who suffer from anxiety disorders.
| Panic disorder |
| Agoraphobia |
| Social phobia |
| Specific phobia |
| Posttraumatic stress disorder |
| Acute stress disorder |
| Generalized anxiety disorder |
| Obsessive-compulsive disorder |
| Anxiety disorder due to a general medical condition |
| Substance-induced anxiety disorder |
| Anxiety disorder not otherwise specified |
| Prodrome (stress/anxiety/worry) |
| Initial panic attack |
| Health worry (scanning, anticipation) |
| Limited avoidance (attempts to suppress or prevent an attack, leading to new panic attacks) |
| Extensive avoidance |
| Depression |
| Medical disorders |
| Cardiac conditions |
| Arrhythmiasa,c,d |
| Supraventricular tachycardiaa,c,d |
| Mitral valve prolapseb,c,d |
| Endocrine disorders |
| Thyroid abnormalitya,b,c,d |
| Hyperparathyroidismb,c,d |
| Pheochromocytomad |
| Hypoglycemiaa,c,d |
| Vestibular dysfunctionb,c,d |
| Seizure disorders (e.g., temporal lobe epilepsya,b,c,d) |
| Psychiatric disorders |
| Affective disorders |
| Major depressiond,e,f |
| Bipolar disorderb,d,e,f |
| Other anxiety disordersa,b,c,d,e,f |
| Acute stress disordera,b,c,d,e,f |
| Obsessive-compulsive disordera,b,c,d,e,f |
| Posttraumatic stress disordera,b,c,d,e,f |
| Social phobiaa,c,d,e,f |
| Specific phobiaa,c,d,e,f |
| Psychotic disordersa,d,e,f |
| Substance abuse and dependence |
| Withdrawal from central nervous system depressantsa,b,c,d,e,f |
| Alcohol abuse |
| Barbiturates |
| Stimulantsa,b,c,d,e,f |
| Cocaine |
| Amphetamines |
| Caffeine |
| Cannabisa,b,c,d,e,f |
| Hallucinogensa,b,c,d,e,f |
| Stages of Disorder | Neuronal Circuits | Possible Treatments |
|---|---|---|
| Anxiety attacks (alarm reactions) | Periaqueductal gray matter, amygdala, hippocampus | Low-dose SSRIs, SNRIs, benzodiazepines; introceptive exposure |
| Anxious expectation, catastrophic thoughts (abnormal information processing) | Orbital frontal cortex, cingulum, hippocampus, striatum | SSRIs, SNRIs, cognitive restructuring, antipsychotics |
| Precautions, rituals, and avoidances | Prefrontal and temporal cortex | SSRIs, SNRIs, antipsychotics, exposure and response prevention |
| Adverse Effect | Fluoxetine | Sertraline | Paroxetine | Fluvoxamine | Citalopram or Escitalopram | Venlafaxinea | Nortriptyline | Clomipramine |
|---|---|---|---|---|---|---|---|---|
| Headache | ↑ | — | — | — | — | — | ↓ | — |
| Agitation or anxiety | ↑↑ | ↑ | — | — | ↑ | ↑ | — | — |
| Tremor | ↑ | ↑ | ↑ | — | — | ↑↑ | ↑↑ | ↑↑ |
| Insomnia | ↑↑ | ↑↑ | — | — | — | ↑↑ | ↓ | — |
| Drowsiness | ↑ | ↑ | ↑↑ | ↑↑ | — | ↑↑ | ↑↑ | ↑↑ |
| Fatigue | ↑ | — | ↑↑ | — | ↑ | ↑ | ↑↑ | ↑↑ |
| Confusion | — | — | — | — | — | — | — | — |
| Dizziness | — | — | ↑ | — | — | ↑ | ↑ | ↑ |
| Anticholinergic effectsb | — | — | ↑ | — | — | — | ↑↑↑ | ↑↑↑ |
| Sweating | — | — | — | — | — | ↑↑ | ↑↑ | ↑↑ |
| Weight gain | ↑ | ↑ | ↑↑ | ↑ | — | ↑ | ↑↑ | ↑↑ |
| Gastrointestinal effects | ↑ | ↑↑ | — | ↑↑ | — | ↑↑ | — | — |
| Sexual side effectsc | ↑↑ | ↑↑ | ↑↑ | ↑ | ↑ | ↑↑ | ↑ | ↑↑ |
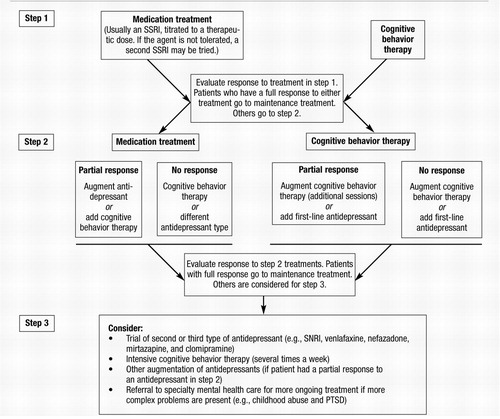
Figure 1. Stepped Algorithm for the Treatment of Anxiety Disorders
1 Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8–19Crossref, Google Scholar
2 Weissman MM, Merikangas KR: The epidemiology of anxiety and panic disorders: an update. J Clin Psychiatry 1986; 47(suppl):11–17Google Scholar
3 Leon AC, Portera L, Weissman MM: The social costs of anxiety disorders. Br J Psychiatry Suppl 1995; 27:19–22Google Scholar
4 Wittchen HU, Fehm L: Epidemiology, patterns of comorbidity, and associated disabilities of social phobia. Psychiatr Clin North Am 2001; 24:617–641Crossref, Google Scholar
5 Wittchen HU, Kessler RC, Beesdo K, Krause P, Hofler M, Hoyer J: Generalized anxiety and depression in primary care: prevalence, recognition, and management. J Clin Psychiatry 2002; 63(suppl 8):24–34Google Scholar
6 Diagnostic and Statistical Manual of Mental Disorders, 4th ed, Text Revision. Washington, DC, American Psychiatric Association, 2000Google Scholar
7 Vollebergh WA, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J: The structure and stability of common mental disorders: the NEMESIS study. Arch Gen Psychiatry 2001; 58:597–603Crossref, Google Scholar
8 Kaufman J, Charney D: Comorbidity of mood and anxiety disorders. Depress Anxiety 2000; 12(suppl 1):69–76Crossref, Google Scholar
9 Brown TA, Chorpita BF, Barlow DH: Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. J Abnorm Psychol 1998; 107:179–192Crossref, Google Scholar
10 Hollander E, Kwon JH, Stein DJ, Broatch J, Rowland CT, Himelein CA: Obsessive-compulsive and spectrum disorders: overview and quality of life issues. J Clin Psychiatry 1996; 57(suppl 8):3–6Google Scholar
11 Shear MK, Frank E, Rucci P, Fagiolini DA, Grochocinski VJ, Houck P, Cassano GB, Kupfer DJ, Endicott J, Maser JD, Mauri M, Banti S: Panic-agoraphobic spectrum: reliability and validity of assessment instruments. J Psychiatr Res 2001; 35:59–66Crossref, Google Scholar
12 Moreau C, Zisook S: Rationale for a posttraumatic stress spectrum disorder. Psychiatr Clin North Am 2002; 25:775–790Crossref, Google Scholar
13 Schneier FR, Blanco C, Antia SX, Liebowitz MR: The social anxiety spectrum. Psychiatr Clin North Am 2002; 25:757–774Crossref, Google Scholar
14 Weissman MM, Fyer AJ, Haghighi F, Heiman G, Deng Z, Hen R, Hodge SE, Knowles JA: Potential panic disorder syndrome: clinical and genetic linkage evidence. Am J Med Genet 2000; 96:24–35Crossref, Google Scholar
15 Leckman JF, Pauls DL, Zhang H, Rosario-Campos MC, Katsovich L, Kidd KK, Pakstis AJ, Alsobrook JP, Robertson MM, McMahon WM, Walkup JT, van de Wetering BJ, King RA, Cohen DJ; Tourette Syndrome Assocation International Consortium for Genetics: Obsessive-compulsive symptom dimensions in affected sibling pairs diagnosed with Gilles de la Tourette syndrome. Am J Med Genet 2003; 116B(1):60–68Crossref, Google Scholar
16 Hettema JM, Neale MC, Kendler KS: A review and meta-analysis of the genetic epidemiology of anxiety disorders. Am J Psychiatry 2001; 158:1568–1578Crossref, Google Scholar
17 Bremner JD: Functional neuroanatomical correlates of traumatic stress revisited 7 years later, this time with data. Psychopharmacol Bull 2003; 37(2):6–25Google Scholar
18 Axelson DA, Doraiswamy PM, McDonald WM, Boyko OB, Tupler LA, Patterson LJ, Nemeroff CB, Ellinwood EH Jr, Krishnan KR: Hypercortisolemia and hippocampal changes in depression. Psychiatry Res 1993; 47:163–173Crossref, Google Scholar
19 Nutt DJ: The psychobiology of posttraumatic stress disorder. J Clin Psychiatry 2000; 61(suppl 5):24–29, discussion 30–32Google Scholar
20 Swedo SE: Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS). Mol Psychiatry 2002; 7(suppl 2):S24–S25Crossref, Google Scholar
21 LeDoux J: Fear and the brain: where have we been, and where are we going? Biol Psychiatry 1998; 44:1229–1238Crossref, Google Scholar
22 Fendt M, Fanselow MS: The neuroanatomical and neurochemical basis of conditioned fear. Neurosci Biobehav Rev 1999; 23:743–760Crossref, Google Scholar
23 Gorman JM, Kent JM, Sullivan GM, Coplan JD: Neuroanatomical hypothesis of panic disorder, revised. Am J Psychiatry 2000; 157:493–505Crossref, Google Scholar
24 Saxena S, Rauch SL: Functional neuroimaging and the neuroanatomy of obsessive-compulsive disorder. Psychiatr Clin North Am 2000; 23:563–586Crossref, Google Scholar
25 Dager SR, Layton M, Richards T: Neuroimaging findings in anxiety disorders. Semin Clin Neuropsychiatry 1996; 1:48–60Google Scholar
26 Charney DS: Neuroanatomical circuits modulating fear and anxiety behaviors. Acta Psychiatr Scand Suppl 2003; 417:38–50Google Scholar
27 Roy-Byrne P, Stein M, Bystrisky A, Katon W: Pharmacotherapy of panic disorder: proposed guidelines for the family physician. J Am Board Fam Pract 1998; 11:282–290Crossref, Google Scholar
28 Pollack MH: New advances in the management of anxiety disorders. Psychopharmacol Bull 2002; 36(4 suppl 3):79–94Google Scholar
29 Gorman JM, Kent JM: SSRIs and SMRIs: broad spectrum of efficacy beyond major depression. J Clin Psychiatry 1999; 60(suppl 4):33–38, discussion 39Crossref, Google Scholar
30 Craske MG, Rodriguez BI: Behavioral treatment of panic disorders and agoraphobia. Prog Behav Modif 1994; 29:1–26.Google Scholar
31 Craske MG, Maidenberg E, Bystritsky A: Brief cognitive-behavioral versus nondirective therapy for panic disorder. J Behav Ther Exp Psychiatry 1995; 26:113–120Crossref, Google Scholar
32 Hembree EA, Riggs DS, Kozak MJ, Franklin ME, Foa EB: Long-term efficacy of exposure and ritual prevention therapy and serotonergic medications for obsessive-compulsive disorder. CNS Spectr 2003; 8:363–71, 381Google Scholar
33 Otto MW, Pollack MH, Meltzer-Brody S, Rosenbaum JF: Cognitive-behavioral therapy for benzodiazepine discontinuation in panic disorder patients. Psychopharmacol Bull 1992; 28(2):123–130Google Scholar
34 Allgulander C, Bandelow B, Hollander E, Montgomery SA, Nutt DJ, Okasha A, Pollack MH, Stein DJ, Swinson RP; World Council of Anxiety: WCA recommendations for the long-term treatment of generalized anxiety disorder. CNS Spectr 2003; 8(suppl 1):53–61Crossref, Google Scholar
35 Greist JH: The comparative effectiveness of treatments for obsessive-compulsive disorder. Bull Menninger Clin 1998; 62(4 suppl A):A65–A81Google Scholar
36 Barlow DH, Gorman JM, Shear MK, Woods SW: Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: a randomized controlled trial. JAMA 2000; 283:2529–2536Crossref, Google Scholar
37 McDougle CJ, Epperson CN, Pelton GH, Wasylink S, Price LH: A double-blind, placebo-controlled study of risperidone addition in serotonin reuptake inhibitor-refractory obsessive-compulsive disorder. Arch Gen Psychiatry 2000; 57:794–801Crossref, Google Scholar
38 Gorman, J.M., et al., Merging the cognitive behavioral and psychopharmacological paradigms in comparative studies: controversies, issues, and some solutions. Psychopharmacol Bull 2001; 35(2):111–124Google Scholar
39 Ackerman DL, Greenland S, Bystritsky A, Morgenstern H, Katz RJ: Predictors of treatment response in obsessive-compulsive disorder: multivariate analyses from a multicenter trial of clomipramine. J Clin Psychopharmacol 1994; 14:247–254Crossref, Google Scholar
40 Roy-Byrne PP, Sherbourne CD, Craske MG, Stein MB, Katon W, Sullivan G, Means-Christensen A, Bystritsky A: Moving treatment research from clinical trials to the real world. Psychiatr Serv 2003; 54:327–332Crossref, Google Scholar
41 Hollander E, Bienstock CA, Koran LM, Pallanti S, Marazziti D, Rasmussen SA, Ravizza L, Benkelfat C, Saxena S, Greenberg BD, Sasson Y, Zohar J: Refractory obsessive-compulsive disorder: state-of-the-art treatment. J Clin Psychiatry 2002; 63(suppl 6):20–29Google Scholar
42 Liebowitz MR: Update on the diagnosis and treatment of social anxiety disorder. J Clin Psychiatry 1999; 60(suppl 18):22–26Crossref, Google Scholar
43 Bystritsky A, Liberman RP, Hwang S, Wallace CJ, Vapnik T, Maindment K, Saxena S: Social functioning and quality of life comparisons between obsessive-compulsive and schizophrenic disorders. Depress Anxiety 2001; 14:214–218Crossref, Google Scholar
44 Greenberg BD, Price LH, Rauch SL, Friehs G, Noren G, Malone D, Carpenter LL, Rezai AR, Rasmussen SA: Neurosurgery for intractable obsessive-compulsive disorder and depression: critical issues. Neurosurg Clin N Am 2003; 14:199–212Crossref, Google Scholar
45 Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, Kessler RC: Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA 1998; 280:1569–1575Crossref, Google Scholar
46 Kessler RC: The epidemiology of pure and comorbid generalized anxiety disorder: a review and evaluation of recent research. Acta Psychiatr Scand Suppl 2000; 406:7–13Google Scholar



