Diagnostic Criteria for Complicated Grief Disorder
Abstract
Objective: Some prolonged and turbulent grief reactions include symptoms that differ from the DSM-IV criteria for major depressive disorder. The authors investigated a new diagnosis that would include these symptoms. Method: They developed observer-based definitions of 30 symptoms noted clinically in previous longitudinal interviews of bereaved persons and then designed a plan to investigate whether any combination of these would serve as criteria for a possible new diagnosis of complicated grief disorder. Using a structured diagnostic interview, they assessed 70 subjects whose spouses had died. Latent class model analyses and signal detection procedures were used to calibrate the data against global clinical ratings and self-report measures of grief-specific distress. Results: Complicated grief disorder was found to be characterized by a smaller set of the assessed symptoms. Subjects selected by an algorithm for these symptom patterns did not significantly overlap with subjects who received a diagnosis of major depressive disorder. Conclusions: A new diagnosis of complicated grief disorder may be indicated. Its criteria would include the current experience (more than a year after a loss) of intense intrusive thoughts, pangs of severe emotion, distressing yearnings, feeling excessively alone and empty, excessively avoiding tasks reminiscent of the deceased, unusual sleep disturbances, and maladaptive levels of loss of interest in personal activities.
Normal grief can combine distressing moods and turbulent, even confusing thoughts. It is assumed that equilibrium will return eventually as a result of mourning processes, but extremes that may impair functional capacity to a psychopathological degree may occur. Because of this range from normal to abnormal distress after loss, clinicians have debated the possible inclusion of complicated and prolonged grief reactions in a nosology of mental disorders (1–3). The result of the present lack of such a diagnosis is that many longitudinal studies of bereaved populations have assessed pathology only or mainly as signs and symptoms of major depressive disorder (4–6). This strategy has been useful because loss events are associated with increasing rates of major depressive disorder (7, 8), but the focus on major depression has probably led to underestimation of the frequency of increased psychopathology after the death of a significant other (9–15).
Complicated grief disorders may include symptoms such as intrusive images, severe pangs of emotion, denial of implications of the loss to the self, and neglect of necessary adaptive activities at work and at home (16–18). Complicated grief in response to a loss may be distinguished from a chronic adjustment disorder by the specificity of the etiologic event, as well as grief-specific symptoms. In this study, we attempted to identify such symptoms and studied how they might cohere over time. Our aim was to provide empirical criteria for diagnosing complicated disorders of grief.
Scientific discussions for the construction of DSM-IV included the topic of pathological grief (16). The DSM-IV subcommittee on posttraumatic stress disorder (PTSD) suggested that a separate category of diagnoses for stress response syndromes be established. The set would have combined several diagnoses in which stressor events precipitate symptom formation: pathological or complicated grief, acute stress disorder, PTSD, dissociative amnesia, and adjustment disorder. Higher-level decisions rejected the suggestion of a separate grouping and the proposed diagnosis of complicated or pathological grief, the latter because of lack of empirical work on its constituent symptoms.
Empirical data have been published since this decision was made. In this journal Prigerson and colleagues (3) reported a distinction between grief psychopathology and depression in their study of 82 elderly widowed individuals, where self-report measures of symptoms were used. The salient symptoms of complicated grief included preoccupation with thoughts of the deceased, disbelief, feeling stunned, and lack of acceptance of the death; high levels of these symptoms were associated with enduring functional impairments, yet they were distinct from depressive symptoms. These authors concluded that complicated grief reactions represent “a unique disorder deserving of specialized treatment.”
As reviewed elsewhere (10, 11, 17–21), other clinical studies have made similar distinctions between normal distress during mourning and complicated or pathological grief. The importance of prior vulnerabilities to depression, personality problems, and lower socioeconomic status has been established (22–28). These complex associations do not mitigate the need for a new axis I symptom-based diagnosis.
Our belief in the need for a diagnosis is based on longitudinal clinical investigations. In studies of individuals seeking brief therapy after the death of a loved one, we found that many prolonged grief reactions were characterized by three sets of symptoms: intrusions, avoidances, and failures to adapt to the specific loss event (29). By developing operational definitions of these three sets of symptoms, we designed a module for use in a clinical interview, following the methods used in the Structured Clinical Interview for DSM-III-R—Non-Patient Edition (SCID-NP) (30). Using the SCID-NP plus the new module in a group of bereaved subjects studied 6 months and 14 months after the loss of a spouse, we predicted 1) that a salient diagnostic algorithm would be found upon statistical analyses of the data, 2) if so, that some subjects would have a complicated grief disorder but not a current major depressive disorder, and 3) that individuals with a lifetime history of major depressive disorder would be more likely to have a current diagnosis of major depressive disorder, a complicated grief disorder, or both.
Method
Bereaved subjects were evaluated by means of structured clinical interviews and self-report rating scales 6 months and 14 months after the death of their spouse or long-term domestic partner. Interviewers, trained in the use of the SCID-NP, added questions related to 30 possible symptoms of complicated grief. They rated each symptom, made SCID-NP diagnoses, and provided an overall rating of complicated grief. The subjects completed self-report measures.
A latent class model analysis (explained below) related grief symptom ratings from the interview to the clinician’s overall rating of complicated grief and to two self-report measures specific to grief distress, to derive a consensus measure (“gold standard”) of complicated grief. This was then used in signal detection analyses to select specific and sensitive grief symptoms as candidates for diagnostic criteria. When we had selected the diagnostic criteria, the frequency of the diagnosis was compared with current and lifetime diagnoses of major depressive disorder in all subjects.
Individuals who had experienced the death of a spouse when they were between the ages of 21 and 55 years were recruited through notices placed in the local newspaper. This nonelderly age range was used to increase the likely frequency of symptoms, since past research indicates more distress in younger persons who experience conjugal loss, especially if the loss is relatively sudden, rather than gradual and expected as a consequence of terminal illness.
Volunteers who entered the study had been either married or living domestically and intimately with their deceased partner for at least 3 years. Persons with any recent physical or mental disorder requiring hospitalization, those with eating disorders, and those with substance abuse were excluded. After all procedures were fully explained, subjects gave written informed consent.
Volunteer study groups do not usually represent an entire population and are often enriched with subjects experiencing particularly intense responses, who for this reason are interested in the study. This suited our purpose, as we wanted to increase the likelihood of psychopathological symptoms. In using such a method, we planned for a high “case-finding” yield, but consequently our data do not permit extrapolation of the prevalence of complicated grief in a bereaved population.
We evaluated 90 subjects 6 months after their loss of a long-term domestic partner. This group included 29 male and 61 female subjects, of whom 7.8% had a high school education or less, 85.6% had some college education, and 6.7% had graduate education. Seventy of these subjects participated in a repeat evaluation 14 months after their loss. The subjects who remained in the study did not differ significantly in demographic characteristics or symptoms at 6 months from the 20 subjects who were lost by attrition between the two evaluations.
Three advanced clinical trainees took and passed an SCID-NP training course. Using procedures similar to those of the SCID-NP, they were trained to investigate and rate the 30 symptoms of an SCID-NP-type module for grief-related symptoms.
Procedures
Respondents who met the criteria for inclusion in the study on the basis of a telephone screening were mailed preliminary consent forms and a self-report battery. When the packet was returned, the structured interview for diagnostic evaluation was scheduled. The SCID-NP, supplemented by the analogous module of 30 grief symptoms, was conducted by a clinical interviewer who made all relevant axis I DSM-IV diagnoses, rated each of the grief symptoms, and gave a global rating of the presence or absence of a pathological degree of grief response. The grief symptoms are listed in table 1. Each symptom and the global rating of complicated grief were scored on 7-point Likert scales: 0–1=absent, false, or minimal presence; 2–4=subthreshold or subclinical manifestation; 5–7=threshold or true, with a maladaptive manifestation. These definitions correspond to the SCID-NP rating system: our 0–1 ratings to SCID-NP rating 1; our 2–4 ratings to SCID-NP rating 2; and our 5–7 ratings to SCID-NP rating 3.
The SCID-NP interviews were videotaped. Twenty-five were reviewed and scored by a clinical interviewer. Interobserver reliability on rating the 30 grief symptoms was satisfactory (kappa=0.78). The 30 symptoms were divided into three clinically derived categories: avoidance, intrusion, and failure to adapt. These were found, upon analyses of the data, to have satisfactory levels of internal consistency: 1) avoidance of thoughts and experiences related to the deceased (alpha coefficient=0.58) included episodes of numbing emotion and inhibiting themes that could remind the subject of the death; 2) intrusion (alpha coefficient=0.52) included undesired, unbidden images of the deceased and frequent nightmares; and 3) failure to adapt to the loss (alpha coefficient=0.49) included extreme avoidance of new relationships and difficulty in returning to a daily routine of life activities.
The self-report battery included the following two instruments.
1. The Texas Revised Inventory of Grief (31) is an established self-administered questionnaire that measures grief response in reference to a specified deceased person. A 5-point scale is used to indicate degree of endorsement of each of 13 items.
2. The Reaction to Loss Inventory, developed by Horowitz and Field, is a new and as-yet unpublished self-administered questionnaire with 34 items that assess current symptoms, functional capacity, sense of identity, sense of relationship to the person who has died, and control of emotion related to the loss. The Reaction to Loss Inventory reduces many experiences, such as the intrusive and avoidance items found in the earlier Impact of Event Scale (32), to fewer items. The subject endorses each item on a 5-point scale ranging from “no experience” to “a high level of experience” within the last week.
Sstatistical analyses
The first step in identifying possible diagnostic criteria for complicated grief was to select a criterion against which to compare each of the 30 newly developed candidate items. This was accomplished by applying latent class analysis. Since there are various applications for latent class models, and these are only recently coming into use in psychiatric studies, we review briefly the methodological advantages and procedures that influenced us to proceed with data analysis in this fashion. Latent class models have been used previously to examine the congruity among potential diagnostic “gold standards” for other psychiatric disorders, such as schizophrenia (33, 34), mania (35), and, most recently, autism in the DSM-IV field trials (36). Estimates of sensitivity and specificity for various sets of potential diagnostic criteria are obtained by modeling the data with the use of maximum likelihood technique computed relative to the latent standard or classification. An expression is obtained for the probability of an individual’s having any of the combinations of observed results on the possible tests of the diagnosis. These expressions are made up of components associated with each of the latent classes that might characterize the subject (i.e., really having, or really not having, the diagnosis). The first component of the probability is associated with a true positive; the second with a false positive. The two components add up to an overall probability of a positive result for a subject of latent positive status. Parallel probability calculations are made for individuals with negative test results. The probability calculations make up the likelihood for the whole data set. The prevalence of the disorder and the sensitivity and specificity of the criteria are estimated from the data. Iterative numerical maximization of the likelihood for all the data leads to the maximum likelihood estimates of these parameters. The latent class model method used in this study is reviewed by Walter and Irwig (37); the program used for the calculations was developed by Szatmari and Walter (unpublished).
The data analysis assumes that the multiple measures of complicated grief being used should overlap for subjects identified as having positive positive, false positive, negative negative, and false negative diagnoses, that iterative convergence will estimate the latent class, and that the actual measure which most closely (singularly) corresponds to this latent class is the best estimator of the phenomenon. After the latent class model is applied to empirical selection of a “gold standard” against which a set of diagnostic criteria may be calibrated, signal detection analyses can be applied to select specific items to serve as diagnostic criteria.
The mathematics of the signal detection method has been described for psychiatric applications (38) and has already been used to model DSM-like sets of diagnostic criteria (39–41). In the signal detection method, it is possible to enter a series of predictors (possible diagnostic criteria) simultaneously and then to pick the predictors that correspond to the highest total predictive value, while monitoring the need to identify further predictors for cases that have not yet been diagnosed by the existing algorithm. Signal detection simultaneously selects diagnostic criteria that yield the highest total predictive value while continuing to select further diagnostic criteria that keep sensitivity and specificity best balanced. In addition, signal detection yields an algorithm consisting of structured “and/or” rules that models procedures typically used in the DSMs and easily used by clinicians.
Signal detection was selected for this study because it enables selection of “whole” items, which is clinically much more useful than a logistic regression approach, for example, which would produce a list of weighted predictor variables. It should be noted, however, that both the latent class model and signal detection approaches are forms of exploratory data analysis, and as such they do not allow testing of “trend” significance but, rather, serve to develop models. In this case, the goal was to produce a model set of criteria for complicated grief disorder that may be tested in future research on independent samples.
Results
Table 1 shows the percentages of subjects with severe grief symptoms at 6 months and 14 months and notes the symptoms that showed significant decreases over this time interval. Within each category (avoidance, intrusion, and failure to adapt), symptoms are ranked by frequency from most likely to least likely at first evaluation. Table 1 also contains the mean rating by the interviewer of the severity of each symptom. Some symptoms from each category were present in more than one-half of the subjects at the first evaluation. Both frequency and intensity declined with time, as was expected. Unbidden memories of the deceased, in the intrusion category, was both the most frequent and the most severe symptom at both evaluation times.
Latent class model analyses
Separate latent class model analyses were constructed for data on the subjects 6 months and 14 months after bereavement to determine whether indicators of complicated grief more than a year after loss were stable over that time period. Data entered into the latent class models were four potential “gold standards” for measuring pathological grief. The 6-month data were 1) an above-median total score on the Texas Revised Inventory of Grief (median=50); 2) an above-median total score on the Reaction to Loss Inventory (median=64); 3) an above-median number of symptoms scored in the “complicated grief” range (i.e., ≥5) by clinical interviewers (median=6); and 4) the clinician’s global rating of the presence or absence of pathological grief after the diagnostic interview. Data were divided in this way to reflect nonuniform distributions suggesting a “high” cluster of subjects who could be hypothesized clinically to have markedly more severe symptoms. Data were dichotomized because of the requirements of latent class model analysis for nominal data. Table 2 shows how each of these possible “gold standards” compared to the “latent” standard 6 months and 14 months after bereavement. The comparison is expressed in terms of false negative and false positive rates, as well as the sensitivity and specificity of each standard to the latent model.
The results at 6 months indicated that the number of clinician-rated (SCID-NP) severe grief symptoms (five symptoms or more in a subject) was the closest reflection of the latent model, misclassifying only 3% of cases. A parallel analysis was conducted for the 14-month data (although median scores, and therefore cutoffs, varied from the 6-month data [Texas Revised Inventory of Grief, median=41; Reaction to Loss Inventory, median=57; severe grief symptoms, median=5]). At 14 months, the number of severe grief symptoms also proved to be the best reflection of the latent class model, accurately classifying 100% of cases.
Using the above-median versus below-median cutoff for the number of SCID-NP interview severe grief symptoms as the “gold standard” for detecting complicated grief, we then calculated the sensitivity and specificity of each item 6 months and 14 months after bereavement. The results (table 3) show that most of these symptoms had lower sensitivity and higher specificity, indicating that while any one symptom was relatively infrequent, most symptoms, when endorsed, tended to be endorsed by the subjects who reported multiple symptoms of complicated grief. Between 6 and 14 months after the loss, the sensitivity of items generally decreased and the specificity increased further, indicating that when symptoms were endorsed at 14 months, they were even more exclusively endorsed by those with prolonged problems of complicated grief, as indicated by the “gold standard” derived by the latent class model.
Signal detection analyses
The latent class model analysis identified having an above-median number of severe grief symptoms according to the SCID-NP interview as our “gold standard” for assessing complicated grief. We then used signal detection to identify which specific criteria from among the 30 canvassed by the clinician interviewers with the SCID-NP might best define a diagnosis. These signal detection analyses can yield a set of criteria that are linked by “and/or” rules.
In the analysis 6 months after loss, the signal detection algorithm produced a diagnostic algorithm for complicated grief that consisted of either of the two symptoms with the highest specificity plus either of the two symptoms with the highest sensitivity. Thus, a subject with symptoms that (at least) included a low interest in important activities or strong spells of emotion, as well as unbidden memories or feelings of aloneness or emptiness, would be diagnosed by the computer on the basis of these symptoms as having complicated grief 6 months after loss (sensitivity=0.80; specificity=0.85; total predictive value=0.88). That is, 88% of the subjects identified by the latent class model analysis as having the most severe grief symptoms 6 months after loss experienced one of the above-mentioned combinations of symptoms. It is interesting that these criteria-like symptoms stem from each of the clinically derived symptom groupings of avoidance, intrusion, and failure to adapt. Different individuals and individuals in different phases of response to stress may exhibit different signs of maladaptive grief processing, as suggested by the clinical impressions and empirical findings on subtypes of complicated grief cited earlier. At 14 months, subjects who experienced a strong yearning for the deceased, continued feelings of aloneness or emptiness, trouble sleeping, or strong avoidance of reminders of the deceased would be found by a computer following this algorithm to have complicated grief (sensitivity=1.00; specificity=0.71; total predictive value=0.86). This pattern indicates that the symptoms of grief that were most severe at 6 months were not necessarily the ones most manifest at 14 months, but, as indicated below, the group of individuals showing severe symptoms remained quite stable over time.
Diagnoses
Although our results suggest that it may be possible to detect complicated grief at 14 months by the presence of just one or two severe grief symptoms, all subjects who met this criterion experienced a multiplicity of symptoms, with the most prominent symptoms being significantly intercorrelated. It was felt that while it was statistically justified to base the diagnosis on one of the four severe grief symptoms identified by signal detection at 14 months, a conservative, clinician-based, and DSM-like approach would be needed to formulate a set of diagnostic criteria with a minimum of three of these symptoms. The fact that these symptoms are intercorrelated justifies such an approach statistically.
We propose that three or more of seven possible symptoms must be currently intensely present for a diagnosis of complicated grief disorder to be made, as shown in appendix 1. The seven symptoms are those identified in the 6-month and 14-month signal detection studies. The exploratory nature of the data analyses conducted here is another reason to tend toward overinclusion rather than exclusion of potentially informative diagnostic criteria. In addition, the inclusion of more rather than fewer symptoms to reach the diagnostic threshold is likely to further improve specificity (which was 78%) while likely lowering sensitivity only marginally because of the intercorrelation among criteria.
We applied these criteria to arrive at the frequency of the proposed diagnosis. We found that 41% (N=29) of the 70 subjects met the criteria for complicated grief disorder, and 21% (N=6) of these 29 subjects—about one-fifth—had a concurrent diagnosis of major depressive disorder, while 79% did not. Only a slightly higher proportion, 31% (N=9), of these 29 subjects had had a diagnosis of current major depressive disorder at the 6-month evaluation. However, as we hypothesized earlier, many of these subjects with complicated grief disorder (79%, N=23) met the SCID=NP criteria for a previous lifetime diagnosis of major depressive disorder. Of the 41 subjects (59%) without complicated grief disorder at 14 months, 41% (N=17) met the SCID-NP criteria for a lifetime diagnosis of major depressive disorder. We concluded that previous vulnerability to depression predisposed these subjects to formation of complicated grief disorder. Among the 41 subjects not diagnosed as having a complicated grief disorder at 14 months, none received a current diagnosis of major depressive disorder, and only 10% (N=4) had received a current diagnosis of major depressive disorder 6 months after loss.
The rate of lifetime major depressive disorder among the 70 subjects, judged by clinician interviewers at 14 months after loss, was significantly associated with the current diagnosis of complicated grief disorder made by these interviewers (χ2=1.8.0, df=1, p≤0.0001). These data replicate earlier research showing that higher grief distress occurs in subjects with a history of depressive disorders (6). Our subjects were also assessed by SCID-NP criteria for anxiety disorders. The anxiety disorders were few and had no relevant associations with complicated grief disorder. Although 40% (N=28) of our subjects gave a lifetime history of an anxiety disorder, these past experiences failed to be significantly associated with a current diagnosis of complicated grief disorder (χ2=3.0, df=l, p≤0.10).
Discussion
From a broad range of 30 possible grief symptoms assessed 6 months and 14 months after a major loss, it was possible to extract seven that could serve as potential diagnostic criteria for complicated grief disorder with a high degree of sensitivity and specificity. The frequency of these symptoms declined significantly in the interval between 6 months and 14 months after the death of a significant other, but more than 1 year after the loss some subjects still had many symptoms. At that time, 14 months after the loss, 41% of the subjects received a proposed diagnosis of complicated grief disorder. Only one-fifth of these subjects also received a concurrent diagnosis of major depressive disorder. On the other hand, both current complicated grief disorder and current major depressive disorder were strongly predicted by a lifetime history of major depressive disorder. Vulnerability in terms of preloss issues of biological temperament, psychological character, and social context is likely for complicated grief disorder as well as major depressive disorder.
The criteria we suggest for complicated grief disorder presently group individuals with prolonged and severe grief responses together into one category, yet clinical experiences have led to reports of various possible subtypes of symptomatic presentation after prolonged and unresolved mourning (20–23). People frozen in mourning might be grouped with people flooded with sadness, rage, and disturbances in a sense of coherent identity if our criteria (appendix 1) are used. As we see it, this can be handled with multiaxial diagnoses, adding axis 11 personality disorder categories to make distinctions between subgroups. under a single axis I symptom diagnosis of complicated grief disorder or major depressive disorder.
Conclusions
Does DSM-IV already have enough categories? As we have seen, major depressive disorder does not adequately cover the symptom picture. Adjustment disorder is too nonspecific to serve as the relevant additional category. The event criteria for PTSD exclude some common loss-induced reactions from use of this diagnosis. A new diagnosis could help clinicians to formulate and treat pathology that is not adequately covered at present in our nosology in DSM-IV.
Appendix 1. Proposed Diagnostic Criteria for Complicated Grief Disorder
A. Event criterion: prolonged response criterion
Bereavement (loss of a spouse, other relative, or intimate partner) at least 14 months ago (12 months is avoided because of possible intense turbulence from an anniversary reaction)
B. Signs and symptoms criteria
In the last month, any three of the following seven symptoms with a severity that interferes with daily functioning
Intrusive symptoms
| 1. | Unbidden memories or intrusive fantasies related to the lost relationship | ||||
| 2. | Strong spells or pangs of severe emotion related to the lost relationship | ||||
| 3. | Distressingly strong yearnings or wishes that the deceased were there | ||||
Signs of avoidance and failure to adapt
4. Feelings of being far too much alone or personally empty
5. Excessively staying away from people, places, or activities that remind the subject of the deceased
6. Unusual levels of sleep interference
7. Loss of interest in work, social, caretaking, or recreational activities to a maladaptive degree
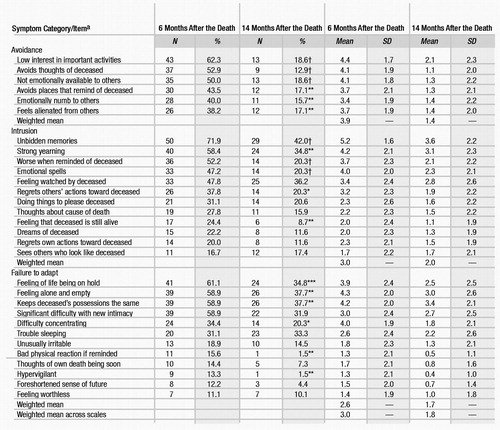 |
Table 1. Symptoms of Complicated Grief in 70 Subjects 6 Months and 14 Months After the Death of a Spouse
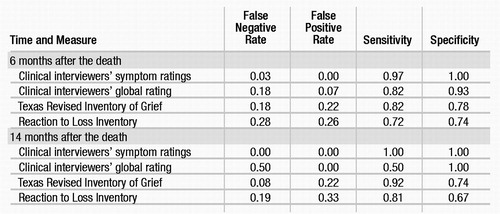 |
Table 2. Latent Class Model Analyses of Four Potential Measures of Complicated Grief Administered to 70 Subjects 6 Months and 14 Months After the Death of a Spouse
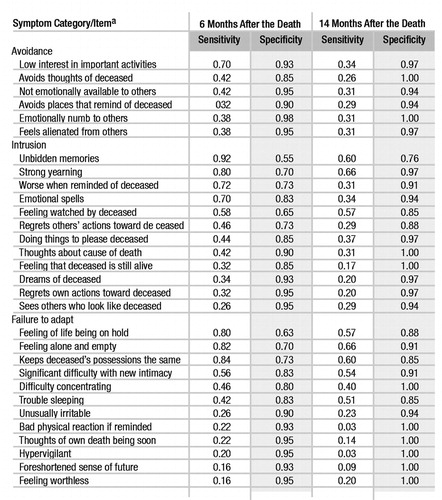 |
Table 3. Sensitivity and Specificity of Grief Symptoms in 70 Subjects 6 Months and 14 Months After the Death of a Spouse
1 Horowitz MJ: Stress Response Syndromes, 2nd ed. Northvale, NJ, Jason Aronson, 1986Google Scholar
2 Biederman M: Grief: normal and pathological variants (editorial). Am J Psychiatry 1995; 152:1–4Crossref, Google Scholar
3 Prigerson HG, Frank E, Kasl SV, Reynolds CF III, Anderson B, Zubenko GS, Houck PR, George CJ, Kupfer DJ: Complicated grief and bereavement-related depression as distinct disorders: preliminary empirical validation in elderly bereaved spouses. Am J Psychiatry 1995; 152:22–30Crossref, Google Scholar
4 Kim K, Jacobs S: Pathologic grief and its relationship to other psychiatric disorders. J Affect Disord 1991; 21:257–263Crossref, Google Scholar
5 Bruce ML, Kim K, Leaf PJ, Jacobs S: Depressive episodes and dysphoria resulting from conjugal bereavement in a prospective community sample. Am J Psychiatry 1990; 147:608–611Crossref, Google Scholar
6 Zisook S, Shuchter SR: Depression through the first year after the death of a spouse. Am J Psychiatry 1991; 148:1346–1352Crossref, Google Scholar
7 Kessler RC, Kendler KS, Heath A, Neale MC, Eaves LJ: Social support, depressed mood, and adjustment to stress: a genetic epidemiologic investigation. J Pers Soc Psychol 1992; 62:257–272Crossref, Google Scholar
8 Adler N, Boyce T, Chesney MA, Cohen S Folkman S. Kahn RL, Syme SL: Socioeconomic status and health: the challenge of the gradient. Am Psychol 1994; 49:15–24Crossref, Google Scholar
9 Clayton PJ: Mortality and morbidity in the first year of widowhood. Arch Gen Psychiatry 1974; 30:747–750Crossref, Google Scholar
10 Jacobs S, Hansen F, Kasl S, Ostfeld A, Berkman L, Kim K: Anxiety disorders during acute bereavement: risk and risk factors. J Clin Psychiatry 1990; 51:269–274Google Scholar
11 Stroebe M, Stroebe W: Does “grief work” work? J Consult Clin Psychol 1991; 59:479–482Crossref, Google Scholar
12 Downey G, Silver RC, Wortman CB: Reconsidering the attribution-adjustment relation following a major negative event: coping with the loss of a child. J Pets Soc Psychol 3990; 59:925–940Google Scholar
13 Raphael B, Middleton W: What is pathologic grief? Psychiatr Annals 1990; 20:304–307Crossref, Google Scholar
14 Lieberman MA: A reexamination of adult life crises: spousal loss in mid- and late life, in The Course of Life, vol 6: Late Adulthood. Edited by Pollock GH, Greenspan SL. Madison, Conn, International Universities Press, 1993, pp 69–119Google Scholar
15 Lundin T: Long-term outcome of bereavement. Br J Psychiatry 1984; 145:424–428Crossref, Google Scholar
16 Marwit S: DSM-III-R, grief reactions, and a call for revision. Professional Psychol Res Practice 1991; 22:75–79Crossref, Google Scholar
17 Horowitz MJ: A model of mourning: change in schemas of self and other. J Am Psychoanal Assoc 1990; 38:297–324Crossref, Google Scholar
18 Horowitz MJ: Post-traumatic stress disorder: psychosocial aspects of the diagnosis. Int J Merit Health 1990; 19:21–36Google Scholar
19 Freud S: Inhibitions, symptoms and anxiety (1926 [1925]), in Complete Psychological Works, standard ed, vol 20. London, Hogarth Press, 1959, pp 77–175Google Scholar
20 Lindemann E: Symptomatology and management of acute grief. Am J Psychiatry 1944; 101:141–148Crossref, Google Scholar
21 Deutsch H: The absence of grief. Psychoanal Q 1937; 6:12–22Crossref, Google Scholar
22 Klein M: Contributions to Psychoanalysis. London, Hogarth Press, 1948Google Scholar
23 Parkes CM, Weiss R: Recovery From Bereavement. New York, Basic Books, 1983Google Scholar
24 Mendes de Leon CF, Karl SV, Jacobs S: A prospective study of widowhood and changes in symptoms of depression in a community sample of the elderly. Psychol Med 1994; 24:613–624Crossref, Google Scholar
25 Lehman DR, Wortman CB, Williams AF: Long-term effects of losing a spouse or child in a motor vehicle crash. J Pets Soc Psychol 1987; 52:218–231Crossref, Google Scholar
26 Zisook S, Schneider D, Schucter S: Anxiety and bereavement. Psychiatr Med 1990; 8:583–596Google Scholar
27 Zisook S, Shuchter S: Early psychological reaction to the stress of widowhood. Psychiatry 1991; 54:320–333Crossref, Google Scholar
28 Nuss WS, Zubenko GS: Correlates of persistent depressive symptoms in widows. Am J Psychiatry 1992, 149:346–351Crossref, Google Scholar
29 Horowitz MJ, Marmar C, Krupnick J, Wilner N, Kaltreider N, Wallerstein R: Personality Styles and Brief Psychotherapy. New York, Basic Books, 1984Google Scholar
30 Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-III-R-Non-Patient Edition (SCID-NP, Version 1.0). Washington, DC, American Psychiatric Press, 1990Google Scholar
31 Faschingbauer TR: Texas Revised Inventory of Grief Manual. Houston, Honeycomb, 1981Google Scholar
32 Horowitz MJ, Wilner N, Alvarez W: Impact of Event Scale: a measure of subjective stress. Psychosom Med 1979; 41:209–218Crossref, Google Scholar
33 Young MA, Tanner MA, Meltzer HY: Operational definitions of schizophrenia: what do they identify? J Nerv Ment Dis 1982; 171:443–447Crossref, Google Scholar
34 Young MA: Evaluating diagnostic criteria: a latent class paradigm. J Psychiatr Res 1983; 17:285–296Crossref, Google Scholar
35 Young MA, Abrams R, Taylor MA, Meltzer HY: Establishing diagnostic criteria for mania. J Nerv Ment Dis 1983; 171:676–682Crossref, Google Scholar
36 Szatmari P, Volkmar FR, Walter S: Evaluation of diagnostic criteria for autism using latent class models. J Am Acad Child Adolesc Psychiatry 1995; 34:216–222Crossref, Google Scholar
37 Walter SD, Irwig LM: Estimation of test error rates, disease prevalence and relative risk from misclassified data: a review. J Clin Epidemiol 1988; 9:923–937Crossref, Google Scholar
38 Kraemer HC: The methodological and statistical evaluation of medical tests: the dexamethasone suppression test in psychiatry. Psychoneuroendocrinology 1987; 12:411–427Crossref, Google Scholar
39 Hsiao JK, Bartko JJ, Potter WZ: Diagnosing diagnoses: receiver operating characteristic methods and psychiatry. Arch Gen Psychiatry 1989; 46:664–667Crossref, Google Scholar
40 Siegel B, Vukicevic J, Elliott GR, Kraemer HC: An assessment of the DSM-III-R criteria for autistic disorder using signal detection theory. J Am Acad Child Adolesc Psychiatry 1989; 28:542–548Crossref, Google Scholar
41 Siegel B, Vukicevic J, Spitzer RL: Using signal detection theory to revise DSM-III: reanalysis of the DSM-III-R national field trials for autistic disorder. J Psychiatr Res 1990; 24:293–311Crossref, Google Scholar



