Assessment of Decision-Making Capacity in Older Adults: An Emerging Area of Practice and Research
Abstract
The convergence of the aging of our society, the increase in blended families, and an enormous intergenerational transfer of wealth has greatly expanded the incidence and importance of capacity assessment of older adults. In this article we discuss the emergence of capacity assessment as a distinct field of study. We review research efforts in two domains: medical decision-making capacity and financial capacity. Existing research in these two areas provides a first pass at many key questions related to capacity assessment, but additional studies that replicate, extend, and improve on this research are urgently needed. An agenda for future is detailed that recommends studies of a wide range of capacity constructs, focusing on clinical markers of diminished capacity, methods to improve clinical assessment, and the many intersections of law and clinical practice.
(Reprint w/permission from Journal of Gerontology: PSYCHOLOGICAL SCIENCES 2007, Vol. 62B, No. 1, P3– P11)
The field of capacity assessment is dominated by a fundamental tension between two core ethical principles: autonomy (self-determination) and protection (beneficence; Berg, Appelbaum, Lidz, & Parker, 2001). What should we do when an older adult, particularly one who is frail, vulnerable, dementing, or eccentric, begins to make decisions that put the elder or others in danger, or that are inconsistent with the person's long-held values? At what point does decision making that is affected by a neuropsychiatric disease process no longer represent “competent” decision making? These are some of the essential, and perplexing, questions of clinical capacity assessment.
We use the term capacity to refer to a dichotomous (yes or no) judgment by a clinician or other professional as to whether an individual can perform a specific task (such as driving or living independently) or make a specific decision (such as consenting to health care or changing a will). There are at least eight major capacity domains of relevance to older adults with neuropsychiatric illness, as presented in Table 1. Two of these require a broad set of cognitive and procedural skills—independent living and general financial management. Other capacities, such as treatment consent, testamentary capacity (wills), research consent, sexual consent, and voting, are generally narrower in scope, focusing on one or a small number of specific decisions requiring an underlying set of cognitive abilities. These narrow capacities, although technically legal capacities, are rarely subject to judicial review.
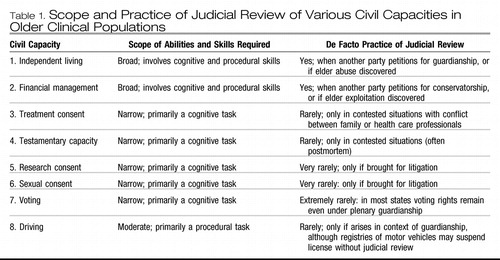 |
Table 1. Scope and Practice of Judicial Review of Various Civil Capacities in Older Clinical Populations
Decisions about capacity are ultimately legal judgments enforced by the power of the state. However, in practice, the majority of determinations of diminished capacity are probably made outside of the courtroom, by clinicians, attorneys, adult protective service workers, and other professional groups working with the elderly population. As noted in Table 1, situations requiring guardianship or conservatorship are resolved in a court of law, and they require a legal determination regarding competency. However, in such cases where there exists a previously appointed surrogate (such as a health care proxy), the authority of the surrogate springs into effect on the basis of a clinical finding of diminished capacity without judicial review. Further, in practice, many situations of diminished capacity are managed without any formal determination of incapacity or appointment of a surrogate. For example, a caregiver to an adult with dementia may simply assume responsibility for bill paying and investments, or strategically disallow driving. Thus families are often the arbiter of judicial involvement, seeking court authority in situations that cannot be managed through less restrictive alternatives. This somewhat fuzzy line between the family, the clinical role, and judicial role in managing diminished capacities in older adults can create considerable confusion but is important to recognize (Ganzini, Volicer, Nelson, & Derse, 2003).
In this article we consider civil capacity assessment of older adults as a growing field of clinical practice and empirical research. We note the sociodemographic forces that are driving the new prominence of capacity assessment, discuss cross-disciplinary interest in capacity assessment, and describe the emergence of capacity assessment as a distinct field of practice and research. We then review existing research in the two important clinical domains of medical decision-making capacity and financial capacity, and we outline an agenda for future research.
SOCIODEMOGRAPHIC CHANGES AND CAPACITY ASSESSMENT
There are important sociodemographic forces that have made capacity assessment a topic of national concern. Our population is aging at an extraordinary pace, and the prevalence of cognitive aging, dementia, and medical and neurological comorbidities increases dramatically with age. Such cognitive and physical changes are intimately linked with declines in everyday functioning that include loss of decision-making skills (Karlawish & Schmitt, 2000; Kim, Karlawish, & Caine, 2002). The effects of multiple interacting medical conditions on decision-making abilities vary across individuals, affecting some aspects of decision making and not others, calling for sophisticated and functionally oriented capacity assessment.
Attention to capacity issues is also increasing as a result of large-scale financial and cultural changes. Our society is undergoing a massive transfer of wealth from the World War II to the baby boomer generation (Havens & Schervish, 2003) within families that are increasingly blended and living at geographical distance. As a result, probate courts are seeing a marked rise in contested guardianships and wills, and there is a high prevalence of elder abuse and exploitation by strangers, friends, and family members (National Center on Elder Abuse, 2005).
INCREASING INTEREST IN CAPACITY ASSESSMENT ACROSS PROFESSIONAL DISCIPLINES
As a result of these changes, capacity assessment, previously a relatively peripheral aspect of clinical or legal practice, has over the past 20 years become a generic, everyday issue that permeates different sectors of society. Issues of decision-making capacity are germane to a wide range of professional disciplines, including biomedical clinicians, mental health workers, adult protective service workers, police, judges, and attorneys, as well as to cognitively impaired individuals and concerned families. By its very nature, capacity determination itself is a complex, cross-disciplinary endeavor involving knowledge of medical syndromes, clinical assessment, ethics, and the law. Recent collaborations between the American Bar Association and the American Psychological Association represent an attempt to integrate these diverse disciplines into practical applications (American Bar Association Commission on Law and Aging and American Psychological Association, 2005, 2006).
EMERGENCE OF CAPACITY AS A FIELD OF STUDY
Not surprisingly, capacity assessment has recently emerged as a distinct field of legal, clinical, and behavioral research (Marson & Ingram, 1996). The origins of the field lie in a series of important articles published in the late 1970s and early 1980s on the capacity of psychiatric patients to consent to treatment (Appelbaum, 1982; Appelbaum & Bateman, 1980; Appelbaum & Grisso, 1988; Appelbaum & Roth, 1981; Meisel, Roth, & Lidz, 1977; Roth, Meisel, & Lidz, 1977). In the later 1980s and 1990s the field benefited from additional scholarly rigor through seminal theoretical and empirical work by Appelbaum and Grisso (Appelbaum & Grisso, 1988, 1995; Grisso, 1986; Grisso & Appelbaum, 1998a, 1998b) and the pioneering work of others focusing on older adults (Fitten, Lusky, & Hamann, 1990; Kim et al., 2002; Marson, Chatterjee, Ingram, & Harrell, 1996; Marson, Cody, Ingram, & Harrell, 1995; Moye & Karel, 1999; Sabatino, 1996; Smyer, Schaie, & Kapp, 1996; Stanley, Stanley, Guido, & Garvin, 1988; Taub, Baker, Kline, & Sturr, 1987).
DEVELOPMENT OF CAPACITY ASSESSMENT INSTRUMENTS
The development of objective instruments to measure capacity has been integral to the emergence of the capacity assessment field. In the earlier part of the 20th century, incapacity was determined on the basis of the presence of a diagnosis alone, and perhaps some global indication of mental status. A critical conceptual and legal development has been the shift away from diagnosis to the consideration of key functional abilities relevant for specific capacity domains (Grisso, 2003). The emphasis on function has sparked efforts at developing standardized instruments to empirically measure skills in these domains. Among these instruments are those produced by the MacArthur Group to assess capacity to consent to treatment (Grisso & Appelbaum, 1998b) and research (Appelbaum & Grisso, 2001), by Marson and colleagues to assess capacity to consent to treatment (Marson, Ingram, Cody, & Harrell, 1995) and financial decision making (Marson et al., 2000), as well as instruments to assess the capacity to live independently (guardianship; Anderer, 1997; Loeb, 1996). Several recent reviews summarize the properties and uses of various instruments (Moye, 2003; Moye, Gurrera, Karel, Edelstein, & O'Connell, 2006; Sturman, 2005).
Standardized capacity assessment instruments aim to improve upon the notorious low reliability of more general clinical examinations (Markson, Kern, Annas, & Glantz, 1994; Marson, McInturff, Hawkins, Bartolucci, & Harrell, 1997; Rutman & Silberfeld, 1992) by focusing clinical assessment on the most relevant functional skills. They are meant to supplement but not supplant clinical judgment about capacity. Because of the interactive and contextual nature of capacity, a test score alone cannot substitute for a professional clinical judgment (Kapp & Mossman, 1996). A significant challenge in the development of such instruments is that there is no generally accepted criterion validity standard for capacity. Therefore, capacity assessment instruments are validated through construct validation (Moye, 2000) by a consideration of the convergence of various approximate indicators of validity, namely, the finding of incapacity in populations who are expected to have diminished capacity and the consistency of measurement over time and methods—such as the association between two measures of capacity, or the association of a capacity measure and cognitive tests.
EMPIRICAL CAPACITY RESEARCH
The introduction of standardized instruments has been central to the emergence of empirical capacity research. Research to date has focused on five core issues: (a) the nature of capacity impairment within different patient groups; (b) cognitive predictors of capacity performance within different patient groups; (c) the reliability of capacity ratings across clinicians; (d) associations between different methods of capacity assessment (i.e., psychometric vs clinician base approaches), and (e) the longitudinal course of capacity change and decline.
In the remainder of this article we summarize and analyze research in the two important clinical capacity domains that have received the most research attention to date: treatment consent capacity and financial capacity. We offer summaries of research to illustrate the range, strengths, and limitations of existing research, and to serve as a basis for outlining an agenda for future research. For in-depth reviews of research in these areas, readers may refer to other sources (Grisso, 2003; Kim et al., 2002; Marson, 2001; Moye, Gurrera, et al., 2006; Moye, Karel, & Armesto, 2007).
CAPACITY TO CONSENT TO MEDICAL TREATMENT
BACKGROUND
Treatment consent capacity is a fundamental aspect of personal autonomy and refers to a patient's cognitive and emotional capacity to select among treatment alternatives or to refuse treatment (Berg et al., 2001; Grisso, 1986; Tepper & Elwork, 1984). In the United States, consent capacity is the cornerstone of the medical-legal doctrine of informed consent, which requires that a valid consent to treatment be informed, voluntary, and competent (Kapp, 1992; Marson, Ingram, et al., 1995). In Section 1(3), the Uniform Health-Care Decisions Act (National Conference of Commissioners on Uniform State Laws, 1993) defines consent capacity as “the ability to understand significant benefits, risks, and alternatives to proposed health care and to make and communicate a health-care decision.” As a capacity, treatment consent is distinctive for several reasons: (a) it arises in a medical and not a legal setting; (b) it generally involves a physician, psychologist, or other health care professional, and not a legal professional, as decision maker about capacity; and (c) these judgments are rarely subject to judicial review (Grisso, 2003).
CONCEPTUAL MODEL
A conceptual model of consent capacity based on U.S. case law outlines four core abilities. The first is expressing a choice, which is the ability simply to convey a relatively consistent treatment choice. The second is understanding, which is the ability to comprehend diagnostic and treatment-related information, including the risks or benefits of proposed treatments. The third is appreciation, which is the ability to relate diagnostic and treatment information and related consequences to one's own personal situation. The fourth is reasoning, which is the ability to rationally evaluate and compare treatment alternatives (Appelbaum & Grisso, 1988; Drane, 1985; Roth et al., 1977; Tepper & Elwork, 1984).
EMPIRICAL WORK
Treatment consent capacity in older populations is the most extensively researched of any of the civil capacities, although the overall number of studies is still small. In our review of 16 studies (some with multiple publications), patient sample sizes ranged from 20 to 100 individuals (M = 41.44, SD = 22.54), as presented in Table 2.
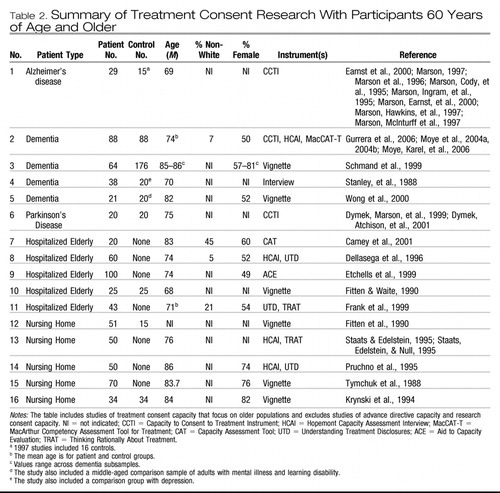 |
Table 2. Summary of Treatment Consent Research With Participants 60 Years of Age and Older
IMPAIRMENT WITHIN PATIENT GROUPS
Older adults who are hospitalized or in nursing homes.
Older adults evaluated in long-term-care settings have high rates, between 44% and 69%, of capacity impairment (Barton, Mallik, Orr, & Janofsky, 1996; Fitten & Waite, 1990; Krynski, Tymchuk, & Ouslander, 1994; Pruchno, Smyer, Rose, Hartman-Stein, & Laribee-Henderson, 1995; Royall, Cordes, & Polk, 1997; Staats & Edelstein, 1995; Tymchuk, Ouslander, & Fitten, 1988). Similarly, acutely hospitalized older patients have demonstrated transient capacity impairments (Carney, Neugroschl, Morrison, Marin, & Siu, 2001; Dellasega, Frank, & Smyer, 1996; Etchells et al., 1999; Fitten & Waite; Frank, Smyer, Grisso, & Applebaum, 1999).
Older adults with dementia.
Compared with healthy control individuals, the consent capacity of individuals with dementia is reduced (Kim, Caine, Currier, Leibovici, & Ryan, 2001; Marson, Cody et al., 1995; Marson, Ingram, et al., 1995; Moye, Karel, Azar, & Gurrera, 2004a; Schmand, Gouwenberg, Smit, & Jonker, 1999; Stanley, 1988; Wong, Clare, Holland, Watson, & Gunn, 2000), particularly for understanding, reasoning, and appreciation (Marson, Cody, et al.; Marson, Ingram et al.; Moye et al.) Using norm-based cutoffs, researchers have found that adults with dementia are most impaired on measures of understanding, followed by reasoning and appreciation (Marson, Ingram, et al.; Moye et al.). Rates of impairment varied, depending on the instrument used. Loss of task (difficulty projecting oneself into the story), nonresponsive answers, and loss of detachment (confusion over the hypothetical nature of the task) are qualitative errors associated with capacity impairment in patients with mild Alzheimer's disease (AD; Marson, Annis, McInturff, Bartolucci, & Harrell, 1999).
Adults with psychiatric illness.
A number of studies have examined consent capacity in patients with psychiatric illness (Grisso & Appelbaum, 1995; Saks et al., 2002; Wong, Cheung, & Chen, 2005; Wong et al., 2000), but these studies have not focused on older populations
RELIABILITY OF CAPACITY ASSESSMENT
Agreement between physicians is near chance for patients with dementia (Marson, McInturff, et al., 1997), with physicians basing their capacity judgments on different cognitive skills of patients (Earnst, et al., 2000) but it improves with training on legal standards (Marson, Earnst, Jamil, Bartolucci, & Harrell, 2000). Agreement is highest for understanding and lowest for appreciation.
VALIDITY OF CONSENT CAPACITY ASSESSMENT
Agreement between multiple capacity assessment methods.
Agreement between instrument-based assessments of capacity and physician-based assessments is poor in some studies (Bean, Nishisato, Rector, & Glancy, 1996; Fitten et al., 1990) and good in others (Carney et al., 2001; Etchells et al., 1999). Agreement between different capacity measures is good for understanding, fair for reasoning and expressing a choice, and poor for appreciation (Moye, Karel, Azar, & Gurrera, 2004b).
Association between capacity measures and cognitive measures.
Understanding is associated with conceptualization and confrontation naming in AD (Marson et al., 1996) and executive functions, memory, and comprehension in adults with Parkinson's dementia (PD; Dymek, Atchison, Harrell, & Marson, 2001). In the same study groups, appreciation is related to verbal fluency, visual attention, and conceptualization in AD (Marson et al.), whereas no specific neuropsychological test was related to appreciation in PD (Dymek et al.). Reasoning is related to verbal fluency in AD (Marson et al.) and to executive functions, mental flexibility, attention, and delayed memory in PD (Dymek et al.). Expressing a choice is related to auditory comprehension and confrontation naming in AD (Marson et al.), and to memory, comprehension, attention, and executive functions in PD (Dymek et al.).
In a factor analytic study, neuropsychological factors robustly predicted understanding, but they had modest to low prediction for reasoning, appreciation, and expressing a choice. A verbal retrieval factor strongly predicted understanding, whereas both verbal retrieval and problem-solving factors were predictive of reasoning and appreciation (Gurrera, Moye, Karel, Azar, & Armesto, 2006). In an earlier factor analytic study, consent capacity as a construct in AD was explained by two neuropsychologically mediated factors associated with verbal conceptualization and verbal memory (Dymek, Marson, & Harrell, 1999).
LONGITUDINAL COURSE OF CAPACITY DECLINE IN DEMENTIA
Consent capacity declines as dementia progresses. Patients with mild dementia show impaired decisional capacity at baseline, and they demonstrate significant additional decline on complex consent abilities of appreciation, reasoning, and understanding over a 2-year period (Huthwaite et al., in press). Loss of capacity over time is attributable to declining reasoning, and it was predicted by earlier problems with naming, verbal memory, and mental flexibility (Moye, Karel, Gurrera, & Azar, 2006).
SUMMARY
Over the past 10 years, the topic of treatment consent capacity in elderly persons has been receiving increasing research attention (Kim et al., 2002), yet the overall number of studies is still small. Within these studies, findings are limited by small samples, little replication of findings, and, in many cases, an absence of control groups.
Together, the studies have found, not especially surprisingly, some general agreement between impairment as measured on standardized capacity measures and neuropsychological measures, although there are too few studies to state with confidence the exact relationships between legal standards for consent capacity and specific underlying cognitive abilities. Understanding is often strongly associated with verbal retrieval, which perhaps raises the question of whether prevailing methods of assessing understanding rely too heavily on verbal recall and miss the opportunity to provide cues and supports to maximize comprehension and minimize memory demands (Dunn & Jeste, 2001). Of more concern is that those studies focusing on reliability between capacity assessment methods tend to find limited agreement between evaluations by multiple clinicians, multiple measures, or between a clinician and a measure, especially for the standards of appreciation and reasoning. This suggests that more work may be needed to further flesh out these constructs and to improve the reliability and validity of their measurement.
These studies also find that patients with dementia are impaired on consent abilities, and that as the dementia progresses, so too do the consent impairments. Of note, there appear to be no studies of older patients with chronic mental illness, whose already fragile decisional abilities may deteriorate further in late life. Measurement strategies developed to assess abilities in one patient group may work less well in other patient groups. For example, memory impairment may be a primary factor in diminished capacity for patients with dementia, whereas executive dysfunction and psychiatric symptomatology may figure more significantly for patients with schizophrenia, and therefore this impacts how diminished capacity should be assessed and also how capacity might be maximized.
It is concerning that so few studies report the racial and ethnic makeup of the individuals in their samples, and to date there is no exploration of how and whether racial and cultural factors and other important values intersect with the assessment of consent capacity, despite the fact that medical decision making, in itself, varies by these factors (Caralis, Davis, Wright, & Marcial, 1993; Eleazer et al., 1996; Karel, 2000). Could an incongruence between patient and clinician values about treatment decision making (see, e.g., Jahng, Martin, Golin, & DiMatteo, 2005) impact the outcome of capacity assessments? Such questions await study. As a general rule, although the ability to select treatment choices in view of one's values is a core indicator of capacity (Berg et al., 2001), the relationship values and capacity assessment is unexplored.
CAPACITY TO MANAGE FINANCES
BACKGROUND
Along with medical decision making and driving, financial capacity is a vital aspect of individual autonomy in our society. Financial capacity comprises a broad range of conceptual, pragmatic, and judgment abilities that are critical to the independent functioning of adults in our society (Marson & Briggs, 2001; Marson, Sawrie, et al., 2000). In this way, it differs in many respects from medical decision-making capacity, which is primarily a verbally mediated capacity (Dymek et al., 1999). Epidemiological studies in the elderly population have suggested that financial capacity is an “advanced” activity of daily living (ADL), also called an instrumental ADL or IADL (Wolinsky & Johnson, 1991). The IADLs are mediated by higher cognitive function and can be distinguished from “household” ADLs (e.g., preparing meals, shopping, doing housework) and “basic” ADLs (e.g., bathing, dressing, walking; see Wolinsky & Johnson). Financial abilities range from basic skills of counting coins or currency to conducting cash transactions, managing a checkbook and bank statement, and executing a will, to higher level abilities of making contracts and deciding on investments. Financial abilities can vary substantially across individuals, depending on a person's socioeconomic status, occupational attainment, and overall financial experience (Marson, 2001; Marson & Briggs, 2001; Marson, Earnst, et al., 2000; Marson, Sawrie, et al., 2000).
CONCEPTUAL MODELS
Despite its importance, there have been few working conceptual models of financial capacity. One proposed model that combines cognitive neuropsychological and clinical aspects contains three elements. The first is declarative knowledge, which is the ability to describe facts, concepts, and events related to financial activities (knowledge of currency, concepts such as interest rate or loans, and personal financial data). The second is procedural knowledge, which is the ability to carry out motor based, overlearned practical financial skills and routines such as making change and writing checks. The third is judgment, which is the ability to make financial decisions consistent with self-interest, in both everyday and also novel or ambiguous situations (Marson, Sawrie, et al., 2000). From a clinical standpoint, this model views financial capacity at three levels: specific abilities (task level); broader areas of activity (domain level) that each have clinical relevance for independent functioning (e.g., conducting cash transactions; checkbook management; bill payment); and overall financial capacity (global level; see Marson, 2001).
EMPIRICAL WORK IN OLDER ADULTS WITH DEMENTIA
Empirical research in the area of financial capacity in older adults has only recently emerged. The financial skills of patients with AD are substantially impaired relative to healthy older controls (Marson, Sawrie, et al., 2000). In an initial study using the aforementioned model of financial capacity and an associated standardized assessment instrument, patients with mild AD demonstrated deficits in many complex financial abilities (tasks), and in almost all financial activities (domains; Marson et al.). Patients with moderate AD demonstrated loss of both simple and complex financial abilities, as well as severe impairment across all financial activities. A subsequent study demonstrated a marked difference in global financial capacity between participants with AD and those without it (Marson, 2001). Patients with dementia also demonstrate a lack of awareness of declining financial abilities relative to patients without dementia (Cramer, Tuokko, Mateer, & Hultsch, 2004), with loss of awareness occurring first for more complex tasks (Van Wielingen, Tuokko, Carmer, Mateer, & Hultsch, 2004).
Discrete financial skills are also impaired in patients with amnestic mild cognitive impairment (MCI), the precursor stage to AD (Griffith et al., 2003). Using the aforementioned model and instrument, Marson and colleagues found that MCI patients performed significantly below controls on domains tapping financial concepts, checkbook management, bank statement management, financial judgment, and bill payment. Compared with controls, MCI patients also showed a 1.74-SD decline in overall financial capacity. These results strongly suggested that decline in financial abilities is an aspect of functional change in MCI (Griffith et al.). In addition, memory functioning in patients with MCI has been linked to future impairments in money management (Tuokko, Morris, & Ebert, 2005).
SUMMARY AND FUTURE DIRECTIONS
Despite its importance, financial capacity has only recently begun to receive systematic research attention. Financial capacity is a complex, multifaceted construct. Given its central importance to independent functioning, there is a strong need for continued model building and instrument development in this area. The studies reviewed here represent researchers' initial efforts at empirically understanding financial capacity in dementia populations. Patients with preclinical dementia demonstrate focal impairments in financial skills that, in turn, become substantial and widespread by the time dementia advances. In future studies, researchers need to address issues of normative longitudinal change in financial capacity over the life course, the natural history of financial capacity loss in patients with dementia, and cognitive predictors of financial capacity.
CAPACITY ASSESSMENT IN THE 21ST CENTURY
Capacity assessment of older adults will become increasingly important over the coming century. Our aging society has a very strong interest in being able to accurately discriminate intact from impaired functioning in the older adult population (Marson, Sawrie, et al., 2000). The convergence of increased longevity, cognitive aging and dementia, blended families, and the intergenerational transfer of wealth in our individualistic society are making, and will continue to make, issues of capacity loss in older adults a prominent public policy concern.
The past 10 years has witnessed the emergence of capacity assessment in aging as a field of study, with a growing body of empirical studies, a promising first generation of capacity assessment instruments, and a small but growing cadre of scientific researchers. Two clinical areas that have received the most research attention are treatment consent capacity and financial capacity. These studies await replication, but they provide a departure point for expanded explorations of other capacity constructs.
For example, a critical area concerns the assessment of capacity to live independently, which is the basis for judgments of guardianship in probate court. This capacity comprises a domain so vast it can include almost all areas of functioning, and it may manifest itself in poorly understood behaviors such as “self-neglect” and with extreme unsanitary living conditions (Moye, 2003). Another key area requiring attention is testamentary capacity and the related issues of undue influence and exploitation of older adults with diminished capacity. Undue influence is a concept that appears in the law, but is not well defined clinically. It generally relates to some form of coercion of a vulnerable adult to do something that will benefit the coercer. These are increasingly common forensic issues in the courts, which unfortunately have correspondingly very little literature or knowledge from the psychological sciences to draw upon (Marson, Huthwaite, & Hebert, 2004). Two other areas that are almost without study are sexual consent capacity and voting capacity. The sexual consent issue arises with two older adults living in an institution who are intimate and at least one of whom has questionable capacity to consent to a sexual relationship (Lichtenberg & Strzepek, 1990). The recent presidential elections have highlighted the issue of voting capacity, particularly in patients with advanced dementia (Appelbaum, Bonnie, & Karlawish, 2005).
In addition to considering a wider range of capacities, it will be important for researchers to characterize the nature of capacity impairment within a wider range of older patient groups. For example, studies might focus on capacity impairment within dementia subtypes (AD, PD, diffuse Lewy body disease, and frontal lobe dementia), and within other neuropsychiatric illnesses such as schizophrenia and profound depression. Capacity issues in developmental disorders such as mental retardation and autism in older adults should also be explored. In short, we need to understand how capacity issues present in older adults across the spectrum of neuropsychiatric and developmental syndromes.
A third area for study is clinician decision making. Capacity assessments are ultimately human judgments occurring in a social context. It is therefore crucial that we understand how clinical judgments of decisional capacity relate to the social dynamics of decision making. We need more studies that look at how clinicians integrate multiple sources of capacity data with the elder's situation and values, and at the interrater reliability of clinician capacity judgments. These studies should also explore how clinicians from different disciplinary backgrounds may vary in their capacity assessment approach and outcomes.
A fourth area of empirical study involves identifying cognitive and other behavioral markers of diminished capacity. Neuropsychological studies of decisional capacity in dementia have provided important initial findings concerning the neuro-cognitive changes in the brain that presumably mediate loss of capacity, and that appear to strongly underlie the competency construct. Such studies will provide an empirical basis for clinicians to assess capacity and to predict future decisional abilities and needs of older adults for caregivers and families, attorneys and judges, and public health officials.
A solid empirical research base will be necessary to ensure the quality and accuracy of capacity determinations in the coming century. Capacity is a construct with clinical, ethical, and legal referents, and in this regard it may be unique among clinical constructs. Although a clinician's opinion is currently the accepted clinical standard for capacity determination—there is no “gold” standard—clinical judgments of capacity can often be inaccurate, unreliable, and even invalid. Thus, capacity assessment training should become a part of the clinical training of physicians, psychologists, and other health care professionals working with the elderly population (Karlawish & Schmitt, 2000; Marson, Sawrie, et al., 2000).
Finally, the many intersections of law and clinical practice in this area require more examination. Capacity research poses some unique challenges in that research design must, necessarily, be linked to legal definitions of capacity, as capacity is ultimately a legal matter. Yet the law is more a matter of social consensus than science, and as such it forms an unusual basis for scientific study (Moye, 2000). Thus a dynamic approach must be pursued in which science is based on but not restricted by law and, one would hope, subsequently informs the law.
Accordingly, studies are needed of the relationship between legal and clinical models of capacity, and of the relationship between clinical assessments and juridical actions (e.g., what kind of capacity assessments lead to optimal judicial orders). An important goal of clinical capacity assessment is to assist judges and other legal professionals in crafting legal interventions that are specifically tailored to the needs of individual clients, and that clearly identify needs for protection while simultaneously protecting rights in areas of preserved capacity. Within the law, there is a growing movement away from full (plenary) guardianship orders to limited orders that provide surrogate controls only in needed areas. Thus vigorous interdisciplinary collaboration between legal and clinical professionals, and also public policy makers, is vital to the continuing development of capacity assessment as a field, and to its success as a societal mechanism for resolving individual issues of autonomy and protection.
American Bar Association Commission on Law and Aging and American Psychological Association. ( 2005). Assessment of older adults with diminished capacity: A handbook for lawyers. Washington, DC: American Bar Association.Google Scholar
American Bar Association Commission on Law and Aging and American Psychological Association. (in press). Judicial determination of capacity of older adults in guardianship proceedings. Washington, DC: American Bar Association.Google Scholar
Anderer, S. J. ( 1997). Development of an instrument to evaluate the capacity of elderly persons to make personal care and financial decisions. Unpublished doctoral dissertation. Allegheny University of the Health Sciences.Google Scholar
Appelbaum, P. S. ( 1982). Competency to consent to research: A psychiatric overview. Archives of General Psychiatry, 39, 951– 958.Crossref, Google Scholar
Appelbaum, P. S., & Bateman, A. ( 1980). Empirical assessment of competency to consent to psychiatric hospitalization. American Journal of Psychiatry, 138, 1170– 1176.Google Scholar
Appelbaum, P. S., Bonnie, R. J., & Karlawish, J. H. T. ( 2005). The capacity to vote of persons with Alzheimer's disease. American Journal of Psychiatry, 162, 2094– 2100.Crossref, Google Scholar
Appelbaum, P. S., & Grisso, T. ( 1988). Assessing patients' capacities to consent to treatment. New England Journal of Medicine, 319, 1635– 1638.Crossref, Google Scholar
Appelbaum, P. S., & Grisso, T. ( 1995). The MacArthur Treatment Competency Study 1: Mental illness and competence to consent to treatment. Law and Human Behavior, 19, 105– 126.Crossref, Google Scholar
Appelbaum, P. S., & Grisso, T. ( 2001). MacArthur Competence Assessment Tool for Clinical Research (MacCAT-CR). Sarasota, FL: Professional Resource Press.Google Scholar
Appelbaum, P. S., & Roth, L. ( 1981). Clinical issues in the assessment of competence. American Journal of Psychiatry, 138, 1462– 1467.Crossref, Google Scholar
Barton, C. D., Mallik, H. S., Orr, W. B., & Janofsky, J. S. ( 1996). Clinicians' judgement of capacity of nursing home patients to give informed consent. Psychiatric Services, 47, 956– 960.Crossref, Google Scholar
Bean, G., Nishisato, S., Rector, N. A., & Glancy, G. ( 1996). The assessment of competence to make a treatment decision: An empirical approach. Canadian Journal of Psychiatry, 41, 85– 92.Crossref, Google Scholar
Berg, J. W., Appelbaum, P. S., Lidz, C. W., & Parker, L. S. ( 2001). Informed consent: Legal theory and clinical practice. New York: Oxford University Press.Google Scholar
Caralis, P. V., Davis, B., Wright, K., & Marcial, E. ( 1993). The influence of ethnicity and race on attitudes towards advance directives, life-prolonging treatments, and euthanasia. The Journal of Clinical Ethics, 4, 155– 165.Google Scholar
Carney, M. T., Neugroschl, J., Morrison, R. S., Marin, D., & Siu, A. L. ( 2001). The development and piloting of a capacity assessment tool. The Journal of Clinical Ethics, 12, 17– 23.Google Scholar
Cramer, K., Tuokko, H., Mateer, C., & Hultsch, D. ( 2004). Measuring awareness of financial skills: Reliability and validity of a new measure. Aging and Mental Health, 8, 161– 171.Crossref, Google Scholar
Dellasega, C., Frank, L., & Smyer, M. ( 1996). Medical decision-making capacity in elderly hospitalized patients. Journal of Ethics, Law and Aging, 2, 65– 74.Google Scholar
Drane, J. F. ( 1985). The many faces of competency. Hastings Center Report, 15, 17– 21.Google Scholar
Dunn, L. B., & Jeste, D. V. ( 2001). Enhancing informed consent for research and treatment. Neuropsychopharmacology, 24, 595– 607.Crossref, Google Scholar
Dymek, M. P., Atchison, P., Harrell, L., & Marson, D. C. ( 2001). Competency to consent to medical treatment in cognitively impaired patients with Parkinson's disease. Neurology, 56, 17– 24.Crossref, Google Scholar
Dymek, M. P., Marson, D. C., & Harrell, L. ( 1999). Factor structure of capacity to consent to medical treatment in patients with Alzheimer's disease: An exploratory study. Journal of Forensic Neuropsychology, 1, 27– 48.Crossref, Google Scholar
Earnst, K. S., Marson, D. C., & Harrell, L. E. ( 2000). Cognitive model of physicians' legal standard and personal judgments of competency in patients with Alzheimer's disease. Journal of the American Geriatric Society, 48, 919– 927.Crossref, Google Scholar
Eleazer, G. P., Hornung, C. A., Egbert, C. B., Egbert, J. R., Eng, C., & Hedgepeth, J., et al. ( 1996). The relationship between ethnicity and advance directives in a frail older population. Journal of the American Geriatrics Society, 44, 938– 943.Crossref, Google Scholar
Elchells, E., Darzins, P., Silberfeld, M., Singer, P. A., McKenny, J., & Naglie, G., et al. ( 1999). Assessment of patients' capacity to consent to treatment. Journal of General Internal Medicine, 14, 27– 34.Crossref, Google Scholar
Fitten, L. J., Lusky, R., & Hamann, C. ( 1990). Assessing treatment decision-making capacity in elderly nursing home residents. Journal of the American Geriatrics Society, 38, 1097– 1104.Crossref, Google Scholar
Fitten, L. J., & Waite, M. S. ( 1990). Impact of medical hospitalization on treatment decision making capacity in the elderly. Archives of Internal Medicine, 150, 1717– 1721.Crossref, Google Scholar
Frank, L., Smyer, M., Grisso, T., & Applebaum, P. ( 1999). Measurement of advance directive and medical treatment decision-making capacity of older adults. Journal of Mental Health and Aging, 5, 257– 274.Google Scholar
Ganzini, L., Volicer, L., Nelson, W., & Derse, A. ( 2003). Pitfalls in the assessment of decision-making capacity. Psychosomatics, 44, 237– 243.Crossref, Google Scholar
Griffith, H., Belue, K., Sicola, A., Krzywanski, S., Zamrini, E., Harrell, L., & Marson D.C. ( 2003). Impaired financial abilities in mild cognitive impairment: A direct assessment approach. Neurology, 60, 449– 457.Crossref, Google Scholar
Grisso, T. ( 1986). Evaluating Competencies: Forensic Assessments and Instruments. New York, NY: Plenum Press.Google Scholar
Grisso, T. ( 2003). Evaluating competences, 2nd edition. New York: Plenum.Google Scholar
Grisso, T., & Appelbaum, P. S. ( 1995). The MacArthur Treatment Competency Study III: Abilities of patients to consent to psychiatric and medical treatment. Law and Human Behavior, 19, 149– 174.Crossref, Google Scholar
Grisso, T., & Appelbaum, P. S. ( 1998a). Assessing competence to consent to treatment. New York: Oxford University Press.Google Scholar
Grisso, T., & Appelbaum, P. S. ( 1998b). MacArthur Competency Assessment Tool for Treatment (MacCAT-T). Sarasota, FL: Professional Resource Press.Google Scholar
Gurrera, R. J., Moye, J., Karel, M. J., Azar, A. R., & Armesto, J. C. ( 2006). Cognitive performance predicts treatment decisional abilities in mild to moderate dementia. Neurology, 66, 1367– 1372.Crossref, Google Scholar
Havens, J. J., & Schervish, P. G. ( 2003). Why the $41 trillion wealth transfer estimate is still valid: A review of challenges and questions. The Journal of Gift Planning, 7, 11– 15, 47–50.Google Scholar
Huthwaite, J., Martin, R., Griffith, H. R., Anderson, B., Harrell, L., & Marson, D. (in press). Declining medical decision-making capacity in mild Alzheimer's disease: A two-year longitudinal study. Behavioral Sciences and the Law.Google Scholar
Jahng, K. H., Martin, L. R., Golin, C. E., & DiMattco, M. R. ( 2005). Preferences for medical collaboration: Patient-physician congruence and patient outcomes. Patient Education and Counseling, 57, 308– 314.Crossref, Google Scholar
Kapp, M. ( 1992). Geriatrics and the law: Patient rights and professional responsibilities. New York: Springer.Google Scholar
Kapp, M. B., & Mossman, D. ( 1996). Measuring decisional capacity: Cautions on the construction of a “capacimeter.” Psychology, Public Policy, and Law, 2, 73– 95.Crossref, Google Scholar
Karel, M. J. ( 2000). The assessment of values in medical decision making. Journal of Aging Studies, 14, 403– 422.Crossref, Google Scholar
Karlawish, J. H. T., & Schmitt, F. A. ( 2000). Why physicians need to become more proficient in assessing their patients' competency and how they can achieve this. Journal of the American Geriatrics Society, 48, 1014– 1016.Crossref, Google Scholar
Kim, S. Y. H., Caine, E. D., Currier, G. W., Leibovici, A., & Ryan, J. M. ( 2001). Assessing the competence of persons with Alzheimer's disease in providing informed consent for participation in research. American Journal of Psychiatry, 158, 712– 717.Crossref, Google Scholar
Kim, S. Y. H., Karlawish, J. H. T., & Caine, E. D. ( 2002). Current state of research on decision-making competence of cognitively impaired elderly persons. American Journal of Geriatric Psychiatry, 10, 151– 165.Crossref, Google Scholar
Krynski, M. D., Tymchuk, A. J., & Ouslander, J. G. ( 1994). How informed can consent be? New light on comprehension among elderly people making decisions about enteral tube feeding. The Gerontologist, 34, 36– 43.Crossref, Google Scholar
Lichtenberg, P. A., & Strzepek, D. M. ( 1990). Assessments of institutionalized dementia Patients' competencies to participate in intimate relationships. The Gerontologist, 30, 117– 120.Crossref, Google Scholar
Loeb, P. ( 1996). Independent living scales. San Antonio: Psychological Corporation.Google Scholar
Markson, L. J., Kern, D. C., Annas, G. J., & Glantz, L. H. ( 1994). Physician assessment of patient competence. Journal of American Geriatrics Society, 42, 1074– 1080.Crossref, Google Scholar
Marson, D. C. ( 2001). Loss of financial competency in dementia: Conceptual and empirical approaches. Aging, Neuropsychology, and Cognition, 8, 164– 181.Crossref, Google Scholar
Marson, D. C., Annis, S. M., McInturff, B., Bartolucci, A., & Harrell, L. E. ( 1999). Error behaviors associated with loss of competency in Alzheimer's disease. Neurology, 53, 1983– 1992.Crossref, Google Scholar
Marson, D. C., & Briggs, S. ( 2001). Assessing competency in Alzheimer's disease: Treatment consent capacity and financial capacity. In S. Gauthier & J. L. Cummings (Eds.), Alzheimer's disease and related disorders annual: 2001. London: Martin Dunitz.Google Scholar
Marson, D. C., Chatterjee, A., Ingram, K. K., & Harrell, L. E. ( 1996). Toward a neurologic model of competency: Cognitive predictors of capacity to consent in Alzheimer's disease using three different legal standards. Neurology, 46, 666– 672.Crossref, Google Scholar
Marson, D. C., Cody, H. A., Ingram, K. K., & Harrell, L. E. ( 1995). Neuropsychological predictors of competency in Alzheimer's disease using a rational reasons legal standard. Archives of Neurology, 52, 955– 959.Crossref, Google Scholar
Marson, D. C., Earnst, K., Jamil, F., Bartolucci, A., & Harrell, L. E. ( 2000). Consistency of Physicians' legal standard and personal judgments of competency in patients with Alzheimer's disease. Journal of the American Geriatrics Society, 48, 911– 918.Crossref, Google Scholar
Marson, D. C., Hawkins, L., McInturff, B., & Harrell, L. E. ( 1997). Cognitive models that predict physician judgments of capacity to consent in mild Alzheimer's disease. Journal of the American Geriatrics Society, 45, 458– 464.Crossref, Google Scholar
Marson, D. C. Huthwaite, J., & Hebert, K. ( 2004). Testamentary capacity and undue influence in the elderly: A jurisprudent therapy perspective. Law and Psychology Review, 28, 71– 96.Google Scholar
Marson, D. C., & Ingram, K. ( 1996). Competency to consent to research: A growing field of research. Journal of Ethics, Law, and Aging, 2, 59– 63.Google Scholar
Marson, D. C., Ingram, K. K., Cody, H. A., & Harrell, L. E. ( 1995). Assessing the competency of patients with Alzheimer's disease under different legal standards. Archives of Neurology, 52, 949– 954.Crossref, Google Scholar
Marson, D. C., McInturff, B., Hawkins, L., Bartolucci, A., & Harrell, L. E. ( 1997). Consistency of physician judgments of capacity to consent in mild Alzheimer's disease. The American Geriatrics Society, 45, 453– 457.Crossref, Google Scholar
Marson, D. C., Sawrie, S., Snyder, S., McInturff, B., Stalvey, T., & Boothe, A., et al. ( 2000). Assessing financial capacity in patients with Alzheimer's disease: A conceptual model and prototype instrument. Archives of Neurology, 57, 877– 884.Crossref, Google Scholar
Meisel, A., Roth, L., & Lidz, C. W. ( 1977). Toward a model of the legal doctrine of informed consent. American Journal of Psychiatry, 134, 285– 289.Crossref, Google Scholar
Moye, J. ( 2000). Mr. Franks refuses surgery—cognition and values in competency determination in complex cases. Journal of Aging Studies, 14, 385– 401.Crossref, Google Scholar
Moye, J. ( 2003). Guardianship and conservatorship. In T. Grisso (Ed.), Evaluating competencies. (pp. 309– 390). New York: Plenum Press.Google Scholar
Moye, J., Gurrera, R. J., Karel, M. J., Edelstein, B., & O'Connell, C. ( 2006). Empirical advances in the assessment of the capacity to consent to medical treatment: Clinical implications and research needs. Clinical Psychology Review, 26, 1054– 1077.Crossref, Google Scholar
Moye, J., & Karel, M. ( 1999). Evaluating decisional capacities in older adults: Results of two clinical studies. Advances in Medical Psychology, 10, 71– 84.Google Scholar
Moye, J., Karel, M. J., & Armesto, J. C. ( 2007). Evaluating capacity to consent to treatment. In A. M. Goldstein (Ed.), Forensic psychology: Emerging topics and expanding roles. (pp. 260– 293). Hoboken, NJ: Wiley.Google Scholar
Moye, J., Karel, M. J., Azar, A. R., & Gurrera, R. J. ( 2004a). Capacity to consent to treatment: Empirical comparison of three instruments in older adults with and without dementia. The Gerontologist, 44, 166– 175.Crossref, Google Scholar
Moye, J., Karel, M. J., Azar, A. R., & Gurrera, R. J. ( 2004b). Hopes and cautions for instrument- based evaluations of consent capacity: Results of a construct validity study of three instruments. Ethics, Law, and Aging Review, 10, 39– 61.Google Scholar
Moye, J., Karel, M. J., Gurrera, R. J., & Azar, A. R. ( 2006). Neuropsychological predictors of decision-making capacity over 9 months in mild to moderate dementia. Journal of General Internal Medicine, 21, 78– 83.Crossref, Google Scholar
National Center on Elder Abuse. ( 2005). Fifteen questions and answers about elder abuse. Washington, DC: Author.Google Scholar
National Conference of Commissioners on Uniform State Laws, ( 1993). Uniform Health Care Decisions Act. Retrieved November 10, 2006. from http://www.law.upcnn.edu/bll/ulc/fnact99/1990s/uhcda93.pdfGoogle Scholar
Pruchno, R. A., Smyer, M. A., Rose, M. S., Hartman-Stein, P. E., & Laribee-Henderson, D. L. ( 1995). Competence of long-term care residents to participate in decisions about their medical care: A brief, objective assessment. The Gerontologist, 35, 622– 629.Crossref, Google Scholar
Roth, L. H., Meisel, C. A., & Lidz, C. A. ( 1977). Tests of competency to consent to treatment. Canadian Journal of Psychiatry, 134, 279– 284.Google Scholar
Royall, D. R., Cordes, J., & Polk, M. ( 1997). Executive control and the comprehension of medical information by elderly retirees. Experimental Aging Research, 23, 301– 313.Crossref, Google Scholar
Rutman, D., & Silberfeld, M. ( 1992). A preliminary report on the discrepancy between clinical and test evaluations of competency. Canadian Journal of Psychiatry, 37, 634– 639.Crossref, Google Scholar
Sabatino, C. ( 1996). Competency: Refining our legal fictions. In M. Smyer, K. W. Schaie, & M. B. Kapp (Eds.), Older adults' decision making and the law. (pp. 1– 28). New York: Springer.Google Scholar
Saks, E. R., Dunn, L. B., Marshall, B. J., Nayak, G. V., Golshan, S., & Jeste, D. V. ( 2002). The California Scale of Appreciation: A new instrument to measure the appreciation component of capacity to consent to research. American Journal of Geriatric Psychiatry, 10, 166– 174.Crossref, Google Scholar
Schmand, B., Gouwenberg, B., Smit, J. H., & Jonker, C. ( 1999). Assessment of mental competency in community-dwelling elderly. Alzheimer Disease and Associated Disorders, 13, 80– 87.Crossref, Google Scholar
Smyer, M. A., Schaie, K. W., & Kapp, M. B. ( 1996). Older adults decision-making and the law. New York: Springer.Google Scholar
Staats, N., & Edelstein, B. ( 1995). Cognitive changes associated with the declining competency of older adults. Paper presented at
Staats, N., Edelstein, B., & Null, J. ( 1995). Neuropsychological correlates of thinking rationally about treatment tests. Paper presented at
Stanley, B., Stanley, M., Guido, J., & Garvin, L. ( 1988). The functional competency of elderly at risk. The Gerontologist, 28( Suppl. June 1988), 53– 58.Google Scholar
Sturman, E. D. ( 2005). The capacity to consent to treatment and research: A review of standardized assessment tools. Clinical Psychology Review, 25, 954– 974.Crossref, Google Scholar
Taub, H. A., Baker, M. T., Kline, G. E., & Sturr, J. F. ( 1987). Comprehension of informed consent by young-old and old-old volunteers. Experimental Aging Research, 13, 173– 178.Crossref, Google Scholar
Tepper, A., & Elwork, A. ( 1984). Competency to consent to treatment as a psycho-legal construct. Law and Human Behavior, 8, 205– 223.Crossref, Google Scholar
Tuokko, H., Morris, C., & Ebert, P. ( 2005). Mild cognitive impairment and everyday functioning in older adults. Neurocase, 11, 40– 47.Crossref, Google Scholar
Tymchuk, A. J., Ouslander, J. G., & Fitten, J. ( 1988). Medical decision-making among elderly people in long term care. The Gerontologist, 28, 59– 63.Crossref, Google Scholar
Van Wielingen, L., Tuokko, H., Carmer, K., Mateer, C., & Hultsch, D. ( 2004). Awareness of financial skills in dementia. Aging and Mental Health, 8, 374– 380.Crossref, Google Scholar
Wolinsky, F., & Johnson, R. ( 1991). The use of health services by older adults. Journal of Gerontology: Social Sciences, 46, S345– S357.Crossref, Google Scholar
Wong, J. G., Cheung, E. P., & Chen, E. Y. ( 2005). Decision-making capacity of inpatients with schizophrenia in Hong Kong. Journal of Nervous and Mental Disease, 193, 316– 322.Crossref, Google Scholar
Wong, J. G., Clare, I. C. H., Holland, A. J., Watson, P. C., & Gunn, M. ( 2000). The capacity of people with a “mental disability” to make a health care decision. Psychological Medicine, 30, 295– 306.Crossref, Google Scholar