Anxiety Disorders and Comorbid Medical Illness
Abstract
Objective:
To provide an overview of the role of anxiety disorders in medical illness. Method: The Anxiety Disorders Association of America held a multidisciplinary conference from which conference leaders and speakers reviewed presentations and discussions, considered literature on prevalence, comorbidity, etiology and treatment, and made recommendations for research. Irritable bowel syndrome (IBS), asthma, cardiovascular disease (CVD), cancer and chronic pain were reviewed. Results: A substantial literature supports clinically important associations between psychiatric illness and chronic medical conditions. Most research focuses on depression, finding that depression can adversely affect self-care and increase the risk of incident medical illness, complications and mortality. Anxiety disorders are less well studied, but robust epidemiological and clinical evidence shows that anxiety disorders play an equally important role. Biological theories of the interactions between anxiety and IBS, CVD and chronic pain are presented. Available data suggest that anxiety disorders in medically ill patients should not be ignored and could be considered conjointly with depression when developing strategies for screening and intervention, particularly in primary care. Conclusions: Emerging data offer a strong argument for the role of anxiety in medical illness and suggest that anxiety disorders rival depression in terms of risk, comorbidity and outcome. Research programs designed to advance our understanding of the impact of anxiety disorders on medical illness are needed to develop evidence-based approaches to improving patient care.
(Reprinted with permission from General Hospital Psychiatry 2008; 30:208–225)
INTRODUCTION
Mental disorders occur with chronic medical conditions in many patients, causing significant role impairment, work loss and work cut-back (1, 2). Depression increases symptom burden and functional impairment and worsens prognosis for heart disease, stroke, diabetes mellitus, HIV/AIDS, cancer and other chronic illnesses (3–5). One nationally representative survey of over 130,000 Canadian adults demonstrated that depression independently increased role impairment by 21% compared to healthy controls. However, when depression occurred along with chronic lung disease, diabetes mellitus or heart disease, the rate of disability increased by over 50% (5). A more complete understanding of the adverse effect of depression on biological and self-care (e.g., adherence to diet, smoking cessation, exercise, medications) mechanisms and findings from treatment studies is emerging to guide patient care (6–14). These data paint a compelling picture of the importance of depression in medical illness.
Much less is known about the impact of anxiety disorders on function and outcome in persons with chronic medical illness. There is convincing evidence that anxiety is associated with high rates of medically unexplained symptoms and increased utilization of healthcare resources (4, 15–19). Moreover, anxiety disorders are strongly and independently associated with chronic medical illness (20, 21), low levels of physical health-related quality of life, and physical disability (21–24). Indeed, the disability and related poor physical and economic outcomes associated with anxiety disorders may be as great as with depression. In a sample of 480 primary care patients, the probability of missing time from work in the prior month for persons with an anxiety disorder (OR: 2.22) was as great as for persons with major depression (OR: 2.15) (25). In patients with diabetes, comorbid panic disorder had a significant adverse effect on symptom burden, functional impairment and HbA1c levels after controlling for depression (23). In the National Comorbidity Survey-Replication (NCS-R), Kessler et al. (1) reported that various anxiety disorders had equal or greater association than depression with four chronic physical disorders (i.e., hypertension, arthritis, asthma, ulcers) (Fig. 1).Similarly, the number of 30-day role impairment days associated with anxiety disorders among respondents with these four chronic medical disorders was similar or greater to that seen in association with depression and dysthymia (Fig. 2) (1).
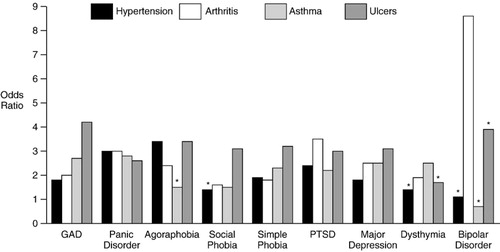
Figure 1. Associations (Odds Ratios) of DSM-III-R Mental Disorders Among NCS-R Respondents With Chronic Physical Disorders
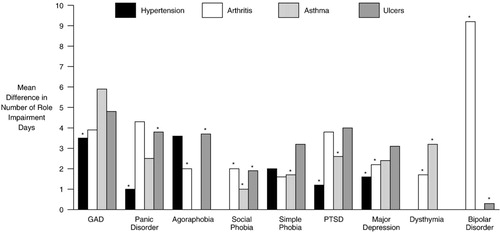
Figure 2. Number of 30-Day Role Impairment Days Associated With Comorbid DSM-III-R Mental Disorders Among NCS-R Respondents With Chronic Physical Disorders
In recognition of the need to better understand and illustrate the effect of anxiety disorders on persons with chronic medical illnesses and with the hope of developing treatment strategies, the Anxiety Disorders Association of America (ADDA) convened a multidisciplinary conference on January 30 31, 2006, to review current data on the relationship between anxiety disorders and specific medical illnesses. Presenters and discussants included clinicians and researchers in psychiatry, psychology, primary care, healthcare systems, epidemiology, public health, healthcare policy and advocacy. The proceedings of the conference are summarized in this paper, which reviews anxiety disorders in the context of functional gastrointestinal disorders, asthma, heart disease, cancer and chronic pain. These selective reviews mainly focused on anxiety disorders per se and did not investigate numerous studies focused on “stress”. In addition, specific recommendations are made for furthering the basic science and clinical research agenda to better understand the impact of anxiety disorders on medical illness and improve clinical outcomes and patient care.
ANXIETY DISORDERS AND COMORBID MEDICAL ILLNESS
FUNCTIONAL GASTROINTESTINAL DISEASES
Epidemiology.
Irritable bowel syndrome (IBS) is characterized by chronic, unexplained abdominal pain or discomfort associated with diarrhea, constipation, or both (26). It is one of the most common and well studied of the 28 functional gastrointestinal disorders (FGIDs) (27), affecting an estimated 10% to 25% of the population and occurring in women twice as frequently as in men. A key feature of IBS is visceral hyperalgesia, defined as abnormally exaggerated visceral pain responses from gut events (e.g., experimental colonic distension, meals, infection/inflammation) (27–29). Stress reactivity is considered an extremely important nondiagnostic feature of IBS (27, 29) and is characteristic of other disorders with which IBS most frequently overlaps, such as anxiety disorders, mood disorders and other functional somatic disorders.
There is a strong association between IBS and psychiatric diagnoses, particularly anxiety disorders (30). Rates of psychiatric diagnoses range from 54% to 94% in treatment-seeking patients with IBS (31, 32). Rates of anxiety and mood disorders in patients with IBS are significantly higher than in patients with inflammatory bowel disease (33). When psychiatric disorders co-exist with IBS, gastrointestinal symptoms are typically more severe and disabling. In a survey of university students. IBS was associated with high rates of generalized anxiety disorder (GAD) and higher levels of neuroticism, visceral anxiety, anxiety sensitivity and worry than in those without (34). A community-based survey of 3911 adults in the USA found that rates of panic disorder, generalized social anxiety disorder, posttraumatic stress disorder (PTSD) and major depression were significantly higher in respondents with IBS than in those without IBS, but that rates of psychiatric diagnoses in treatment-seekers were remarkably similar to non-treatment-seeking persons with IBS. Both treatment-seeking and non-treatment-seeking groups with IBS reported greater levels of functional impairment than non-IBS groups (35, 36). In a re-analysis of the Epidemiologic Catchment Area study (N = 13,537), respondents with panic disorder were nearly five times as likely to have IBS-like symptoms than those with no psychiatric diagnosis (37). The rate of IBS among persons with panic disorder appears to be over twice that of those without panic disorder (37). The temporal relationship between onset of anxiety disorders and IBS is not well studied, although one study found that IBS subjects with anxiety disorders were significantly more likely to report that the anxiety disorder preceded the onset of IBS (39). Up to one-third of IBS patients have PTSD (40), and prior physical/sexual abuse and PTSD are more frequent in women with IBS than in those with equally severe organic gastrointestinal disorders and are predictive of increased vulnerability for the onset or worsening of IBS (41, 42).
Pathophysiology.
There are multiple, nonexclusive potential etiologies for IBS, including inherited risk, infection/inflammation, severe traumatic events and psychiatric disorders, all of which may play a role in the onset or exacerbation of existing IBS symptoms (27, 43). Psychosocial stress is increasingly recognized as playing an important role in the onset, persistence and severity of IBS, regardless of presumed etiology (i.e., infections, stress-related, inherited risk) (44, 45). Sensitized central stress circuits may be important mediators of the distorted visceral perception/hyperalgesia and stress reactivity observed in IBS (45, 46), consistent with preclinical and clinical evidence that anxiety and stress can induce or worsen existing visceral hyperalgesia (47, 48).
The neural pathways that process visceral pain signals also regulate the stress response, anxiety, mood and gastrointestinal function (28). A key mediator of these pathways is the neuropeptide corticotropin-releasing factor (CRF). Exposure to prolonged or severe stress, especially in vulnerable individuals, can result in persistent changes in CRF activity with dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, extra-hypothalamic and peripheral CRF neural systems that mediate responses to stress, visceral hypersensitivity, colonic motility, immune response and fear conditioning (28, 38). If stress is sufficiently severe or persistent, the stress response may not be completely terminated, leading to continued CRF hyperactivity and release of stress mediators, including pro-inflammatory cytokines and catecholamines, resulting in sustained excessive inflammatory activity. There is some evidence, although not entirely consistent in direction, for HPA abnormalities and altered pro-inflammatory cytokine activity in IBS (45, 49) and several disorders commonly overlapping with IBS (e.g., fibromyalgia, chronic fatigue, anxiety disorders, including PTSD, and mood disorders) (50). Thus, CRF dysregulation may be one potential neurobiological link among these seemingly unrelated, stress-reactive conditions (45, 46, 50). Antidepressants (51) and cognitive behavioral therapy (CBT) (52), both of which are effective in IBS and in reducing stress reactivity, may reduce circulating pro-inflammatory cytokines or improve immune function in individuals with stress-related disorders.
An emerging neuroimaging literature suggests that, compared to healthy controls, experimental rectal distension is associated with altered reactivity of the anterior cingulate cortex, a brain region implicated in pain perception, anxiety, stress and prior trauma in persons with IBS (53). Recognition of the shared neurobiological underpinnings theoretically linking anxiety and stress may eventually provide the basis for mechanism-based psychotherapeutic and psychopharmacologic treatments for IBS (35).
Treatment.
Patients with mild IBS symptoms are generally seen in primary care settings and do not have significant functional impairment or psychological symptoms. Treatment for mild IBS focuses on education about the causes and course of IBS, reassurance of patients' concerns, and restrictions of foods and medications that exacerbate symptoms. Psychological treatments are usually reserved for patients with moderate or severe IBS symptoms and for patients with pain (Fig. 3)(27, 54). A meta-analysis of 32 psychotherapy trials in patients with IBS concluded that, despite the small sample sizes and nonstandardized methods, evidence exists to support the efficacy of psychological treatments in reducing IBS symptom severity compared to control conditions. Cognitive-behavioral therapy, which is the best studied intervention, teaches patients to regulate symptoms of IBS and alter behavior that reinforces or exacerbates symptoms (55, 56). Different psychotherapeutic techniques, including CBT, relaxation training, interpersonal psychotherapy and hypnotherapy, can be used in combination (54).
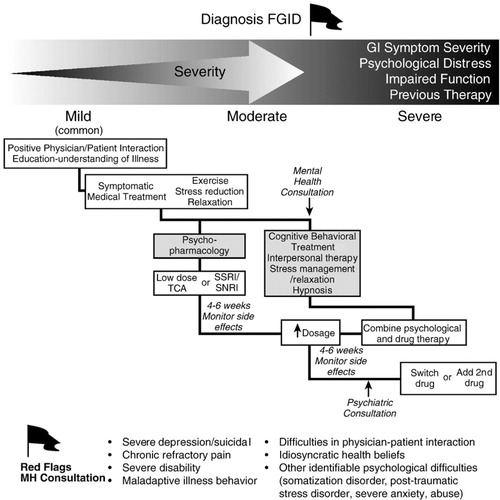
Figure 3. Rome III Guidelines for the Medical and Psychological Treatment of IBS.
Antidepressants and anxiolytics are prescribed for patients with IBS for their effects on anxiety and mood as well as for direct analgesic effects. In their summary of the psychopharmacologic treatment literature, Levy et al. (54) suggested that the tricyclic antidepressants (TCAs) are more beneficial than the selective serotonin reuptake inhibitors (SSRIs), possibly due to the central analgesic actions associated with the noradrenergic properties of the TCAs. Nonetheless, the SSRIs are effective for underlying anxiety and depression, and there is emerging evidence that these newer agents are effective for IBS sufferers without psychiatric disorders (57). The benzodiazepines have had a limited place in the treatment of IBS because of concern over potential abuse and withdrawal. However, the limited available literature suggests that benzodiazepine treatment of anxiety is associated with improvement in anxiety and IBS (58, 59). The nonbenzodiazepine anxiolytic agent, buspirone, may have a role in the treatment of IBS, but studies are needed to support its use in this population. As in the treatment of anxiety disorders and depression, psycho-pharmacologic treatment should not be abandoned until the dose and duration of therapy are optimized (54).
ASTHMA
Epidemiology.
Asthma is a chronic lung condition characterized by episodic inflammation and small airway constriction that can occur in response to environmental and other triggers. More than 30 million Americans have asthma, of whom 30% are children under the age of 18. Asthma ranges in severity from mild to life-threatening with an intermittent or persistent course. Age-adjusted mortality in 2003 was 1.4/100,000 population, with higher rates in African-Americans, women and the elderly. The prevalence of asthma has increased substantially over the past several decades, making it the most common chronic disease among youth worldwide, though the causes of this increase are unknown. Although death rates are stabilizing or decreasing, possibly due to improvements in medical care, asthma continues to pose a substantial economic burden. The total cost of asthma in 2004 was US$16 billion, US$11.5 billion due to direct healthcare costs (including US$5 billion in prescription drug costs) and US$4.6 billion in indirect costs associated with lost productivity at work and school and mortality (60). While there is no cure for asthma, the vast majority of persons with asthma can live symptom-free and without functional impairment with adequate routine medical care and adherence to asthma treatment. Yet, poor asthma control remains a problem among a substantial proportion of the population. As such, ongoing research aims to identify factors associated with poor asthma control. Recent evidence suggests that mental disorders may play a role in various aspects of onset and course of asthma and are the subject of studies designed to better understand this relationship.
Findings from community-based epidemiologic studies in youth and adults demonstrate a strong and consistent association between asthma and anxiety disorders (61–66). In contrast, available evidence on the link between asthma and depression is somewhat mixed (63, 67–69). The majority of studies to date on the link between mental disorders and asthma have relied on patient self-reports or parental reports of asthma. However, one study that examined the relationship between physician-diagnosed asthma and mental disorders found that anxiety disorders were significantly associated with both nonsevere [OR: 1.51 (1.00–2.32); P<.05) and severe asthma [OR: 2.09 (1.30–3.36); P<.05] (64), in contrast to the weaker and nonsignificant associations for mood disorders with lifetime nonsevere [OR: 1.44 (0.94–2.19)] or severe asthma [OR: 1.21 (0.75–1.98)]. Of note, nonsevere asthma (past 4 weeks) was significantly associated with increased likelihood of any affective disorder [OR: 2.42 (1.03–5.72); P<.05], while bipolar disorder was very strongly associated with lifetime severe asthma [OR: 5.64 (1.95–16.35); P<.05]. Panic disorder, panic attacks, GAD and phobias appear to be the anxiety disorders most strongly associated with asthma (64). Another study compared 769 youth with physician-diagnosed asthma to 582 age-matched controls and found an approximately twofold increase in the prevalence of one or more anxiety or depressive disorders, with greater rates of anxiety compared to mood disorders, and a significant correlation between anxiety sensitivity and asthma severity (70).
Clinical studies assessing the rates of mental disorders in patients with asthma, although largely limited to relatively small sample sizes and self-reported asthma status, have consistently found high rates of anxiety disorders in children, adolescents and adults (Table 1). Few studies have been able to control for potentially confounding or mediating factors in the links between asthma and mental disorders, such as smoking or use of asthma medications (78). One study found that adolescents with a history of life-threatening asthma attacks are more likely to have symptoms of PTSD, which was directly related to the life-threatening experiences associated with asthma, compared to less severely ill patients or healthy controls (73). Another study examined the relationship between PTSD symptoms and asthma among male twins and found the association was not explained by common genetic factors (79).
 |
Table 1. Anxiety Disorders in Clinical Samples of Patients With Asthma
One study of adolescents with asthma found that, after controlling for severity of asthma, the presence of an anxiety or depressive disorder was associated with an increased number of days with asthma symptoms in the past 2 weeks (mean: 5.4 days) compared to adolescents without these psychiatric diagnoses (mean: 3.5 days; P<.001), and that the number of anxiety-depressive symptoms was strongly associated with higher levels of asthma symptoms (P <.001) (80). The presence of anxiety disorders or other psychiatric diagnoses did not correlate with asthma severity in two studies of adult patients in asthma clinics (76, 81) or one large, primary care-based study (70). Findings for depression are somewhat equivocal, with some studies suggesting that depression is prevalent (74–77).
Nonetheless, poor asthma control, increased functional impairment, decreased quality of life, and utilization and cost of healthcare resources have been shown to be strongly associated with anxiety and mood disorders among persons with asthma (80, 82). Patients with comorbid asthma plus anxiety or mood disorders are more likely to use bronchodilators in the previous week (P<.02), have lower scores on asthma-control rating scales (P<.001) (e.g., nocturnal waking, activity limitation, wheezing, increased use of asthma medications, pulmonary function tests) (81) and lower quality of life as measured by activity limitation, asthma symptoms, environmental stimuli and emotional distress (P<.001) (81). Patients with asthma and a comorbid psychiatric diagnosis, including an anxiety disorder, are 4.9 times more likely to use an emergency room and 3.8 times more likely to be hospitalized (76), but few patients are treated for their mental disorder (81). Despite these robust data, comorbid anxiety and depressive disorders are only accurately diagnosed in approximately 40% of asthmatic patients in primary care (83). There are also a number of clinical and community-based studies that have found links between asthma and suicidal ideation (63, 84), suicide attempts and completed suicide (84). As suicide behavior has also been linked with anxiety disorders (85), further investigation into the risk of suicide behavior among individuals with asthma and anxiety disorders is needed.
Smoking is a particularly problematic health behavior in youth with asthma, leading to higher symptom burden and treatment resistance. DSM-IV anxiety/depressive disorders in a sample of adolescent patients with asthma in one healthcare system have been found to be present in 14.5% of nonsmokers, 19.8% of susceptible nonsmokers and 37.8% of smokers. After controlling for several covariates, youth with comorbid anxiety and depressive disorders and asthma had a two-fold increased likelihood of smoking compared to those without. Youth with asthma who smoked reported significantly more asthma symptoms, reduced functioning due to asthma, less use of controller medication and more use of rescue medications compared to those who did not smoke (86).
Pathophysiology.
The mechanisms underlying the association between asthma and anxiety disorders are not known. It may be that there is a causal link between asthma and anxiety disorders; yet, increasingly, evidence supports the possibility that one or more outside factors, either environmental or genetic, may influence the risk of both (87). One longitudinal study that tracked children from ages 3 through 18 and assessed temperamental and illness factors found that a history of self-reported poor respiratory health at age 15 predicted panic disorder/agoraphobia at ages 18 to 21 compared to participants without a history of respiratory problems (88). Another longitudinal, community-based study followed 591 young adults for 20 years, beginning at age 19, and examined the relationship between asthma and panic disorder (65). A bidirectional relationship was observed in which asthma predicted onset of later panic disorder, and panic disorder was antecedent to active asthma. Childhood anxiety, parental smoking and a family history of allergy have been suggested as possible shared etiologic factors in both asthma (65) and panic disorder (89). Environmental factors including low socioeconomic status, exposure to pollutants, environmental stressors and childhood adversity may predispose youth to both asthma and anxiety and depressive disorders (78). Potential factors that could play a role in causal mechanisms for the relationship between asthma and panic disorder include increased levels of anxiety associated with fear of the next asthma attack, the anxiogenic properties of asthma medications, hyperventilation associated with panic attacks, and poor adherence to asthma treatment in patients with psychiatric diagnoses (65, 78).
Treatment.
Data demonstrating the relationship between asthma and anxiety disorders suggest that psychopharmacological and/or psychosocial interventions might improve asthma control. Yet, there is a remarkable paucity of studies that address this issue. One recently published report from the Cochrane Collaboration reviewed the effectiveness of psychological treatment for adults with asthma (90). A total of 14 randomized, controlled studies of 617 subjects were reviewed. Most studies were small, and methodologies varied widely. However, data pooling suggests future avenues of research. Relaxation therapy reduced the need for rescue bronchodilators in two studies, and CBT improved quality of life in two other studies. Spirometry measures improved following bio-feedback in two studies, but not with relaxation therapy in four studies. Overall, the authors concluded that it is not possible to assess the role of psychotherapeutic interventions in patients with asthma because of the lack of an adequate database (90). Larger, more rigorously controlled trials in patients with comorbid asthma and anxiety, including trials of pharmacotherapy, are needed before the role of mental health interventions in the treatment of asthma can be determined.
CARDIOVASCULAR DISEASE
Epidemiology.
Cardiovascular disease (CVD) has been the leading cause of mortality in the USA for over 100 years, with one in three American adults now dying from one or more types of CVD, accounting for one out of every 2.8 deaths in 2004 and more deaths each year than cancer, chronic lung disease, accidents and diabetes mellitus combined. The estimated total cost of CVD in the USA for the year 2007 was US$431.8 billion (91). Hypertension, diabetes mellitus, hypercholesterolemia, elevated body mass index, unhealthy diet, sedentary lifestyle and smoking are key modifiable risk factors for CVD (91). Chronic stress, depression and anxiety also increase the risk of developing CVD and complicate recovery following acute cardiac events (92). Much attention has been paid to depression as both a risk factor for incident CVD and a predictor of poor outcome in cardiac patients. Depression is strongly associated with increased rates of serious cardiac events, all-cause mortality and cardiac mortality following myocardial infarction (MI), unstable angina and coronary artery bypass surgery (7, 93).
Although it is less well studied than depression, emerging data suggest that anxiety is also an important risk factor for both incidence and progression of CVD. Indeed, one comprehensive literature review concluded that there is considerable covariation between depression, anxiety and anger/hostility as risk factors for CVD (94). Denollet et al. (95) found that anxiety symptoms are core features of post-MI depression and concluded that screening for anxiety may be useful in identifying patients at risk for depression following MI. Studies in several cohorts suggest that the general distress shared across depression, anxiety and anger/hostility is a significant risk factor for incident CVD (96–98). However, additional analyses in one study also showed that anxiety symptoms were associated with increased cardiac risk beyond effects of general distress, suggesting the utility of considering anxiety separately from depression and other psychosocial risk factors (96). Depression and anxiety are also as strongly associated with cardiac symptoms and functional impairment in patients with CVD as are physiological measures of cardiac impairment (i.e., number of vessels with ≥50% occlusion or decreased ejection fraction) (4, 99).
The findings of community-based population studies demonstrate that anxiety symptoms (e.g., worry, tension, feeling restless, difficulty making decisions) and anxiety disorders are associated with increased risk for incident CVD, such as MI, sudden cardiac death, angina pectoris, and hypertension (100–105). A recent overview of the literature summarizing findings from 11 prospective studies examining the association between chronic anxiety and incident CVD reported consistently elevated risk associated with anxiety with relative risks ranging from 1.5 to 8 (106). Especially strong data exist for phobic anxiety (100, 107). One study also recently reported increased risk of developing CVD associated with higher levels of PTSD symptoms (108).
Anxiety disorders are also associated with adverse cardiac outcomes. In a recent study of 3369 generally healthy community-dwelling postmenopausal women, a history of recent panic attacks was associated with both coronary heart disease [HR: 4.20 (1.76–9.99)] and the combined end point of coronary heart disease or stroke [HR: 3.08 (1.60–5.94)] after controlling for multiple potential confounders (109). General measures of anxiety and psychological distress were associated with increased rates of 5-year cardiac-related mortality in patients with MI (110). Anxiety in post-MI patients was associated with adverse cardiac events, cardiovascular death (111–113) and increased rates of cardiac rehospitalization and outpatient visits to cardiologists (113). Interestingly, one study of 318 male survivors of a first MI showed that anxiety (HR: 3.01; P = .019) was more strongly associated with subsequent cardiac events than depression (HR: 2.32; P = .039) or hostility (HR: 1.03; P = .950) (113). Studies on cardiac outcomes in patient populations find a particularly strong effect associated with panic disorder (114, 115). Other work has suggested that the trauma of having an MI may cause PTSD, which then adversely impacts survival (116). For example, PTSD was considered in a small study of post-MI patients and found to be associated with cardiac rehospitalization and poor adherence to aspirin prophylaxis regimens (117).
Pathophysiology.
Rozanski and Kubzansky (118) proposed a number of pathways by which anxiety may influence CVD. Effects of anxiety may accumulate over time leading to cardiovascular damage, setting the stage for atherosclerosis and coronary artery disease (93, 119). Thus, similar to chronic stress and other negative emotions, anxiety may lead to excess activation of the HPA axis and sympathetic nervous system. Increases in sympathetic nervous system activity and release of plasma catecholamines may damage the vascular endothelium and also lead to the release of fatty acids above levels needed for metabolic requirements. Excess HPA activation may lead to increased inflammation (120). Anxiety is also hypothesized to increase cardiovascular reactivity to stress leading to greater strain on the heart as a result of increased resting heart rate, baroreflex dysfunction and variability in ventricular repolarization (111, 114, 118, 121). Moreover, anxiety has been linked to altered cardiovascular autonomic control with studies demonstrating reduced heart rate variability among individuals with high levels of anxiety (122). Taken together, the effects of sympathetic nervous system and HPA axis hyperactivity along with altered sympathovagal control of the heart increase the risk of incident CVD and lower the threshold for cardiac ischemia, arrhythmias and sudden cardiac death (93). Anxiety may also influence CVD indirectly, as anxiety is associated with poor health-related behaviors including smoking and excess alcohol consumption, which in turn increase the risk of CVD (122). Acute effects of anxiety are also possible. There is some evidence to suggest that extreme emotional states, like an acute anxiety episode, may actually trigger an MI (123, 124).
Treatment.
Despite the strong association between depression and CVD, many studies designed to assess the effect of psychosocial interventions or antidepressant medications on depression and CVD outcomes failed to show a significant difference between active treatment and placebo on CVD outcomes (7, 92, 125). Given that many patients have had long-term exposure to depressive symptoms and most interventions occur after disease processes are initiated (126), it may be that these interventions have not been administered during the appropriate etiologic window (107). There are very few studies of anxiety treatment in cardiac patients, although issues of exposure duration and appropriate timeframes for interventions are also likely to be relevant for treating anxiety. In a cohort of patients with PTSD who were recovering from an MI, the combination of trauma-focused CBT and education about treatment adherence resulted in improved PTSD symptoms and adherence to aspirin therapy (127). Fluoxetine treatment in patients with mild depression following their first MI resulted in significant improvements in measures of hostility (128). Case-control studies also suggest that the use of SSRIs may be associated with decreased rates of mortality in patients with depression and CVD (129). Clearly, knowledge about the effects of anxiety treatment on CVD risk and outcome is in its infancy and further studies are needed.
CANCER
Epidemiology.
Cancer is a common and frequently deadly diagnosis despite remarkable advances in the past 40 years. During 2006, 1.4 million new cases were diagnosed in the USA, and more than 560,000 Americans died from cancer. However, continued improvements in the prevention, diagnosis and treatment of cancer are at work to improve survival. The 5-year survival rates for all cancers increased from 50% in the 1970s to 65% between 1995 and 2001, and deaths from colon, rectum, stomach, prostate, breast and lung (men only) cancers are declining. As of 2002, there were 10.1 million Americans who had survived cancer or who were undergoing treatment (130).
Conventional wisdom and clinical experience dictate that cancer is a source of situational anxiety, causing psychological distress, fear, dread and sadness. However, apart from these normative emotional responses, cancer is associated with high rates of anxiety and depressive disorders (Table 2), though the latter have been much more extensively studied. Prevalence rates for anxiety and depressive disorders are generally in the range of 10% to 30%, with rates of various anxiety disorders equivalent to or greater than those of depression in many cases. However, rates vary depending on the type and stage of cancer, treatment regimens, time since diagnosis, gender and methods used to diagnose psychiatric illness. Specific phobias, panic disorder with or without agoraphobia, and GAD are commonly reported anxiety disorders in this population, as are adjustment disorder with anxious mood or depressed/anxious mood and PTSD.
 |
Table 2. Anxiety Disorders Diagnosed Using Structured or Semistructured Interviews or Standardized Self-Report Instruments in Patients With Cancer
Pathophysiology.
Factors that influence distress include endocrine or metabolic changes associated with cancer or its treatment, cancer prognosis, individual coping style and social support systems. Some medications commonly used in the treatment of cancer are associated with symptoms of anxiety (e.g., glucocorticoids) or depression (e.g., interferon, glucocorticoids) (140). Variables independently associated with anxiety disorders in one set of patients with advanced cancer who were receiving palliative care were global health status, emotional/cognitive/social functioning, fatigue, nausea and vomiting (136). In another study of patients with mixed types of cancer, anxiety disorders correlated with female sex and poor social support systems (131). Dahl et al. (137) studied 1408 long-term survivors of testicular cancer and found that anxiety disorders correlated with young age at follow-up, relapse anxiety, psychiatric treatment, peripheral neuropathy, alcohol abuse, economic problems and sexual dysfunction. Anxiety and depression among women with a first recurrence of breast cancer correlated with current toxic chemotherapy treatment (i.e., doxorubicin/cyclophosphamide), history of major depression, and feelings of helplessness or hopelessness (133).
Treatment.
Even though psychiatric illness in the context of cancer can increase somatic symptom burden and impair functioning and quality of life, negatively affect adherence to cancer treatment regimens and result in poor outcomes (131, 137, 139, 141), they should not be considered untreatable. Attention to patients' mental health status is an essential part of cancer treatment. However, anxiety and mood disorders in patients with cancer are often untreated or inadequately treated because of time or training constraints or because oncologists do not ask about psychological distress or endorse its importance. Patients contribute to under-treatment by trivializing symptoms of fear, anxious preoccupation, or helplessness/hopelessness, or because they feel that these symptoms are an expected part of their diagnosis and treatment (142, 143). Many physicians prescribe short-term benzodiazepines to help patients cope with the situational anxiety associated with surgery, chemotherapy or radiation (144). There are relatively few placebo-controlled drug trials in patients with depression and cancer (12, 145–151) and virtually none focusing on anxiety disorders. Nonetheless, the traditional antidepressants [e.g., TCAs, SSRIs, serotonin-norepinephrine reuptake inhibitors (SNRIs)] possess anxiolytic properties, and some studies demonstrated improvement in anxiety symptoms in patients with a primary diagnosis of depression (144, 148). This provides some degree of support for their use in patients with cancer and comorbid anxiety disorders (144, 152).
In contrast, a large body of literature, as summarized in several reviews (153–156), evaluates the use of psychological interventions in patients with cancer. Cognitively based psychotherapy alone or in conjunction with skills training and relaxation therapy has been shown in some controlled trials to improve quality of life, coping skills, symptoms of anxiety, and general distress (141, 156, 157). One rigorously conducted systematic review of 329 intervention trials concluded that extant data are insufficient to support strong recommendations for the use of psychological interventions for anxiety in patients with cancer. Few of these trials examined patients with specific anxiety disorders, such as panic disorder or GAD. The overwhelming number of trials examined patients with adjustment disorders, where placebo response rates are likely very high. However, CBT, therapist-delivered interventions, self-practice techniques, communication/expression training and guided imagery/visualization strategies warrant further study (154). Psychosocial interventions lasting 3 months or longer may be more effective than short-term treatment strategies (156, 157), and the combination of different behavioral treatments may be useful in relieving symptoms of anxiety (155). However, findings of recent studies show that psychological treatments do not actually affect survival time in cancer patients (158, 159).
CHRONIC PAIN
Epidemiology.
Contemporary models describe pain as a complex perceptual experience that is determined by sensory as well as psychological (i.e., cognition, emotion, behavior) and social influences. Pain is an essential adaptive process that enables one to curtail further physical harm and permit recuperation. However, for some persons pain becomes chronic, losing its adaptive qualities. The National Comorbidity Survey Part II estimates that approximately 7% of the general population in the USA has experienced chronic pain in the past 12 months (160), at an annual cost of about US $100 billion (161). However, because rates of chronic pain vary depending on the population, definition of chronicity (e.g., pain lasting ≥3 months vs. ≥6 months) and type of pain studied, rates upwards of 20% to 30% have been reported in recently published community-based population studies (162–165). Chronic pain is associated with disability, physical deconditioning, excessive utilization of healthcare resources and emotional distress (163–166). The spectrum of distress seen in chronic pain includes depression, anger, guilt, social withdrawal, fear and anxiety (160, 167, 168).
Depression is strongly and consistently associated with chronic pain in both clinical and community-based samples (160, 162, 169). Fear and anxiety are also significant contributors to the experience of chronic pain, but until relatively recently the anxiety component of psychiatric morbidity in chronic pain received little attention. Means-Christensen et al. (170) found that primary care patients with somatic pain-related complaints (e.g., headache, stomach pain, muscle pain) had high rates not only of depressive symptoms, but also of anxiety symptoms (notably, panic and GAD symptoms). High rates of anxiety disorders have been observed in patients with different pain syndromes, including chronic spinal pain (11% to 27%) (165, 167), rheumatoid arthritis (25% to 35%) (160, 171), fibromyalgia (60%) (171) and migraine (172). In patients seeking treatment for chronic pain (Table 3), the most prevalent past 12-month anxiety disorders are phobic disorders (9% to 13%), GAD (0% to 13.4%) and panic disorder (2.1% to 7.2%). Particularly high rates of panic disorder and phobias are found in patients with chest pain and negative cardiac workups (178, 179). The most prevalent past 12-month anxiety disorders reported in community samples with chronic pain (Table 3) are specific phobia (12.5% to 15.7%), social anxiety disorder (8.3 to 11.8%) and PTSD (7.3 to 10.7%). These rates are higher than 12-month prevalence rates in the general US population (180). Pooled data from a recent survey of 85,088 community-dwelling adults from 17 countries indicate that persons with back or neck pain are two to three times more likely to have had past 12-month panic disorder/agoraphobia, social anxiety disorder, GAD or PTSD compared to those without (181).
 |
Table 3. Twelve-Month Prevalence of Anxiety Disorders in Persons With Pain in Community and Treatment-Seeking Samplesa
Data from the NCS (160) and the Midlife Development in the United States (MIDUS) survey (173) demonstrated that compared with the general population, rates of depression and anxiety disorders were significantly higher in persons with chronic pain. Somewhat surprisingly, they also found that the association with chronic pain was stronger for anxiety disorders than for depression. For example, among persons with chronic pain in the NCS, the 12-month prevalence of any anxiety disorder was 35.1% compared to 21.7% for any mood disorder (160). When chronic pain in persons with rheumatoid arthritis, migraine or back pain was assessed in MIDUS, the strength of association was consistently larger for panic attacks (OR: 2.09–3.58) and GAD (OR: 2.17–3.86) than for depression (OR: 1.48–2.84) (173).
There is some evidence to suggest that anxiety disorders precede the onset of pain. In a sample of 146 injured workers with chronic musculoskeletal pain, Asmundson et al. (174) found that, in all but one case, the anxiety disorder preceded the pain complaint. Likewise, Kinney et al. (176) found that among 90 patients with chronic low back pain, 23% had a preexisting anxiety disorder. Additional research on temporal sequence and course of anxiety disorders in chronic pain is needed.
Pathophysiology.
Pain and anxiety are both associated with physiological arousal. Bodily changes stemming from arousal (see Sections on IBS and CVD) serve a protective function by promoting escape and withdrawal. However, if prolonged, arousal can have detrimental physical effects. Physical injury and stressful or uncontrollable experiences also initiate other complex neural and hormonal processes (e.g., release of cytokines, β-endorphin, 5-HT-moduline) that, while designed to promote tissue healing and reinstate homeostasis, can be destructive to various body systems (e.g., muscle, bone, neural tissue) when prolonged (182, 183). Illustrating these effects, Sareen et al. (24) found strong associations between anxiety disorders, particularly PTSD, and medical illnesses characterized by pain (e.g., multiple sclerosis, ulcer, hernia, arthritis, rheumatism).
Persons with anxiety sensitivity (i.e., fear of anxiety symptoms based on the belief they may have harmful consequences) or injury/illness sensitivity or who have preexisting anxiety disorders may respond to chronic pain with catastrophic misinterpretation of the meaning of the pain, physiologic arousal, fear of recurrent pain, fear of movement or re-injury, avoidance of pain, and hyper-vigilance (184). Such maladaptive responses may lead to a self-perpetuating cycle that promotes and maintains activity limitations, disability, pain, and additional fear and anxiety (168, 185–187).
Treatment.
There is a relatively large literature suggesting that CBT in patients with chronic pain may improve pain levels, coping skills and functional abilities (188–190). Consideration of chronic pain and anxiety in the context of a cognitive-behavioral fear-avoidance phenomenon has implications for the design of therapeutic interventions. Graded exposure in vivo is one cognitive-behavioral technique that has been shown in single case-controlled (191, 192) and randomized controlled (193) studies to reduce fear and pain intensity and improve physical activity in patients with chronic pain. These treatments are promising for those with co-occurring chronic pain and anxiety disorders, although it remains to be determined what specific effect they will have on the anxiety disorder symptoms. There is also a large literature suggesting that antidepressants have beneficial effects in treating chronic pain, even in patients without comorbid depression. The TCAs and SNRIs appear to be more effective than the SSRIs in treating neuropathic pain (194).
CRITICAL SUMMARY
The studies reviewed here have numerous methodologic limitations. Some epidemiological studies failed to use structured interviews or standardized rating scales, others did not account for medication effects and some used too narrow a sampling frame. Despite these limitations, each of which would presumably weaken any anxiety-medical condition association, the wealth of evidence clearly shows that anxiety is associated with an increased prevalence of these five broad categories of medical conditions. The extant data cannot tell us at this point the magnitude of these associations, nor how this association compares with depression, though the NCS-R data suggest that the association of anxiety with a number of medical illnesses is likely to be comparable to that of depression. Our understanding of pathophysiological substrates accounting for associations with these five medical conditions is largely inferential and mostly based on preclinical data or knowledge of human pathophysiology. Although more specific understanding is limited by the small number of available human studies, neuroimaging studies are providing a useful window into CNS substrates that may mediate links between anxiety and medical illness. Understanding of pathophysiology is much more advanced for the association between anxiety and some medical conditions (e.g., IBS, CVD) and poorly developed for others (e.g., cancer). Treatment studies with either an anxiety or depressive intervention have focused much more on some medical conditions (e.g., CVD, IBS) than on others (e.g., asthma, cancer), and the majority of treatment studies have targeted depression, with few if any treating anxiety. However, for some conditions (e.g., CVD), treatment may have an impact on behavioral and pathophysiological processes, as well as on some clinically important outcomes of the medical condition such as quality of life. Thus, it is not clear whether anxiety treatments can have an impact on the underlying medical condition, and if so, to what degree.
RESEARCH PRIORITIES
Conference participants outlined research needs to advance understanding of anxiety disorders and comorbid medical illness and improve patient care. No attempt was made at the conference to rank order these priorities, but all were felt to be of substantial importance to the field.
EPIDEMIOLOGY
| •. | Include anxiety indicators, especially those fulfilling DSM-IV diagnostic criteria, in large population-based health surveys. | ||||
| •. | Collect data on the economic impact of anxiety disorders in medically ill patients that are important to both the medical/scientific community and policy makers. | ||||
| •. | Evaluate temporal onset in the relationship between anxiety disorders and medical illness by longitudinally following a cohort of children at risk of developing a chronic medical condition, such as asthma, and documenting which comes first. | ||||
| •. | Conduct observational studies to identify the medical or psychiatric comorbidities that are most strongly associated with quality of life (critical new work in this area has recently been published (195)) and medical prognosis. The findings would aid primary care physicians to focus on baseline symptoms that most urgently require attention. | ||||
PATHOPHYSIOLOGY
| •. | Conduct studies that further examine the vicious cycle of central activation-somatization by identifying brain regions, neural circuits and neurotransmitter systems involved in the visceral hyperalgesia, hypervigilance and increased smooth muscle tone associated with anxiety disorders. | ||||
| •. | Examine potential biological mechanisms of the association between anxiety disorders and medical conditions, while also adjusting for and examining the role of potential confounding/mediating factors. | ||||
TREATMENT
| •. | Develop generalized CBT interventions for primary care patients and measure the effect of improving fear, avoidance, somatization and other elements of negative affect on function, clinical outcomes of medical illness, and utilization patterns. | ||||
| •. | Assess the utility of novel delivery methods for broad-based (i.e., targeting anxiety, depressive and related somatic symptoms) CBT, such as telephone- and web-based CBT or stepped collaborative-care approaches to treatment delivery. | ||||
| •. | Study the effectiveness of CBT approaches in the top 10% of healthcare utilizers in a given healthcare system using a collaborative care model. | ||||
| •. | Identify medically ill patients needing treatment by stratifying patients with DSM-IV anxiety disorders according to severity of emotional distress and randomizing each group to evidence-based treatment vs. usual care. | ||||
| •. | Integrate successful components of collaborative care treatment models, such as brief evidence-based CBT combined with pharmacologic interventions in patients with panic disorder (196, 197), to address symptoms of anxiety and depression and improve functional and medical outcomes in primary care patients. | ||||
| •. | Create a demonstration project that measures the clinical and economic outcomes when financial incentives are provided to primary care physicians for screening high utilizers of healthcare resources and using best-practices treatment guidelines. | ||||
CONCLUSIONS
The clinical importance of the bidirectional relationship between psychiatric and physical illness is beginning to be appreciated by the medical, clinical and research communities. Extant studies primarily focus on comorbid depression. However, emerging evidence suggests that anxiety and the anxiety disorders, which have received relatively less attention, may be as important as depression. In addition, many patients have comorbid anxiety and depressive symptoms, which are associated with increased severity of psychiatric illness, additive functional impairment and medical costs. Much like depression, anxiety disorders and subsyndromal anxiety amplify symptoms of some medical illnesses and appear to worsen clinical outcomes. The considerable overlap of anxiety, depression and chronic stress states suggests that clinicians should broaden their search for mental health problems beyond depressive symptoms in their patients with chronic medical illnesses to include symptoms of anxiety.
Increased funding for research programs that address basic science issues, epidemiology, treatment and healthcare delivery systems is needed. Development of effective messages about the role of anxiety and anxiety disorders in common medical illnesses will facilitate educational approaches designed to increase awareness among patients, physicians, healthcare systems and policy makers. Inclusion of data about the role of mental disorders in comorbid medical illnesses into medical school, residency and continuing medical education curricula will improve awareness in the medical community. Primary care physicians who frequently see patients with chronic medical illness are in an excellent position to assess patients' mental state and begin appropriate interventions. However, there is a remarkable lack of data from rigorously designed clinical trials to guide treatment decisions in this population. In addition, stigma about mental health issues can color patients' acceptance of a psychiatric diagnosis. Patients who understand that a medical illness may be the result of a variety of risk factors that include mental health issues and brain function and who are engaged participants in their care are likely to have better clinical outcomes. Although much work remains to be done, the stage has been set to explore the relationship between anxiety disorders and medical illness with the aim of developing and subsequently promoting evidence-based treatment strategies to improve prognosis and quality of life in patients with chronic medical illnesses.
1 Kessler RC, Ormel J, Demler O, Stang PE. Comorbid mental disorders account for the role impairment of commonly occurring chronic physical disorders: results from the National Comorbidity Survey. J Occup Environ Med 2003; 45:1257–66 Crossref, Google Scholar
2 Wang PS, Beck AL, Berglund P, et al. Effects of major depression on moment-in-time work performance. Am J Psychiatry 2004;161:1885–91 Crossref, Google Scholar
3 Evans DL, Charney DS. Mood disorders and medical illness: a major public health problem. Biol Psychiatry 2003;54:178–80 Crossref, Google Scholar
4 Katon W, Lin EH, Kroenke K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen Hosp Psychiatry 2007;29:147–55 Crossref, Google Scholar
5 Stein MB, Cox BJ, Afifi TO, Belik SL, Sareen J. Does co-morbid depressive illness magnify the impact of chronic physical illness? A population-based perspective. Psychol Med 2006;36:587–96 Crossref, Google Scholar
6 de Jonge P, Roy JF, Saz P, Marcos G, Lobo A, for the ZARADEMP investigators. Prevalent and incident depression in community-dwelling elderly persons with diabetes mellitus: results from the ZARADEMP project. Diabetologia 2006;49:2627–33 Crossref, Google Scholar
7 Frasure-Smith N, Lespérance F. Recent evidence linking coronary heart disease and depression. Can J Psychiatry 2006;51:730–7 Crossref, Google Scholar
8 Judd F, Komiti A, Chua P, Mijch A, Hoy J, Grech P, et al. Nature of depression in patients with HIV/AIDS. Aust N Z J Psychiatry 2005;39:826–32 Crossref, Google Scholar
9 Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol Psychiatry 2003;54:216–26 Crossref, Google Scholar
10 Lin EH, Katon W, Von Korff M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care 2004;27:2154–60 Crossref, Google Scholar
11 Lustman PJ, Clouse RE, Nix BD, et al. Sertraline for prevention of depression recurrence in diabetes mellitus: a randomized, double-blind, placebo-controlled trial. Arch Gen Psychiatry 2006;63:521–9 Crossref, Google Scholar
12 Musselman DL, Somerset WI, Guo Y, et al. A double-blind, multicenter, parallel-group study of paroxetine, desipramine, or placebo in breast cancer patients (stages I, II, III, and IV) with major depression. J Clin Psychiatry 2006;67:288–96 Crossref, Google Scholar
13 Rabkin JG, McElhiney MC, Rabkin R, et al. Placebo-controlled trial of dehydroepiandrosterone (DHEA) for treatment of nonmajor depression in patients with HIV/AIDS. Am J Psychiatry 2006;163: 59–66 Crossref, Google Scholar
14 Taylor CB, Youngblood ME, Catellier D, et al, for the ENRICHD Investigators. Effects of antidepressant medication on morbidity and mortality in depressed patients after myocardial infarction. Arch Gen Psychiatry 2005;62:792–8 Crossref, Google Scholar
15 Katon WJ, Walker EA. Medically unexplained symptoms in primary care. J Clin Psychiatry 1998;59(Suppl 20):15–21 Google Scholar
16 Marciniak MD, Lage MJ, Dunayevich E, Russell JM, Bowman L, Landbloom RP, et al. The cost of treating anxiety: the medical and demographic correlates that impact total medical costs. Depress Anxiety 2005;21:178–84 Crossref, Google Scholar
17 McLaughlin TP, Khandker RK, Kruzikas DT, Tummala R. Overlap of anxiety and depression in a managed care population: prevalence and association with resource utilization. J Clin Psychiatry 2006;67: 1187–93 Crossref, Google Scholar
18 Simon GE, VonKorff M. Somatization and psychiatric disorder in the NIMH Epidemiologic Catchment Area study. Am J Psychiatry 1991;148:1494–500 Crossref, Google Scholar
19 Walker EA, Katon W, Russo J, Ciechanowski P, Newman E, Wagner AW. Health care costs associated with posttraumatic stress disorder symptoms in women. Arch Gen Psychiatry 2003;60: 369–74 Crossref, Google Scholar
20 Harter MC, Conway KP, Merikangas KR. Associations between anxiety disorders and physical illness. Eur Arch Psychiatry Clin Neurosci 2003;253:313–20 Crossref, Google Scholar
21 Sareen J, Jacobi F, Cox BJ, Belik SL, Clara I, Stein MB. Disability and poor quality of life associated with comorbid anxiety disorders and physical conditions. Arch Intern Med 2006;166:2109–16 Crossref, Google Scholar
22 Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med 2007;146:317–25 Crossref, Google Scholar
23 Ludman E, Katon W, Russo J, et al. Panic episodes among patients with diabetes. Gen Hosp Psychiatry 2006;28:475–81 Crossref, Google Scholar
24 Sareen J, Cox BJ, Clara I, Asmundson GJ. The relationship between anxiety disorders and physical disorders in the U.S. National Comorbidity Survey. Depress Anxiety 2005;21:193–202 Crossref, Google Scholar
25 Stein MB, Roy-Byrne PP, Craske MG, Bystritsky A, Sullivan G, Pyne JM, et al. Functional impact and health utility of anxiety disorders in primary care outpatients. Med Care 2005;43:1164–70 Crossref, Google Scholar
26 Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology 2006;130:1480–91 Crossref, Google Scholar
27 Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology 2006;130:1377–90 Crossref, Google Scholar
28 Grundy D, Al-Chaer ED, Aziz Q, et al. Fundamentals of neurogastroenterology: basic science. Gastroenterology 2006;130: 1391–411 Crossref, Google Scholar
29 Jarcho JM, Mayer EA. Stress and irritable bowel syndrome. Prim Psychiatry 2007;14:74–8 Google Scholar
30 Blanchard EB, Keefer L, Lackner JM, Galovski TE, Krasner S, Sykes MA. The role of childhood abuse in Axis I and Axis II psychiatric disorders and medical disorders of unknown origin among irritable bowel syndrome patients. J Psychosom Res 2004;56:431–6 Crossref, Google Scholar
31 Drossman DA, Camilleri M, Mayer EA, Whitehead WE. AGA technical review on irritable bowel syndrome. Gastroenterology 2002;123:2108–31 Crossref, Google Scholar
32 Whitehead WE, Palsson O, Jones KR. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: what are the causes and implications? Gastroenterology 2002;122: 1140–56 Crossref, Google Scholar
33 Walker EA, Gelfand AN, Gelfand MD, Katon WJ. Psychiatric diagnoses, sexual and physical victimization, and disability in patients with irritable bowel syndrome or inflammatory bowel disease. Psychol Med 1995;25:1259–67 Crossref, Google Scholar
34 Hazlett-Stevens H, Craske MG, Mayer EA, Chang L, Naliboff BD. Prevalence of irritable bowel syndrome among university students: the roles of worry, neuroticism, anxiety sensitivity and visceral anxiety. J Psychosom Res 2003;55:501–5 Crossref, Google Scholar
35 Lydiard RB, Irritable bowel syndrome, anxiety, and depression: what are the links? J Clin Psychiatry 2001;62(Suppl 8):38–45 [discussion 46–7] Google Scholar
36 Lydiard RB, Falsetti SA. Experience with anxiety and depression treatment studies: implications for designing irritable bowel syndrome clinical trials. Am J Med 1999;107(Suppl 5A):65S–73S Google Scholar
37 Lydiard RB, Greenwald S, Weissman MM, Johnson J, Drossman DA, Ballenger JC. Panic disorder and gastrointestinal symptoms: findings from the NIMH Epidemiologic Catchment Area project. Am J Psychiatry 1994;151:64–70 Crossref, Google Scholar
38 Lydiard RB. Increased prevalence of functional gastrointestinal disorders in panic disorder: clinical and theoretical implications. CNS Spectr 2005;10:899–908 Crossref, Google Scholar
39 Sykes MA, Blanchard EB, Lackner J, Keefer L, Krasner S. Psychopathology in irritable bowel syndrome: support for a psychophysiological model. J Behav Med 2003;26:361–72 Crossref, Google Scholar
40 Irwin C, Falsetti SA, Lydiard RB, Ballenger JC, Brock CD, Brener W. Comorbidity of posttraumatic stress disorder and irritable bowel syndrome. J Clin Psychiatry 1996;57:576–8 Crossref, Google Scholar
41 Drossman DA, Leserman J, Nachman G, et al. Sexual and physical abuse in women with functional or organic gastrointestinal disorders. Ann Intern Med 1990;113:828–33 Crossref, Google Scholar
42 Walker EA, Katon WJ, Roy-Byme PP, Jemelka RP, Russo J. Histories of sexual victimization in patients with irritable bowel syndrome or inflammatory bowel disease. Am J Psychiatry 1993;150:1502–6 Crossref, Google Scholar
43 Creed F, Ratcliffe J, Fernandes L, et al, for the North of England IBS Research Group. Outcome in severe irritable bowel syndrome with and without accompanying depressive, panic and neurasthenic disorders. Br J Psychiatry 2005;186:507–15 Crossref, Google Scholar
44 Bennett EJ, Tennant CC, Piesse C, Badcock CA, Kellow JE. Level of chronic life stress predicts clinical outcome in irritable bowel syndrome. Gut 1998;43:256–61 Crossref, Google Scholar
45 Chang L. Neuroendocrine and neuroimmune markers in IBS: pathophysiological role or epiphenomenon? Gastroenterology 2006;130:596–600 Crossref, Google Scholar
46 Taché Y, Martinez V, Wang L, Million M. CRF1 receptor signaling pathways are involved in stress-related alterations of colonic function and viscerosensitivity: implications for irritable bowel syndrome. Br J Pharmacol 2004;141:1321–30 Crossref, Google Scholar
47 Mayer EA, Naliboff BD, Chang L, Coutínho SV. Stress and irritable bowel syndrome. Am J Physiol Gastrointest Liver Physiol 2001;280: G519–24Crossref, Google Scholar
48 Posserud I, Agerforz P, Ekman R, Bjornsson ES, Abrahamsson H, Simren M. Altered visceral perceptual and neuroendocrine response in patients with irritable bowel syndrome during mental stress. Gut 2004;53:1102–8 Crossref, Google Scholar
49 Dinan TG, Quigley EM, Ahmed SM, et al. Hypothalamic-pituitarygut axis dysregulation in irritable bowel syndrome: plasma cytokines as a potential biomarker? Gastroenterology 2006;130:304–11 Crossref, Google Scholar
50 Raison CL, Miller AH. When not enough is too much: the role of insufficient glucocorticoid signaling in the pathophysiology of stress-related disorders. Am J Psychiatry 2003;160:1554–65 Crossref, Google Scholar
51 Narita K, Murata T, Takahashi T, Kosaka H, Omata N, Wada Y. Plasma levels of adiponectin and tumor necrosis factor-alpha in patients with remitted major depression receiving long-term maintenance antidepressant therapy. Prog Neuropsychopharmacol Biol Psychiatry 2006;30:1159–62 Crossref, Google Scholar
52 Koh KB, Lee Y. Reduced anxiety level by therapeutic interventions and cell-mediated immunity in panic disorder patients. Psychother Psychosom 2004;73:286–92 Crossref, Google Scholar
53 Drossman DA. Brain imaging and its implications for studying centrally targeted treatments in irritable bowel syndrome: a primer for gastroenterologists. Gut 2005;54:569–73 Crossref, Google Scholar
54 Levy RL, Olden KW, Naliboff BD, et al. Psychosocial aspects of the functional gastrointestinal disorders. Gastroenterology 2006;130:1447–58 Crossref, Google Scholar
55 Drossman DA, Toner BB, Whitehead WE, et al. Cognitive-behavioral therapy versus education and desipramine versus placebo for moderate to severe functional bowel disorders. Gastroenterology 2003;125:19–31 Crossref, Google Scholar
56 Lackner JM, Morley S, Dowzer C, Mesmer C, Hamilton S. Psychological treatments for irritable bowel syndrome: a systematic review and meta-analysis. J Consult Clin Psychology 2004;72: 1100–13 Crossref, Google Scholar
57 Creed F, Fernandes L, Guthrie E, et al, for the North of England IBS Research Group. The cost-effectiveness of psychotherapy and paroxetine for severe irritable bowel syndrome. Gastroenterology 2003;124:303–17 Crossref, Google Scholar
58 Lydiard RB. Psychopharmacology in the treatment of irritable bowel syndrome. Primary Psychiatry 2007;14:40–9 Google Scholar
59 Tollefson GD, Luxenberg M, Valentine R, Dunsmore G, Tollefson SL. An open label trial of alprazolam in comorbid irritable bowel syndrome and generalized anxiety disorder. J Clin Psychiatry 1991;52:502–8 Google Scholar
60 American Lung Association. Trends in asthma morbidity and mortality. American Lung Association Epidemiology & Statistics Unit Research and Program Services. Available at: http://www.lungusa.org/atf/cf/%7B7A8D42C2-FCCA-4604-8ADE-7F5D5E762256%7D/ASTHMA06FINAL.PDF 2006 Accessed November 30, 2006Google Scholar
61 Goodwin RD, Eaton WW. Asthma and the risk of panic attacks among adults in the community. Psychol Med 2003;33:879–85 Crossref, Google Scholar
62 Goodwin RD, Pine DS. Respiratory disease and panic attacks among adults in the United States. Chest 2002;122:645–50 Crossref, Google Scholar
63 Goodwin RD, Olfson M, Shea S, et al. Asthma and mental disorders in primary care. Gen Hosp Psychiatry 2003;25:479–83 Crossref, Google Scholar
64 Goodwin RD, Jacobi F, Thefeld W. Mental disorders and asthma in the community. Arch Gen Psychiatry 2003;60:1125–30 Crossref, Google Scholar
65 Hasler G, Gergen PJ, Kleinbbaum DG, et al. Asthma and panic in young adults. A 20-year prospective community study. Am J Respir Crit Care Med 2005;171:1224–30Crossref, Google Scholar
66 Ortega AN, Huertas SE, Canino G, Ramirez R, Rubio-Stipec M. Childhood asthma, chronic illness, and psychiatric disorders. J Nerv Ment Dis 2002;190:275–81 Crossref, Google Scholar
67 Goldney RD, Ruffin R, Fisher LJ, Wilson DH. Asthma symptoms associated with depression and lower quality of life: a population survey. Med J Aust 2003;178:437–41 Crossref, Google Scholar
68 Goodwin RD, Fergusson DM, Horwood LJ. Asthma and depressive and anxiety disorders among young persons in the community. Psychol Med 2004;34:1465–74 Crossref, Google Scholar
69 Ortega AN, McQuaid EL, Canino G, Goodwin RD, Fritz GK. Comorbidity of asthma and anxiety and depression in Puerto Rican children. Psychosomatics 2004;45:93–9 Crossref, Google Scholar
70 Katon W, Lozano P, Russo J, McCauley E, Richardson L, Bush T. The prevalence of DSM-IV anxiety and depressive disorders in youth with asthma compared to controls. J Adol Health 2007;41:455–63 Crossref, Google Scholar
71 Bussing R, Burket RC, Kelleher ET. Prevalence of anxiety disorders in a clinic-based sample of pediatric asthma patients. Psychosomatics 1996;37:108–15 Crossref, Google Scholar
72 Vila G, Nollet-Clemencon C, Vera M, et al. Prevalence of DSM-IV disorders in children and adolescents with asthma versus diabetes. Can J Psychiatry 1999;44:562–9 Crossref, Google Scholar
73 Kean EM, Kelsay K, Wamboldt F, Wamboldt MZ. Posttraumatic stress in adolescents with asthma and their parents. J Am Acad Child Adolesc Psychiatry 2006;45:78–86 Crossref, Google Scholar
74 Nascimento I, Nardi AE, Valença AM, et al. Psychiatric disorders in asthmatic outpatients. Psychiatry Res 2002;110:73–80Crossref, Google Scholar
75 Lavoie KL, Bacon SL, Barone S, et al. What is worse for asthma control and quality of life: depressive disorders, anxiety disorders, or both? Chest 2006;130:1039–47 Crossref, Google Scholar
76 Feldman JM, Siddique MI, Morales E, Kaminski B, Lu SE, Lehrer PM. Psychiatric disorders and asthma outcomes among high-risk inner-city patients. Psychosom Med 2005;67:989–96 Crossref, Google Scholar
77 Valença AM, Falcao R, Freire RC, et al. The relationship between the severity of asthma and comorbidites with anxiety and depressive disorders. Rev Bras Psiquiatr 2006;28:206–8Crossref, Google Scholar
78 Katon WJ, Richardson L, Lozano P, McCauley E. The relationship of asthma and anxiety disorders. Psychosom Med 2004;66: 349–55 Google Scholar
79 Goodwin RD, Fisher M, Goldberg J. A twin study of post-traumatic stress disorder symptoms and asthma. Am J Respir Crit Care Med 2007 published ahead of print on August 16, 2007 as doi:10.1164/rccm.200610–1467OC Google Scholar
80 Richardson LP, Lozano P, Russo J, McCauley E, Bush T, Katon W. Asthma symptom burden: relationship to asthma severity and anxiety and depression symptoms. Pediatrics 2006;118:1042–51 Crossref, Google Scholar
81 Lavoie KL, Cartier A, Labrecque M, et al. Are psychiatric disorders associated with worse asthma control and quality of life in asthma patients? Respir Med 2005;99:1249–57 Crossref, Google Scholar
82 McCauley E, Katon W, Russo J, Richardson L, Lozano P. Impact of anxiety and depression on functional impairment in adolescents with asthma. Gen Hosp Psychiatry 2007;29:214–22 Crossref, Google Scholar
83 Katon WJ, Richardson L, Russo J, Lozano P, McCauley E. Quality of mental health care for youth with asthma and comorbid anxiety and depression. Med Care 2006;44:1064–72 Crossref, Google Scholar
84 Goodwin RD, Eaton WW. Asthma, suicidal ideation, and suicide attempts: findings from the Baltimore Epidemiologic Catchment Area follow-up. Am J Public Health 2005;95:717–22 Crossref, Google Scholar
85 Boden JM, Fergusson DM, Horwood LJ. Anxiety disorders and suicidal behaviours in adolescence and young adulthood: findings from a longitudinal study. Psychol Med 2007;37:431–40 Crossref, Google Scholar
86 Bush T, Katon W, Russo J, Lozano P, McCauley E, Oliver M. Anxiety and depressive disorders are associated with smoking in adolescents with asthma. J Adolescent Health 2007;40:425–32 Crossref, Google Scholar
87 Goodwin RD, Lewinsohn PM, Seeley JR. Cigarette smoking and panic attacks among young adults in the community: the role of parental smoking and anxiety disorders. Biol Psychiatry 2005;58: 686–93 Crossref, Google Scholar
88 Craske MG, Poulton R, Tsao JC, Plotkin D. Paths to panic disorder/agoraphobia: an exploratory analysis from age 3 to 21 in an unselected birth cohort. J Am Acad Child Adolesc Psychiatry 2001; 40:556–63Crossref, Google Scholar
89 Goodwin RD, Messineo K, Bregante A, Hoven CW, Kairam R. Prevalence of probable mental disorders among pediatric asthma patients in an inner-city clinic. J Asthma 2005;42:643–7 Crossref, Google Scholar
90 Yorke J, Fleming SL, Shuldham CM. Psychological interventions for adults with asthma. Cochrane Database Syst Rev 2006(1):CD002982 Google Scholar
91 Rosamond W, Flegal K, Friday G, et al, for the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2007;115:e69–e171 Crossref, Google Scholar
92 Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice. The emerging field of behavioral cardiology. J Am Coll Cardiol 2005;45:637–51 Crossref, Google Scholar
93 Carney RM, Freedland KE, Veith RC. Depression, the autonomic nervous system, and coronary heart disease. Psychosom Med 2005;67 (suppl 1):S29–33 Crossref, Google Scholar
94 Suls J, Bunde J, Anger, anxiety, and depression as risk factors for cardiovascular disease: the problems and implications of overlapping affective dispositions. Psychol Bull 2005;131:260–300 Crossref, Google Scholar
95 Denollet J, Strik JJ, Lousberg R, Honig A. Recognizing increased risk of depressive comorbidity after myocardial infarction: looking for 4 symptoms of anxiety-depression. Psychother Psychosom 2006;75: 346–52Crossref, Google Scholar
96 Kubzansky LD, Cole SR, Kawachi I, Vokonas P, Sparrow D. Shared and unique contributions of anger, anxiety, and depression to coronary heart disease: a prospective study in the normative aging study. Ann Behav Med 2006;31:21–9 Crossref, Google Scholar
97 Boyle SH, Michalek JE, Suarez EC. Covariation of psychological attributes and incident coronary heart disease in U.S. Air Force veterans of the Vietnam war. Psychosom Med 2006;68:844–50 Crossref, Google Scholar
98 Todaro JF, Shen BJ, Niaura R, Spiro III A, Ward KD. Effect of negative emotions on frequency of coronary heart disease (the Normative Aging Study). Am J Cardiol 2003;92:901–6 Crossref, Google Scholar
99 Sullivan MD, LaCroix AZ, Spertus JA, Hecht J. Five-year prospective study of the effects of anxiety and depression in patients with coronary artery disease. Am J Cardiol 2000;86:1135–8 Crossref, Google Scholar
100 Albert CM, Chae CU, Rexrode KM, Manson JE, Kawachi I. Phobic anxiety and risk of coronary heart disease and sudden cardiac death among women. Circulation 2005;111:480–7 Crossref, Google Scholar
101 Eaker ED, Pinsky J, Castelli WP. Myocardial infarction and coronary death among women: psychosocial predictors from a 20-year follow-up of women in the Framingham Study. Am J Epidemiol 1992;135: 854–64Crossref, Google Scholar
102 Jonas BS, Franks P, Ingram DD. Are symptoms of anxiety and depression risk factors for hypertension? Longitudinal evidence from the National Health and Nutrition Examination Survey I Epidemiologic Follow-up study. Arch Fam Med 1997;6:43–9 Crossref, Google Scholar
103 Kawachi I, Sparrow D, Vokonas PS, Weiss ST. Symptoms of anxiety and risk of coronary heart disease. The Normative Aging Study. Circulation 1994;90:2225–9 Crossref, Google Scholar
104 Kubzansky LD, Kawachi I, Spiro III A, Weiss ST, Vokonas PS, Sparrow D. Is worrying bad for your heart? A prospective study of worry and coronary heart disease in the Normative Aging Study. Circulation 1997;95:818–24 Crossref, Google Scholar
105 Nicholson A, Fuhrer R, Marmot M. Psychological distress as a predictor of CHD events in men: the effect of persistence and components of risk. Psychosom Med 2005;67:522–30 Crossref, Google Scholar
106 Kubzansky LD, Davidson KW, Rozanski A. The clinical impact of negative psychological states: expanding the spectrum of risk for coronary artery disease. Psychosom Med 2005;67(Suppl 1):S10–4 Crossref, Google Scholar
107 Kubzansky LD. Sick at heart: the pathophysiology of negative emotions. Cleve Clin J Med 2007;74(suppl 1):S67–72 Crossref, Google Scholar
108 Kubzansky LD, Koenen KC. Is post-traumatic stress disorder related to development of heart disease? Future Cardiol 2007;3:153–6 Crossref, Google Scholar
109 Smoller JW, Pollack MH, Wassertheil-Smoller S, et al. Panic attacks and risks of incident cardiovascular events among postmenopausal women in the Women's Health Initiative Observational Study. Arch Gen Psychiatry 2007;64:1153–60 Crossref, Google Scholar
110 Frasure-Smith N, Lespérance F. Depression and other psychological risks following myocardial infarction. Arch Gen Psychiatry 2003;60: 627–36Crossref, Google Scholar
111 Carpeggiani C, Emdin M, Bonaguidi F, et al. Personality traits and heart rate variability predict long-term cardiac mortality after myocardial infarction. Eur Heart J 2005;26:1612–7 Crossref, Google Scholar
112 Frasure-Smith N, Lespérance F, Talajic M. The impact of negative emotions on prognosis following myocardial infarction: is it more than depression? Health Psychol 1995;14:388–98 Crossref, Google Scholar
113 Strik JJMH, Denollet J, Lousberg R, Honig A. Comparing symptoms of depression and anxiety as predictors of cardiac events and increased health care consumption after myocardial infarction. J Am Coll Cardiol 2003;42:1801–7 Crossref, Google Scholar
114 Fleet R, Lespérance F, Arsenault A, et al. Myocardial perfusion study of panic attacks in patients with coronary artery disease. Am J Cardiol 2005;96:1064–8Crossref, Google Scholar
115 Sullivan GM, Kent JM, Kleber M, Martinez JM, Yeragani VK, Gorman JM. Effects of hyperventilation on heart rate and QT variability in panic disorder pre- and post-treatment. Psychiatry Res 2004;125:29–39 Crossref, Google Scholar
116 Shemesh E, Rudnick A, Kaluski E, et al. A prospective study of posttraumatic stress symptoms and nonadherence in survivors of a myocardial infarction (MI). Gen Hosp Psychiatry 2001;23:215–22 Crossref, Google Scholar
117 Shemesh E, Yehuda R, Milo O, et al. Posttraumatic stress, nonadherence, and adverse outcome in survivors of a myocardial infarction. Psychosom Med 2004;66:521–6 Crossref, Google Scholar
118 Rozanski A, Kubzansky LD. Psychologic functioning and physical health: a paradigm of flexibility. Psychosom Med 2005;67(Suppl 1):S47–53 Crossref, Google Scholar
119 Schneiderman N. Psychophysiologic factors in atherogenesis and coronary artery disease. Circulation 1987;76(1 Pt 2):141–7 Google Scholar
120 Pitsavos C, Panagiotakos DB, Papagcorgiou C, Tsetsekou E, Soldatos C, Stefanadis C. Anxiety in relation to inflammation and coagulation markers, among healthy adults: the ATTICA study. Atherosclerosis 2006;185:320–6 Crossref, Google Scholar
121 Sheps DS, Rozanski A. From feeling blue to clinical depression: exploring the pathogenicity of depressive symptoms and their management in cardiac practice. Psychosom Med 2005;67 (Suppl 1):S2–5 Crossref, Google Scholar
122 Kubzansky LD, Kawachi I, Weiss ST, Sparrow D. Anxiety and coronary heart disease: a synthesis of epidemiological, psychological, and experimental evidence. Ann Behav Med 1998;20:47–58 Crossref, Google Scholar
123 Mittleman MA, Maclure M, Sherwood JB, et al. Triggering of acute myocardial infarction onset by episodes of anger. Determinants of Myocardial Infarction Onset study investigators. Circulation 1995;92:1720–5 Crossref, Google Scholar
124 Wittstein IS, Thiemann DR, Lima JA, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med 2005;352:539–48 Crossref, Google Scholar
125 Sheps DS, Freedland KE, Golden RN, McMahon RP. ENRICHD and SADHART: implications for future biobehavioral intervention efforts. Psychosom Med 2003;65:1–4 Crossref, Google Scholar
126 Glassman AH, Bigger JT, Gaffney M, Shapiro PA, Swenson JR. Onset of major depression associated with acute coronary syndromes: relationship of onset, major depressive disorder history, and episode severity to sertraline benefit. Arch Gen Psychiatry 2006;63:283–8 Crossref, Google Scholar
127 Shemesh E, Koren-Michowitz M, Yehuda R, et al. Symptoms of posttraumatic stress disorder in patients who have had a myocardial infarction. Psychosomatics 2006;47:231–9 Crossref, Google Scholar
128 Strik JJMH, Honig A, Lousberg R, et al. Efficacy and safety of fluoxetine in the treatment of patients with major depression after first myocardial infarction: findings from a double-blind, placebo-controlled trial. Psychosom Med 2000;62:783–9 Crossref, Google Scholar
129 Glassman AH, Bigger JT. Antidepressants in coronary heart disease: SSRIs reduce depression, but do they save lives? JAMA 2007;297:411–2 Crossref, Google Scholar
130 American Cancer Society. Cancer Facts and Figures, 2006. Atlanta (Ga): American Cancer Society; 2006. Available at: http://www.cancer.org/downloads/STT/CAFF2006PWSecured.pdf. Accessed December 13, 2006Google Scholar
131 Stark D, Kiely M, Smith A, Velikova G, House A, Selby P. Anxiety disorders in cancer patients: their nature, associations, and relation to quality of life. J Clin Oncol 2002;20:3137–48 Crossref, Google Scholar
132 Härter M, Reuter K, Aschenbrenner A, et al. Psychiatric disorders and associated factors in cancer: results of an interview study with patients in inpatient, rehabilitation and outpatient treatment. Eur J Cancer 2001;37:1385–93Crossref, Google Scholar
133 Okamura M, Yamawaki S, Akechi T, Taniguchi K, Uchitomi Y. Psychiatric disorders following first breast cancer recurrence: prevalence, associated factors and relationship to quality of life. Jpn J Clin Oncol 2005;35:302–9 Crossref, Google Scholar
134 Kissane DW, Grabsch B, Love A, Clarke DM, Bloch S, Smith GC. Psychiatric disorder in women with early stage and advanced breast cancer: a comparative analysis. Aust N Z J Psychiatry 2004;38:320–6 Crossref, Google Scholar
135 Kangas M, Henry JL, Bryant RA. The course of psychological disorders in the 1st year after cancer diagnosis. J Consult Clin Psychol 2005;73:763–8Crossref, Google Scholar
136 Smith EM, Gomm SA, Dickens CM. Assessing the independent contribution to quality of life from anxiety and depression in patients with advanced cancer. Palliat Med 2003;17:509–13 Crossref, Google Scholar
137 Dahl AA, Haaland CF, Mykletun A, et al. Study of anxiety disorder and depression in long-term survivors of testicular cancer. J Clin Oncol 2005;23:2389–95 Crossref, Google Scholar
138 Roth A, Nelson CJ, Rosenfeld B, et al. Assessing anxiety in men with prostate cancer: further data on the reliability and validity of the Memorial Anxiety Scale for Prostate Cancer (MAX-PC). Psychosomatics 2006;47:340–7 Crossref, Google Scholar
139 Tagay S, Herpertz S, Langkafel M, et al. Health-related quality of life, anxiety and depression in thyroid cancer patients under short-term hypothyroidism and TSH-suppressive levothyroxine treatment. Eur J Endocrinol 2005;153:755–63 Crossref, Google Scholar
140 Raison CL, Miller AH. Depression in cancer: mechanisms and disease progression. Biol Psychiatry 2003;54:283–94 Crossref, Google Scholar
141 Andersen BL. Biobehavioral outcomes following psychological interventions for cancer patients. J Consult Clin Psychol 2002;70:590–610 Crossref, Google Scholar
142 Ballenger JC, Davidson JRT, Lecrubier Y, Nutt DJ. Consensus statement on depression, anxiety, and oncology. J Clin Psychiatry 2001;62(suppl8):64–7 Google Scholar
143 Ronson A. Psychiatric disorders in oncology: recent therapeutic advances and new conceptual frameworks. Curr Opin Oncol 2004;16:318–23 Crossref, Google Scholar
144 Berard RMF. Depression and anxiety in oncology: the psychiatrist's perspective. J Clin Psychiatry 2001;62(suppl 8):58–61 Crossref, Google Scholar
145 Costa D, Mogos I, Toma T. Efficacy and safety of mianserin in the treatment of depression of women with cancer. Acta Psychiatr Scand Suppl 1985;320:85–92 Crossref, Google Scholar
146 Fisch MJ, Loehrer PJ, Kristeller J, et al, for the Hoosier Oncology Group. Fluoxetine versus placebo in advanced cancer outpatients: a double-blinded trial of the Hoosier Oncology Group. J Clin Oncol 2003;21:1937–43 Crossref, Google Scholar
147 Holland JC, Romano SJ, Heiligenstein JH, Tepner RG, Wilson MG. A controlled trial of fluoxetine and desipramine in depressed women with advanced cancer. Psychooncology 1998;7:291–300 Crossref, Google Scholar
148 Morrow GR, Hickok JT, Roscoe JA, et al. Differential effects of paroxetine on fatigue and depression: a randomized, double-blind trial from the University of Rochester Cancer Center Community Clinical Oncology Program. J Clin Oncol 2003;21:4635–41 Crossref, Google Scholar
149 Pezzella G, Moslinger-Gehmayr R, Contu A. Treatment of depression in patients with breast cancer: a comparison between paroxetine and amitriptyline. Breast Cancer Res Treat 2001;70:1–10 Crossref, Google Scholar
150 Razavi D, Allilaire JF, Smith M, et al. The effect of fluoxetine on anxiety and depression symptoms in cancer patients. Acta Psychiatr Scand 1996;94:205–10 Crossref, Google Scholar
151 van Heeringen K, Zivkov M. Pharmacological treatment of depression in cancer patients. A placebo-controlled study of mianserin. Br J Psychiatry 1996;169:440–3 Crossref, Google Scholar
152 Pasquini M, Biondi M, Costantini A, et al. Detection and treatment of depressive and anxiety disorders among cancer patients: feasibility and preliminary findings from a liaison service in an oncology division. Depress Anxiety 2006;23:441–8 Crossref, Google Scholar
153 Fawzy FI. Psychosocial interventions for patients with cancer: what works and what doesn't. Eur J Cancer 1999;35:1559–64 Crossref, Google Scholar
154 Newell SA, Sanson-Fisher RW, Savolainen NJ. Systematic review of psychological therapies for cancer patients: overview and recommendations for future research. J Natl Cancer Inst 2002;94:558–84 Crossref, Google Scholar
155 Redd WH, Montgomery GH, DuHamel KN. Behavioral intervention for cancer treatment side effects. J Natl Cancer Inst 2001;93: 810–23 Crossref, Google Scholar
156 Rehse B, Pukrop R. Effects of psychosocial interventions on quality of life in adult cancer patients: meta analysis of 37 published controlled outcome studies. Patient Educ Couns 2003;50:179–86Crossref, Google Scholar
157 Antoni MH, Wimberly SR, Lechner SC, et al. Reduction of cancerspecific thought intrusions and anxiety symptoms with a stress management intervention among women undergoing treatment for breast cancer. Am J Psychiatry 2006;163:1791–7 Crossref, Google Scholar
158 Coyne JC, Pajak TF, Harris J, et al. Emotional well-being does not predict survival in head and neck cancer patients: a radiation therapy oncology group study. Cancer 2007;110:2568–75 Crossref, Google Scholar
159 Spiegel D, Butler LD, Giese-Davis J, et al. Effects of supportive-expressive group therapy on survival of patients with metastatic breast cancer: a randomized prospective trial. Cancer 2007;110: 1130–8 Crossref, Google Scholar
160 McWilliams LA, Cox BJ, Enns MW. Mood and anxiety disorders associated with chronic pain: an examination in a nationally representative sample. Pain 2003;106:127–33 Crossref, Google Scholar
161 Weisberg JN, Vaillancourt PD. Personality factors and disorders in chronic pain. Semin Clin Neuropsychiatry 1999;4:155–66 Google Scholar
162 Arnow BA, Hunkeler EM, Blasey CM, et al. Comorbid depression, chronic pain, and disability in primary care. Psychosom Med 2006;68:262–8 Crossref, Google Scholar
163 Blyth FM, March LM, Cousins MJ. Chronic pain-related disability and use of analgesia and health services in a Sydney community. Med J Aust 2003;179:84–7 Crossref, Google Scholar
164 Blyth FM, March LM, Brnabic AJ, Jorm LR, Williamson M, Cousins MJ. Chronic pain in Australia: a prevalence study. Pain 2001;89:127–34 Crossref, Google Scholar
165 Von Korff M, Crane P, Lane M, et al. Chronic spinal pain and physical-mental comorbidity in the United States: results from the national comorbidity survey replication. Pain 2005;113: 331–9 Crossref, Google Scholar
166 Stang PE, Brandenburg NA, Lane MC, Merikangas KR, Von Korff MR, Kessler RC. Mental and physical comorbid conditions and days in role among persons with arthritis. Psychosom Med 2006;68:152–8 Crossref, Google Scholar
167 Dersh J, Gatchel RJ, Mayer T, Polatin P, Temple OR. Prevalence of psychiatric disorders in patients with chronic disabling occupational spinal disorders. Spine 2006;31:1156–62 Crossref, Google Scholar
168 Dersh J, Polatin PB, Gatchel RJ. Chronic pain and psychopathology: research findings and theoretical considerations. Psychosom Med 2002;64:773–86 Google Scholar
169 Patten SB, Williams JVA, Wang JL. Mental disorders in a population sample with musculoskeletal disorders. BMC Muscoloskelet Disord 2006;7:37, doi:10.1186/1471-2474-7-37Crossref, Google Scholar
170 Means-Christensen AJ, Roy-Byrne PP, Sherbourne CD, Craske MG, Stein MB. Relationships among pain, anxiety, and depression in primary care. Depress Anxiety, 2007, Oct 11 [Epub ahead of print]Google Scholar
171 Arnold LM, Hudson JI, Keck PE, Auchenbach MB, Javaras KN, Hess EV. Comorbidity of fibromyalgia and psychiatric disorders. J Clin Psychiatry 2006;67:1219–25 Crossref, Google Scholar
172 Stewart WF, Linet MS, Celentano DD. Migraine headaches and panic attacks. Psychosom Med 1989;51:559–69 Crossref, Google Scholar
173 McWilliams LA, Goodwin RD, Cox BJ. Depression and anxiety associated with three pain conditions: results from a nationally representative sample. Pain 2004;111:77–83 Crossref, Google Scholar
174 Asmundson GJ, Jacobson SJ, Allerdings MD, Norton GR. Social phobia in disabled workers with chronic musculoskeletal pain. Behav Res Ther 1996;34:939–43 Crossref, Google Scholar
175 Polatin PB, Kinney RK, Gatchel RJ, Lillo E, Mayer TG. Psychiatric illness and chronic low back pain. The mind and the spine—which goes first? Spine 1993;66–71 Google Scholar
176 Kinney RK, Gatchel RJ, Polatin PB, Fogarty WT, Mayer TG. Prevalence of psychopathology in acute and low back pain patients. J Occup Rehab 1993;3:95–103 Crossref, Google Scholar
177 Atkinson JH, Slater MA, Patterson TL, Grant I, Garfin SR. Prevalence, onset, and risk of psychiatric disorders in men with chronic low back pain: a controlled study. Pain 1991;45:111–21 Crossref, Google Scholar
178 Beitman BD, Mukerji V, Lamberti JW, et al. Panic disorder in patients with chest pain and angiographically normal coronary arteries. Am J Cardiol 1989;63:1399–403 Crossref, Google Scholar
179 Katon W, Hall ML, Russo J, et al. Chest pain: relationship of psychiatric illness to coronary arteriographic results. Am J Med 1988;84:1–9 Crossref, Google Scholar
180 Kessler RC, Chiu WT, Demler O, Merikangas KR, Walter EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005;62:617–27Crossref, Google Scholar
181 Demyttenaere K, Bruffaerts R, Lee S, et al. Mental disorders among persons with chronic back or neck pain: results from the World Mental Health Surveys. Pain 2007;129:332–42 Crossref, Google Scholar
182 Kiecolt-Glaser JK, McGuire L, Robies TF, Glaser R. Emotions, morbidity, and mortality: new perspectives from psychoneuroimmunology. Annu Rev Psychol 2002;53:83–107 Crossref, Google Scholar
183 McEwen BS. Protective and damaging effects of stress mediators, N Engl J Med 1998;338:171–9 Crossref, Google Scholar
184 Asmundson GJ, Norton PJ, Norton GR. Beyond pain: the role of fear and avoidance in chronicity. Clin Psychol Rev 1999;19:97–119 Crossref, Google Scholar
185 Norton PJ, Asmundson GJ. Amending the fear-avoidance models of chronic pain: what is the role of physiological arousal? Behav Ther 2003;34:17–30 Crossref, Google Scholar
186 Sieben JM, Portegijs PJ, Vlaeyen JW, Knottnerus JA. Pain-related fear at the start of a new low back pain episode. Eur J Pain 2005;9:635–41 Crossref, Google Scholar
187 Vancleef LM, Peters ML, Roelofs J, Asmundson GJ. Do fundamental fears differentially contribute to pain-related fear and pain catastrophizing? An evaluation of the sensitivity index. Eur J Pain 2006;10:527–36 Crossref, Google Scholar
188 Devine EC. Meta-analysis of the effect of psychoeducational interventions on pain in adults with cancer. Oncol Nurs Forum 2003;30:75–89 Crossref, Google Scholar
189 Hoffman BM, Papas RK, Chatkoff DK, Kerns RD. Meta-analysis of psychological interventions for chronic low back pain. Health Psychol 2007;26:1–9 Crossref, Google Scholar
190 Morley S, Eccleston C, Williams A. Systematic review and meta-analysis of randomized controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headache. Pain 1999;80:1–13 Crossref, Google Scholar
191 de Jong JR, Vlaeyen JW, Onghena P, Cuypers C, den Hollander M, Ruijgrok J. Reduction of pain-related fear in complex regional pain syndrome type 1: the application of graded exposure in vivo. Pain 2005;116:264–75Crossref, Google Scholar
192 de Jong JR, Vlaeyen JW, Onghena P, Goossens ME, Geilen M, Mulder H. Fear of movement/(re)injury in chronic low back pain: education or exposure in vivo as mediator to fear reduction? Clin J Pain 2005;21:9–17 Crossref, Google Scholar
193 Woods M, Asmundson GJG. Evaluating the efficacy of graded in vivo exposure for the treatment of fear in patients with chronic back pain: a randomized controlled clinical trial. Pain 2007, Aug 2 [Epub ahead of print]Google Scholar
194 Saarto T, Wiffen PJ. Antidepressants for neuropathic pain. Cochrane Database Syst Rev 2005;CD005454 Google Scholar
195 Merikangas KR, Ames M, Cui L, et al. The impact of co-morbidity of mental and physical conditions on role disability in the US adult household population. Arch Gen Psychiatry 2007;64:1180–8 Crossref, Google Scholar
196 Rollman BL, Belnap BH, Mazumdar S, et al. A randomized trial to improve the quality of treatment for panic and generalized anxiety disorders in primary care. Arch Gen Psychiatry 2005;62:1332–41 Crossref, Google Scholar
197 Roy-Byrne PP, Craske MG, Stein MB, et al. A randomized effectiveness trial of cognitive-behavioral therapy and medication for primary care panic disorder. Arch Gen Psychiatry 2005;62:290–8 Crossref, Google Scholar