Psychiatric Reaction Patterns to Imipramine
Abstract
(Reprinted with permission from the American Journal of Psychiatry 1962; 119:432–438)
Clinical psychiatric experience demonstrates a wide range of variation in behavioral responses to physiological therapies. Present techniques of evaluating therapies by global improvement scores, imprecise diagnostic classification, and target symptoms abstracted from their context were felt to be methodologically inadequate. Following our experience in describing the behavioral reaction patterns to convulsive (4) and phenothiazine (6) therapies, a similar analysis of the data derived from imipramine (Tofrānil) therapy was undertaken. In this report various patterns of behavioral response to imipramine are described; and the relationship to such factors as age, sex, pretreatment behavioral pattern, hospital diagnosis, and hospital discharge evaluation are assessed.
METHOD
Hillside Hospital is a 196-bed, open ward, voluntary psychiatric facility for the treatment of patients with early and acute mental disorders whose stay is independent of their ability to pay. All patients are seen in individual psychotherapy, with the expectation that psychotherapy should be given a trial prior to other measures. Somatic therapies are employed by joint decision of the resident therapist and supervising psychiatrist, with the management of medication restricted to the research staff.
Before starting medication each patient is interviewed by a research psychiatrist. During drug therapy the patient's response is assessed in weekly interviews with both the patient and ward personnel, reviewing changes in mental status and hospital adjustment. In biweekly conferences with the psychiatric resident and his supervisor the patient's progress in psychotherapy, affective and symtomatic state, utilization of hospital facilities, and social and familial relationships are discussed.
When it was evident that the standard diagnostic nomenclature was of little use in categorizing behavioral reactions to drugs, and that psychodynamic formulations lacked predictive clarity, it was decided to derive a descriptive behavioral typology for each agent studied. The detailed longitudinal research records were reviewed and a summary statement concerning the patient's behavioral reaction during treatment was made. The patients were categorized on the basis of changes in symptoms, affect, patterns of communication and participation in psychotherapy and social activity. In each category the drug reaction was the determining feature. While no attention was paid at this point to the patient's pretreatment behavioral patterns, except as relevant to the perceived changes, inspection of these groups showed that not only did the patients share similar behavioral changes with drug therapy, but that they also showed similar behavioral pretreatment characteristics.
For certain patients no discernible change in behavior was observed. It was possible to characterize these subjects by their pretreatment behavioral patterns alone, and these patterns did not occur among those groups showing an imipramine effect.
Treatment was begun orally at 75 mg. daily and usually increased each week in 75 mg. steps, to a modal maximum of 300 mg./day in 80% of the patients.
Between October 1958 and July 1961, 215 patients received imipramine. During the early use of the drug it had not been firmly established that an adequate trial of medication required at least three to four weeks. Therefore, 13 patients who had not responded within two weeks had the medication discontinued. In retrospect, these patients had not received an adequate course of imipramine. Records were incomplete in 3 patients and at the time of writing 19 patients had not yet been discharged. These 35 patients are not included in the data analysis.
Of the 180 remaining patients, 67 were diagnosed as psychoneurotic depressive reactions, involutional melancholia, manic-depressive reaction, or psychotic depressive reaction. Schizophrenia in various subtypes was diagnosed in 102 patients. Ten patients received diagnoses of psychoneurosis or personality disorder, and one patient was diagnosed as chronic brain syndrome. Since the use of specific affective or schizophrenic subtypes was not discriminating in our analyses, the subgroups were combined.
There were 58 men and 122 women reflecting the sex distribution of the hospital. In this population schizophrenia was diagnosed most commonly in patients below 30 years of age, and affective disorders in patients above 40. However, there was no association of diagnosis or age, with sex.
Two methods of evaluating behavioral change were used—a medication management index and a discharge evaluation. The medication management index was based on the various patterns of medication use, reflecting the decision of the therapist as to the value of the medication to the patient—actions proverbially speaking louder than words. Eight patterns were observed, three implying a favorable and five an unfavorable evaluation. Favorable medication management evaluations by the therapist were seen in 115 subjects (68%) and included patients discharged to the community with the recommendation to continue on imipramine therapy (68 patients); patients discharged to the community after imipramine was discontinued with a clinical note that it had accomplished its therapeutic goals and without other somatic therapy prior to discharge (28 patients); and patients discharged to the community to continue imipramine with concurrent phenothiazine medication (19 patients).
Patterns reflecting a therapist's negative evaluation of the behavioral response were seen in 65 patients (32%). These included imipramine discontinued and subsequent treatment with phenothiazines or convulsive therapy prior to discharge (38 patients); imipramine discontinued with the clinical note that it was ineffective and the patients discharged without further somatic treatment (19 patients); and the abrupt ending of imipramine treatment by discharge to another inpatient facility (5 patients), suicide (1 patient), or leaving the hospital against medical advice (2 patients). In this report, the first three patterns of medication use will be referred to as “favorable medication management” and the latter five as “unfavorable medication management.”
In addition, at discharge each patient is given a summary rating as “recovered,” “much improved,” “improved,” or “unimproved” by the staff. This discharge rating is a guide to the effect of hospitalization. It is not the same as the medication management index since other treatment measures may have been interposed after the imipramine treatment. However, this measure will aid in placing the imipramine effects within the context of the general hospital psychiatric treatment. In view of the small number of patients considered “recovered,” this category was combined with “much improved.”
The chi square method of statistical analysis was used and all stated findings are at the .05 level of confidence or better.
RESULTS
General medication response.
The behavioral effect of imipramine required two to three weeks to become evident for the majority of cases. An occasional case responded within a few days, and one case responded after 5 weeks of medication.
Complaints of sweating, tremulousness, dry mouth, and constipation were frequent, but interfered little with the treatment course. Two patients developed grand mal epileptic attacks (at 300 mg./day and 450 mg./day) which ceased with medication reduction or termination. There was one instance of pseudo-tumor cerebri (2) and one instance of agranulocytosis. Both occurred during the concomitant administration of phenothiazines, and may have been unrelated to imipramine.
In 22 of 26 patients receiving imipramine in 300 mg. daily doses for periods of two months or more, and rapidly withdrawn from the drug, the occurrence of a physiological withdrawal syndrome of nausea, vomiting, headache, giddiness, coryza, chills, weakness, fatigue and musculoskeletal pain was documented (7). These symptoms were related to the length of treatment and the abruptness of the withdrawal. It was also observed that these symptoms could be minimized by gradual withdrawal over one to two weeks.
Patterns of behavioral response.
The relation of the behavioral response patterns to medication management, hospital discharge evaluation, age, sex and diagnosis are presented in Tables 1 and 2.
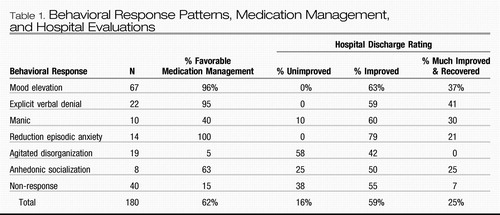 |
Table 1. Behavioral Response Patterns, Medication Management, and Hospital Evaluations
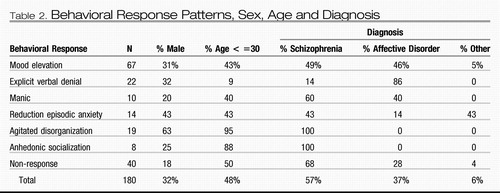 |
Table 2. Behavioral Response Patterns, Sex, Age and Diagnosis
1. MOOD ELEVATION RESPONSE
Before treatment:
These patients were depressed, self-depreciatory and hopeless. Many patients exhibited a rigid, perfectionistic and obsessional personality, although tendencies to minimize and deny difficulty were not conspicuous. They related to the examiner in an apathetic and passive fashion, although a few patients were agitated, fearful and demanding. On inquiry, they complained of anorexia, insomnia, unhappiness, loss of interest in their activities, and inability to cope with their responsibilities, to concentrate, or to make decisions. They had difficulty in staying asleep rather than falling asleep. Somatic complaints other than insomnia, anorexia and constipation would only occasionally be in evidence. However, when present they formed a major preoccupation. Suicidal ideation and frank delusional states were infrequent. These patients did not spontaneously participate in ward activities and if activity was not stimulated and guided they lapsed into apathetic indifference.
With treatment:
There was a marked decrease in expressions of disinterest in the environment, apathy, depression, suicidal rumination, retardation, agitation, insomnia and anorexia. Participation in hospital activities and social relationships increased. Complaints of tension and apprehension relating to difficulties in discharge planning and returning to the community remained, however, with anxious procrastinating attempts to evolve a foolproof plan. Symptoms frequently increased prior to discharge.
Mood elevation was a response frequently associated with favorable medication management and hospital discharge evaluation. Special relationships to age, sex or diagnosis were not evident.
2. EXPLICIT VERBAL DENIAL RESPONSE
Before treatment:
These patients closely resembled those described under mood elevation, although there was more denial and minimization of their difficulties which were usually referred to external events or bodily states rather than emotional distress.
With treatment:
As with mood elevation, depressive symptoms decreased and goal-directed action increased. In contrast to mood elevation, all complaints and difficulties were denied, the patients stating that they were entirely well and should be discharged forth-with, disregarding realistic familial and economic difficulties.
The explicit verbal denial response was generally associated with favorable medication management, an older age group, and a diagnosis of affective disorder. This group received the most favorable hospital discharge evaluations, probably as a consequence of their gross denial of residual difficulties.
Comment:
These patients possessed many of the premorbid personality attributes described by Kahn and Fink (5) as characteristic of patients who responded well to convulsive therapy. Specifically, they were minimizing, denying of difficulty, non-empathic, non-introspective, communicating non-verbally, highly conventional and stereotyped.
3. MANIC RESPONSE
Before treatment:
These patients resembled closely the patients described under mood elevation response.
With treatment:
They first exhibited explicit verbal denial, but then became vociferous with a great display made of their logic as opposed to others illogic. There were periods of psychomotor acceleration accompanied by flights of ideas, loss of frustration tolerance, and lack of self-criticism. In psychotherapy, aggressive verbal attacks upon significant life figures, most frequently spouses and mothers, became common with much talk of divorce or moving away from home. Long standing resentments, previously dealt with by submissive denial, became the focus of therapy with prominent attempts to gain the therapist as an ally against relatives. If this alliance was denied, the patient became hostile and accusatory towards the therapist. Their demanding hostility frequently led them into dictatorial, manipulative, and derogatory attitudes towards both staff and patients. They energetically participated in numerous hospital activities with great self-confidence, occasionally becoming the nucleus for a clique of hostile and negativistic patients. Delusions and bizarre activity did not occur.
Cessation of imipramine medication did not result in a reversion to their previous state, and interruption of this response by large doses of phenothiazine was usually necessary, and helpful.
Manic response was associated with a moderately unfavorable medication management. No special relationships to age, sex, or diagnosis were observed, although the 4 cases of affective disorder showing this response were diagnosed as manic-depressive disorder. There were, however, 15 other subjects with the same diagnosis who did not show a manic response to imipramine.
These patients' medication management classification as unfavorable was determined by their imipramine being replaced by phenothiazines; however, their subsequent improvement resulted in an average discharge evaluation.
4. REDUCTION OF EPISODIC ANXIETY RESPONSE
Before treatment:
Typically, subjects noted the sudden onset of inexplicable “panic” attacks, accompanied by rapid breathing, palpitations, weakness, and a feeling of impending death. Their activities became progressively constricted, until they were no longer able to travel alone for fear of being suddenly rendered helpless while isolated from help. Depressive complaints were infrequent and associated with feelings of futility. Although fear of open spaces was not the hallmark of this condition but rather expectant fear of lack of support when overwhelmed, their condition was often referred to as agoraphobia. They engaged in prolonged outpatient psychotherapy, usually devoted to the exploration of unconscious sexual and aggressive impulses, with the interpretation of the phobically barred areas as situations of forbidden symbolic temptation. Hospitalization occurred after the family could no longer tolerate the restrictions placed upon them.
With treatment:
Under imipramine treatment the “panic” attacks ceased, although both phenothiazines and sedatives had been previously ineffective. However, the patients were reluctant to change their phobic behavior pattern and required much persuasion, direction and support. Their social interaction increased markedly with a surprising rise in aggressive self-assertion and rejection of domination.
The reduction of episodic anxiety response was usually associated with a favorable medication management. This was the only group with a large proportion of psychoneurosis and personality disorder diagnoses. There was no special relationship to age or sex.
Comment:
The reaction to imipramine is of considerable interest since the “anxiety” of the panic attack is sharply diminished while expectant “anxiety” related to the “phobic” patterns remains. The use of the common term “anxiety” may thus obscure an underlying difference in these processes.
Bowlby (3) has emphasized that separation anxiety does not have to be learned via noxious experiences of separation. In this view, separation anxiety has the biological function of evoking the retrieving and mothering response in a parent and is an innate mechanism of social control. One may speculate that imipramine, in these patients, has some specific reparative effects upon this disordered mechanism.
5. AGITATED DISORGANIZATION RESPONSE
Before treatment:
These patients were withdrawn, preoccupied, defensive, suspicious, minimizing and denying. After specific questioning they admitted to ego-alien thoughts but conveyed the impression that their hospitalization was a mistake. Their affect was flat, frequently inappropriate, and apathetic, they appeared to consciously suppress delusional material.
A history of poor social, education and vocational attainment was uniformly present, with many indications of childhood disorder.
They spoke little and by confining themselves to stereotyped utterances preserved a façade of being rational and relevant. However, any extended speech revealed peculiar and bizarre language patterns with neologisms and autistic word usage. Formal thought disorder was evident, with over-concreteness, over-abstraction and loose associations. Psychotherapy was a barren experience as the patients made no effort to relate to their therapists and avoided any discussion of their feelings.
Social contact was actively rejected, the patients remaining isolated on the wards or roaming aimlessly about the grounds. At times they were prankish, eccentric and unpredictable and at best cooperated passively with ward routines and activities.
With treatment:
They first developed an inappropriate euphoria, which was often misinterpreted as the onset of improvement. This was soon followed by bizarre, disorganized, aggressive hyperactivity associated with intolerable tension, fragmentation of thought and marked somatic and paranoid delusions. This response uniformly required the interruption of imipramine treatment and the immediate use of convulsive or phenothiazine therapy.
Agitated disorganization was associated with a negative medication management evaluation and occurred mostly in young, schizophrenic males. This behavioral reaction was a grave prognostic sign as 58% of these patients were discharged “unimproved” and none considered “much improved” or “recovered,” despite subsequent treatment.
Comment:
Of interest is the marked similarity of this group of patients to those described as having the reaction pattern of autistic compliance to phenothiazines (6). The predominance of males is similar to the sex ratio of childhood schizophrenia.
6. ANHEDONIC SOCIALIZATION
Before treatment:
These patients related to the examiner in a discouraged and dependent fashion with manipulative tendencies. They spontaneously grumbled of an anxious depression, also the observed affective display was less than the extensiveness of their complaints. These complaints concerned fluctuating feelings of withdrawal, anxiety, tension, depression, depersonalization, phobic compulsions, ruminative thoughts, and inertia. A lack of feelings of pleasure and competence was prominent.
They were rational, relevant and coherent, and described their complaints in abstract psychiatric terms. It was difficult to obtain a specific connected story concerning their symptomatology. If the psychotherapist indicated certain strengths, this was immediately met by a burst of self-derogatory expressions. Many of these patients had previously received prolonged outpatient psychotherapy.
They associated with similar patients in tight cliques, preserving a friendly relationship. While few of the hospital activities were interesting to them they stayed active rather than withdrawn. They frequently had a history of good social and educational achievement marred by a pervasive anhedonia.
With treatment:
This group manifested an increase in alertness, definiteness and precision. Dependent demands were diminished. Their verbal affective complaints were modified only slightly, although they appeared to be less anxious and depressed. Symptoms of apathy and inability to function were alleviated, while feelings of depersonalization, phobic compulsive and ruminative thoughts were maintained. The effects of the medication were minimized by the patients, yet their symptoms exacerbated on medication withdrawal.
In psychotherapy a degree of overt selfassertion became apparent, associated with some guilt and apprehension over aggressiveness. They became more active, dressed more attractively and associated with more people, achieving responsible positions in their ward or peer group organizations. Hospital activities were utilized more fully and in a more interested fashion.
This response was associated with a favorable management evaluation. This group consisted of young schizophrenic patients without relationship to sex distribution or hospital outcome. The only suicide in this study occurred in this group.
7. NON-RESPONDING PATIENTS
No significant behavioral changes were observed in 40 patients. In pretreatment characteristics, these subjects were classified into a few subgroups.
A group of 13 patients showed histrionic labile affect, with depressive, fearful, paranoid and agitated displays rapidly alternating with affable friendly periods. Their lability made evaluations of drug effect very difficult, requiring long observation periods before an evaluation could be made. The histrionic manipulative character of these patients gave the impression that their affective displays were goal-oriented and ludic devices for manipulation of the environment rather than direct expressions of internal distress. Phenothiazine medications were also ineffective in modifying their behavior.
Other patients had a variety of syndromes with the common thread of marked fixity of symptomatology over a period of years prior to hospitalization. These syndromes were somatic preoccupation (10 patients), obsessional rumination (6 patients), fearful paranoid referential states (4 patients), and a variety of schizoid and psychopathic character disorders (7 patients). Phenothiazine medications were also ineffective in modifying their symptoms.
The “non-responders” were preponderantly female without a special relationship to age or diagnosis. Hospital outcome was poor.
Relation of age and diagnosis to medication evaluation.
By grouping the subjects according to medication management, age and diagnosis, we observed that the percentage of favorable medication management is approximately 51% for schizophrenia, and 79% for affective disorder, at all age levels. We would conclude that diagnosis is more closely related than age to clinical evaluations of imipramine therapy.
CONCLUSIONS
Imipramine appears to be a safe and valuable medication in the treatment of a variety of psychiatric conditions. It produces various behavioral change patterns that are related to both the personality of the patient and the symptom pattern of the illness. While these response patterns cut across the usual nosologic categories, there is a significant statistical relationship to the distinction between schizophrenic and affective disorders. These patterns of behavioral response are highly associated with pretreatment behavioral patterns, and further study may serve to define subgroups whose response to imipramine can be predicted with high probability.
Similar observations are reported by Ayd (1) in a review of the current status of the “major antidepressants.” Allowing for differences in terminology, his findings closely parallel our own. For example, Ayd notes: Dramatic therapeutic results were seen in those patients often diagnosed anxiety hysteria because their depression was overshadowed by severe anxiety with hysterical features. [They] … had good pre-illness personalities despite an anxious, phobic temperament. In contrast to the classical endogenous depressive, these patients had a normal sleep pattern or insomnia, which readily responded to barbiturate hypnotics, rather than an early morning awakening. Usually they complained of feeling worse as the day wore on. They had little appetite disturbance and no great weight loss. They had many somatic complaints. Seldom were they self-depreciatory. They detested being alone, were voluble, anxious, and tremulous and exhibited psychomotor stimulation instead of inhibition … Tranquilizers invariably made them feel worse, ECT enhanced their anxiety… When treated with an antidepressant they reacted promptly…
The personality organization and behavioral response of these patients are strikingly similar to those described as showing a reduction of episodic anxiety response to imipramine.
This response was seen by Ayd as indicating that in these patients “depression was overshadowed by severe anxiety.” In similar fashion, others have referred to “underlying” or “masked” depressions. The basis for these formulations appears to be the positive behavioral response to “antidepressants,” as the classical signs and symptoms of depression are not clinically manifest. Yet, these patients are refractory to convulsive therapy, which should lead to the inference that they do not have an “underlying” depression.
Such terms represent ad hoc formulations that obscure common characteristics distinctive in these patients. In an earlier study (6) we indicated that the behavioral patterns after phenothiazine medication are related to the antecedent behavior, as seen in characteristic adaptive mechanisms, communication patterns, affect, symptoms, psychotherapy participation and social activity. The responses to medication may be used as dissecting tools to uncover various subpopulations and to permit the discovery of specific developmental, physiological, psychological and social similarities within each subpopulation. These common characteristics may also clarify questions of etiology and pathogenesis of psychiatric disorders, and provide rational indications and contraindications for drug therapy. The observations with imipramine reported here suggest that these generalizations may be true for a wide variety of psychotropic agents.
SUMMARY
| 1. | One hundred and eighty voluntary inpatients (102 schizophrenic subjects, 67 subjects with affective disorders, and 11 “other” diagnoses) were studied during treatment with imipramine. | ||||
| 2. | Seven imipramine induced behavioral reaction patterns and their relationships to diagnosis, age, sex, patterns of medication use, and hospital discharge evaluation are presented. These include mood elevation, explicit verbal denial, manic, reduction of episodic anxiety, agitated disorganization, anhedonic socialization, and non-response. | ||||
| 3. | Imipramine was favorably evaluated in 79% of subjects with affective disorders and 51% of schizophrenic patients. | ||||
| 4. | The use of psychiatric reaction patterns to psychotropic drugs for categorizing patients and providing a basis for a more rational pharmacotherapy are emphasized. | ||||
1 Ayd, FJ, Jr.: APA Psychiatric Research Reports, Detroit, 213, 1959.Google Scholar
2 Blumberg, AG, and Klein, DF: Am J. Psychiat., 118: 168, 1961.Crossref, Google Scholar
3 Bowlby, J.: Int. J. Psychoanal., 51: 89, 1960.Google Scholar
4 Fink, M., and Kahn, RL: A.M.A. Arch. Gen. Psychiat., 5: 30, 1961.Crossref, Google Scholar
5 Kahn, RL, and Fink, M.: J. Neuropsychiat., 1: 1, 1959.Google Scholar
6 Klein, DF, and Fink, M.: A.M.A. Arch. Gen. Psychiat. In Press.Google Scholar
7 Kramer, JC, Klein, DF, and Fink, M.: Am. J. Psychiat., 118: 549, 1961.Crossref, Google Scholar