Involuntary Hospitalization of Medical Patients Who Lack Decisional Capacity: An Unresolved Issue
Abstract
(Reprinted with permission from Psychosomatics 2006; 47(5):443–448)
Psychosomatic-medicine psychiatrists often see patients on medical wards who lack the capacity to make treatment decisions when their refusal of necessary treatment may put their health at risk. (1) Although civil commitment because of mental illness and/or being dangerous has been a statutorily regulated and well-studied practice in general psychiatry, (2) there is currently a dearth of information about the issue of involuntary hospitalization for medical patients seen in consultation-liaison psychiatry whose medical disorders may either transiently or more chronically affect their mental status, leading to psychosis, confusional states, and impaired judgment.
Consultation-liaison psychiatrists often struggle with problems presented by patients who lack decisional capacity secondary to a medical illness, are not verbally threatening to self or others, and want to leave the hospital against medical advice (3). Such patients at times have personality changes secondary to a general medical condition or delirium secondary to a general medical condition, (4) but in particular jurisdictions may not meet the criteria or be appropriate for commitment to a psychiatric facility. Consultation-liaison psychiatrists are often consulted on such cases where the patient repeatedly attempts to leave against medical advice and may be combative and require restraints (3). This was precisely the dilemma captured in the following case of “Ms. S.” In this report, specific information about the case has been modified in order to deidentify the details of the case, yet the clinical factors remain illustrative of the difficulties that consultation-liaison psychiatrists often encounter.
CASE REPORT
Ms. S was a 46-year-old woman with multiple medical problems, including HIV/AIDS, HIV dementia, non-insulin-dependent diabetes, history of basilar tip aneurysm, status post-coiling of aneurysm, and an extensive past psychiatric history including bipolar disorder, polysubstance dependence, and multiple psychiatric hospitalizations. She presented to the emergency department with a severe headache and was admitted to the neurosurgery service for assessment and evaluation. During the hospital course, she underwent neurosurgical evaluation and work-up that revealed a questionable new hemorrhagic lesion. On Hospital Day 2, the Psychiatry Consult service was called to evaluate symptoms of paranoia. The impression of the consult team was that she had cognitive disorder, not otherwise specified, or HIV-related dementia. The psychiatric team continued to follow the patient, who subsequently developed a fever and became increasingly confused. Upon further assessment, the consult team believed that she did not have decisional capacity related to her medical treatment. The clinical opinion was based on the observations by the psychiatrists that Ms. S lacked decision-making capacity related to her inability to appreciate her clinical situation and its consequences and her inability to manipulate information presented about her treatment. Specifically, she stated that discontinuing her HIV medications or leaving the hospital against medical advice would not put her health at risk. She was unable to rationally discuss the information about her treatment as she vehemently discussed the futility of treatment even when presented with information about its potential benefits. The consult team's impression was that the lack of capacity was related to a diagnosis of delirium. The cause of delirium was thought to be infectious, yet the exact infectious etiology was not known at that time. The consult team suggested that the medical team pursue guardianship. Pharmacological management of the delirium was also recommended and prescribed at that time.
On Hospital Day 5, before a guardian was instituted, the Psychiatry Consult service was called again because the patient was agitated, combative, and attempting to leave the hospital against medical advice. Consistent with the previous assessment, the on-call psychiatric consultant determined that she lacked capacity to make medical decisions and fit the diagnosis of delirium secondary to a general medical condition, in the context of an underlying HIV dementia. Her delirium work-up was ongoing, and the etiology of her delirium was still not known. Because Ms. S refused to cooperate with a formal cognitive examination, the diagnosis of delirium was based on her waxing and waning mental status, disorientation, memory impairment, and clouding of consciousness. She alternated between extremes of agitation and somnolence. She repeatedly fell asleep while speaking. Furthermore, her presentation differed markedly from her previous psychiatric presentations, providing additional support for the diagnosis of delirium.
The patient was considered dangerous to herself secondary to her lack of decision-making capacity in light of her progressively worsening medical condition. Through-out, she had been hospitalized on a voluntary basis. Her request to leave led to much confusion among hospital staff, given her status as a voluntarily hospitalized patient. The impression of the psychiatrist on call was that Ms. S did not meet criteria for psychiatric commitment, nor was it clinically indicated. Under Massachusetts General Laws, application for an involuntary admission to an inpatient psychiatric facility is specified with the following limitations: “Symptoms caused solely by alcohol or drug intake, organic brain damage, or mental retardation do not constitute a serious mental illness” (6). The clinical consult team felt that, in light of the language of the statute, Ms. S's diagnosis of delirium secondary to a general medical condition qualified as “organic brain damage” and therefore precluded her from meeting criteria for civil commitment under the jurisdiction at issue. Even if she had met clinical criteria for pursuing involuntary commitment, Ms. S had acute medical issues that made transfer to a psychiatric unit not an appropriate option at the time. The psychiatrist on call recommended that Ms. S should not be allowed to leave against medical advice and that the medical team should use restraints to keep her in the hospital if less restrictive methods failed.
The treating physicians were not able to redirect Ms. S, and she remained combative and continued to demand to leave against medical advice. At that time, it was decided that Ms. S needed to be restrained in order to maintain her safety. The campus police refused to restrain the patient, stating that she could not be restrained or kept in the hospital against her will without psychiatric legal commitment documents. The psychiatrist on call discussed this refusal with the hospital police sergeant, who also reported that the patient could not be restrained or kept in the hospital against her will without psychiatric legal commitment documents. The medical team and psychiatrist on call had reached an impasse with the police. The patient needed to be restrained to maintain her safety; the police adamantly refused to restrain her without commitment documents; and the patient did not appear to the clinical team to meet commitment criteria.
The medical team, the psychiatrist on call, and the police debated this point while Ms. S became increasingly agitated. While the medical team was trying to come to an agreement as to how to manage Ms. S, she voiced suicidal ideation. In view of her recently reported suicidal thoughts, psychiatric commitment documents were completed and placed in the chart. The rationale for completing commitment documents at that time was based on her newly-stated suicidal thoughts. According to the consulting psychiatric team, she now fit commitment criteria based on “substantial risk of harm to self as manifested by threats of or attempts at suicidality” (6). Although the consulting psychiatrist was aware that her suicidality may have been part of her delirium presentation, the patient was clearly at risk. Completing commitment papers seemed the only way to maintain the patient's safety, and the consulting psychiatrist did what was necessary. Attributing her suicidality to affective symptoms in the context of a patient with an underlying mood disorder appeared to the consulting team to be an appropriate clinical rationale used to complete the application for her commitment. This also allowed additional time to assess the patient's evolving presentation and the need to proceed to a judicial commitment hearing. Once commitment documents were completed, the police restrained the patient, and she was able to be kept on the medical floor.
This case was particularly frustrating to those involved because the treating physicians and hospital campus police had differing opinions about how this patient should be managed. Eventually, psychiatric commitment documents were completed; yet neither the treating physicians nor the police were certain whether this was the appropriate step. There was a lack of understanding among all involved as to how Ms. S should be kept in the hospital, both legally and ethically. Ms. S's delirium resolved after several weeks, yet she did not regain decisional capacity, and it was determined that she had an underlying severe HIV dementia that continued to impair her decisional capacity. Guardianship was pursued and obtained before her discharge to the community. The hospital attorney was alerted to the case and the confusion that had ensued related to the requirements for involuntarily holding a patient on a medical floor. Training seminars for campus police and a consultation-liaison seminar presentation were subsequently initiated in order maximize multidisciplinary understanding of “restraints” laws and policies.
DISCUSSION
This case provides an objective lesson for consultationliaison psychiatry in both the difficulty of dealing with patients who lack decisional capacity and the conundrums and legal issues involved in the issue of continuing to hospitalize patients involuntarily. This situation brought up the following questions: 1) How do we continue to hospitalize involuntary patients who lack capacity to make medical decisions secondary to a general medical condition, are threatening to leave against medical advice, and yet do not have specific evidence of mental illness and risk of harm to themselves or others that would meet criteria for civil commitment? 2) What is legally/ethically appropriate? 3) How does the medical staff hold the patient on the medical floor? 4) What is the role of the police? Our objective in this Case Report is to examine the legal issues encountered and help clarify how physicians could hospitalize involuntary patients within the context of consultation-liaison psychiatry to provide guidance for medical and psychiatric staff in such complex situations.
COMMITMENT CRITERIA VERSUS DECISIONAL CAPACITY
The chaos in the case of Ms. S might have been avoided if the distinction between meeting commitment criteria and lacking decisional capacity had been clear. Part of the difficulty was that she presented with a history of mental illness and new-onset medical problems. Nevertheless, improved understanding of the concepts of commitment and decision-making capacity may help decrease the confusion among police and hospital staff that our case illustrates. Involuntarily hospitalizing patients in the context of consultation-liaison psychiatry differs from committing patients to a psychiatric facility. Civil commitment refers to the involuntary hospitalization of people with mental illness. The power to commit represents a significant limitation on the individual; therefore, it should be used only with extreme care (7). Most jurisdictions provide short-term psychiatric hospitalizations for patients with mental illness in emergency situations until a court hearing can be held. The period that a person can be held involuntarily varies across jurisdictions. The criteria that must be met to continue to hold a psychiatric patient are often those required for court-ordered commitment. At the end of periods of emergency commitment, facilities must decide whether to release the patient or to petition for court-ordered hospitalization. The strict time-limits on the duration of an emergency commitment are sometimes subverted secondary to delays at the court level in scheduling hearings. As a result, patients may be involuntarily detained for psychiatric reasons for weeks or months before a hearing (7).
The standards that the patient, as a result of being mentally ill, must meet to be committable generally include some combination of several of the following criteria: the patient is 1) a danger to others; 2) a danger to self; 3) unable to care for self; 4) a danger to property; 5) in need of psychiatric treatment; and 6) at risk of deterioration (5). The state's general power to use civil commitment is described as limited to individuals who have a mental disorder, often itself defined by state regulations, statutes, or case law. The debate about the scope of civil commitment is, at times, posed as a problem of defining the kind of mental disorder that is required to justify commitment (2).
Involuntarily hospitalizing medical patients in the context of consultation-liaison psychiatry also differs from determining competency. Competency refers to some minimal mental, cognitive, or behavioral ability, trait, or capability to perform a particular jural act, or to assume a legal role (8). All persons are presumed competent, and, unless their competence is questioned, patients are afforded autonomy in their decisions to accept or reject recommended medical treatment. The term “capacity” is often interchanged with competency; however, the two are not synonymous. Although physicians regularly make determinations about their patients' decision-making capacity, only a judge can declare a patient legally incompetent. Capacity evaluations in consultation-liaison psychiatry generally refer to an assessment of an individual's ability to express a choice around a particular decision, understand information presented to them about their choices, reason through decisions without the influence of mental illness, and appreciate the nature of their situation (9). Agreement or disagreement on the part of the physicians or care-providers with a patient's decision is not at issue; the capacity assessment is meant to look at the decision-making process, rather than the ultimate decision (8).
From a legal perspective, task-specific competencies may be narrowly defined by statute or case law in a given jurisdiction. For example, competency to stand trial is not the same as competency to make treatment decisions. Decision-making capacity involves the ability to appreciate the reasonably foreseeable consequences of a decision or lack of decision. Capacity is specific to particular decisions, and it can change over time. Courts will generally weigh the clinical capacity data to help inform judicial determinations regarding competence, although firmly established national legal standards for determining a patient's competency to make treatment decisions do not exist. A person may be temporarily decisionally-impaired secondary to delirium and may subsequently recover his or her capacity. When patients who lack capacity to make their own medical decisions reject recommended treatment, clinicians are faced with the need to determine the appropriate course of action, the expectation of recovery, and the existence of some type of advance-directive for healthcare decisions may come into play (9).
In establishing what is legally and ethically appropriate when advance-directives are not available, it is important to consider that a patient who lacks capacity to make medical decisions is not necessarily committable. Likewise, patients who appear to meet criteria for civil commitment because they present a substantial risk of harm to themselves or others may not lack the capacity to make medical decisions. It has been established that the lack of decisional capacity is not equivalent to the need to be committed to a psychiatric facility (7). When working within psychosomatic-medicine services, one is often faced with a patient who does not appear to have a significant mental illness, and is therefore not appropriate for civil commitment to a psychiatric ward, but who lacks the capacity to make medical decisions because of an underlying medical condition and expresses a desire to leave the hospital. In these situations, it is not always clear what steps should take place before such a patient may be forced to stay in the hospital on an involuntary basis. The following framework for consideration and subsequent discussion (represented as an algorithm in Figure 1) offers some areas for consideration in these situations.
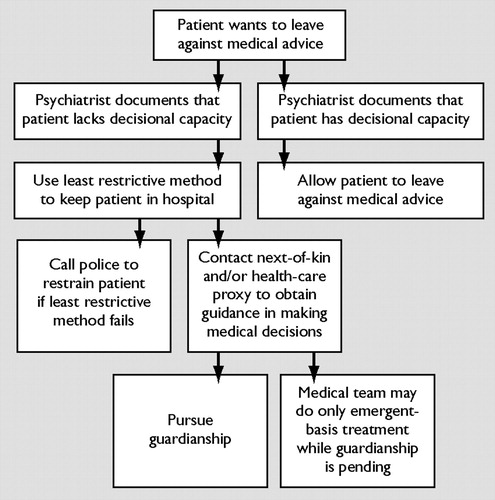
Figure 1. Algorithm for Approaches to Treating Patients Wanting to Leave Against Medical Advice
PROPOSED APPROACHES TO HOSPITALIZATION OF MEDICAL PATIENTS REQUESTING TO LEAVE AGAINST MEDICAL ADVICE
If a patient is believed to lack decisional capacity and wants to leave against medical advice, the medical team must take necessary steps to keep the patient in the hospital (3). If, however, the patient who wants to leave the hospital is believed to have adequate decisional capacity, he or she must be allowed to leave against medical advice. Patients who have decisional capacity are not forced to accept treatment, even when the decision results in a hastening of death (14). Physicians have a responsibility to protect patients who may lack the capacity to protect themselves or care for themselves. In exercising this obligation, such patients may be held in the hospital in order to protect them.
Depending on the jurisdictional parameters, documents to initiate psychiatric civil commitment may not be appropriate to keep a patient who does not fit criteria for inpatient psychiatric admission on a medical floor. When a patient requests to leave the hospital against medical advice, medical teams should contact appropriate consultants as needed to help ascertain a patient's decision-making capacity and appropriateness for commitment. Documentation of the assessment should include a medical history and mental status exam, capacity evaluation, and assessment of decisional capacity from the inpatient's medical chart, in cluding whether it is a primary psychiatric issue or a psychiatric issue secondary to a general medical condition. The involvement of next-of-kin, as available, in these situations is a potential option, in order to obtain guidance in making medical decisions and in keeping a patient who lacks decisional capacity on a medical floor for safety (10). Unless a “healthcare proxy” is in place so indicating, the next-of-kin cannot legally override a patient's refusal to stay in the hospital, but can provide guidance with treatment decisions while guardianship is pending. In these situations, it is important to provide the family with only the information needed to manage the medical situation, balancing confidentiality and attempts at obtaining guidance in the particular situation (7).
Previous authors have commented on the ability of the medical team to hold a patient involuntarily on a medical floor but not to treat the patient against his or her will except in acute emergency situations where immediate lifepreserving care is necessary (3). Medical teams should use the least restrictive methods to hold the patient on the medical floor. If medical staff's attempts to manage the patient without physical or mechanical restraints fail, they may call police to restrain the patient in order to maintain order. Specific federal statutes and national guidelines address the use of mechanical restraints in medical and behavioral health situations, (11–13) and clinicians may wish to gain familiarity with them. In situations where the need for mechanical restraints arises, the initiation of legal or administrative review, as appropriate for the jurisdiction, can help attend to the legal rights of patients, which can also serve to address ethical concerns related to possible inappropriate coercive treatment of patients. Input from hospital legal and/or administrative personnel can be critical when clinical management intersects with a patient's autonomy in decision-making. Hospital ethics teams can also be helpful in sorting through issues related to coercion in treatment. Official guidelines are less clear for situations where the lack of capacity is suspected to be short-lived but not immediately resolved (3). However, the treatment team may wish to consider pursuit of guardianship if lack of capacity is suspected to persist. While guardianship is pending, the medical team may engage in emergency-based treatment (3).
Restraints may be necessary in order to protect patients from their own behavior when they experience delirium. There are many situations where patients can, and do, injure themselves if they are not restrained. First, however, we should attempt to mitigate the reason for the patient's agitation (e.g., by pain control) (11). Clinicians would do well to follow their hospital's policies and protocols, as well as local regulations regarding the use of restraints and the interface with police to aid in the restraint process when needed. Restraints should be used only when it has been deemed a clinical necessity and when less restrictive alternative measures have been unsuccessful or cannot be used without jeopardizing safety or care (14).
The hospital legal counsel can be helpful in resolving areas of disagreement between clinical and security staff related to interpretation of the parameters for restraint. Hospital administration or counsel may consider educating police or security as well as clinical staff in order to maximize the potential for a common understanding of restraint policies and procedures. Promoting ongoing communication among nurse-managers may help avoid confusion and disagreement over the appropriate placement of the patient within the hospital in such situations.
Consultation-liaison psychiatrists often struggle with problems presented by patients who lack decisional capacity secondary to a medical illness, who want to leave the hospital against medical advice, and are considered dangerous to themselves secondary to their lack of decision-making capacity. Consultation-liaison psychiatrists are often consulted in such cases where the patient attempts to leave against medical advice and may be combative and require restraints. There is currently a lack of information on the issue of involuntary hospitalization in consultation-liaison psychiatry. Proper and continuous training about management of patients lacking decisional capacity should be provided to staff. Support should also be provided to medical teams, who may have numerous demands that compete with the time needed to petition for guardianship and pursue the results. We have presented the case described herein and proposed approaches to help increase the awareness of the complexity of issues at play in patients who may present on medical floors requesting to leave the hospital.
1 O'Hara D, Hart W, McDonald, I: Leaving hospital against medical advice. J Qual Clin Pract 1996; 16: 157– 164Google Scholar
2 Janus E: Toward a conceptual framework for assessing police power commitment legislation: a critique of Schopp's and Winick's explications of legal mental illness. 76 Neb Law Rev 1, 1997Google Scholar
3 Wise, T, Berlin, R: Involuntary hospitalization: an issue for the consultation-liaison psychiatrist. Gen Hosp Psychiatry 1987; 9: 40– 44Crossref, Google Scholar
4 American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision. Washington, DC, American Psychiatric Association. 2000, p 401Google Scholar
5 Appelbaum, PS, Grisso, T: Assessing patients' capacities to consent to treatment. N Engl J Med 1988; 319: 1635– 1638Crossref, Google Scholar
6 Massachusetts General Laws: chap. 123, Section 12AGoogle Scholar
7 Gutheil T, Appelbaum P: Clinical Handbook of Psychiatry and the Law. Philadelphia, PA, Lippincott Williams & Wilkins, 2000, pp 51– 52, 231, 234Google Scholar
8 Rajput, V, Bekes, C: Ethical issues in hospital medicine. Med Clin North Am 2002; 86: 869– 886Crossref, Google Scholar
9 Lo, B: Advance care planning. Am J Geriatr Cardiol 2004; 13: 316– 320Crossref, Google Scholar
10 American Psychiatric Association: Document Reference number 960001. Principles of Informed Consent in Psychiatry (www.psych.org/edu/other_res/lib_archives/archives/199601.pdf)Google Scholar
11 Hash M: Department of Health and Human Services: Health Care Financing Administration: Testimony on Patient Treatment in Mental Hospitals. (http://www.hhs.gov/asl/testify/t991026a.html), accessed 6/16/05Google Scholar
12 Joint Commission on Accreditation of Healthcare Organizations: Restraint and seclusion standards for behavioral health. (http://www.jcaho.org/accredited+organizations/behavioral+health+care/standards/faqs/provision+of+care/special+interventions/), accessed: 6/16/05Google Scholar
13 Pinals, D, Appelbaum, P: Impact of the evolving legal framework for chemical restraints. Directions in Psychiatry 2003; 23: 317– 332Google Scholar
14 Maccioli, GA, Dorman, T, Brown, BR, et al: Clinical Practice Guidelines for the Maintenance of Patient Physical Safety in the Intensive Care Unit: Use of Restraining Therapies. American College of Critical Care Medicine Task Force, 2001–2002. Crit Care Med 2003; 11: 2665– 2676Crossref, Google Scholar



