Mental Illness in Hispanics: A Review of the Literature
Abstract
Although Hispanics are the largest minority in the United States, we have only fragmentary information and scarce guidelines on the frequency, recognition, and treatment of mental illness in this population. In reviewing the literature on this issue, the authors found that Hispanics are younger, poorer, and less educated than the average American; have an average unemployment rate; are heterogeneous in aspects such as race/genetics, health care access/utilization, acculturation, and legal status; differ in risk of some mental illnesses and in risky behaviors according to birthplace/acculturation; are at increasing risk of behaviors and health issues that complicate mental illness and its treatment, such as obesity, diabetes, and sedentary lifestyle; have less access to health and mental health care and receive less care and lower-quality care; tend to receive mental health care in primary care settings, often face linguistic barriers, and are more likely not to have mental disorders detected; seem less likely to suffer from depression and anxiety but tend to have more persistent mental illnesses; are more likely to somatize distress and to report psychotic symptoms in the absence of a formal thought disorder; do not appear to differ from Caucasians in drug metabolism and pharmacokinetics; seem to have lower medication adherence, which could be a function of socioeconomic and linguistic or educational factors; seem to respond well to adapted psychotherapeutic and psychosocial interventions and receive significant additional benefit from supplemental services such as case management, collaborative care, and quality improvement interventions.
According to the 2000 census, Hispanics in the United States numbered 35.2 million, or 12.5% of the population (1). As of July 2004, their number was estimated at 41.3 million, the largest minority group in the country (2). Currently Hispanics account for one-half of the national population growth, and by 2050 they are expected to number 102.6 million, or 24.4% of the U.S. population (3).
In the United States, the terms “Hispanic” and “Latino” reflect a cultural identity based on language and geographical provenance; they are not racial definitions, and in fact they include people from several races. This identification seems to be strong and perdurable. According to the 2002 National Survey of Latinos (4), the proportion of Hispanics who defined themselves as Latino or Hispanic was 85% for the first generation, 77% for the second, and 72% for the third and later.
Despite these impressive numbers and the accepted validity of Hispanic as a distinct demographic and cultural category, we have only fragmentary evidence and scarce guidelines on the treatment of mentally ill Hispanic Americans. In this review, our goal is to present a comprehensive, synthetic overview of the research published in the United States that is relevant to the mental health and treatment of Hispanic Americans. We do not include studies of Hispanics in other countries, because the frequency, presentation, and treatment response of mental disorders are significantly influenced by environmental factors. Our review includes reports published from 1959 through November 2005.
General characteristics of Hispanic Americans
Compared with the overall population, Hispanics are younger, poorer, and less educated; they are more likely to be foreign born and to live with family; and they are less likely to speak English and to have health insurance. Their employment rate is close to the average U.S. rate (Table 1). Hispanics make up over 80% of the undocumented U.S. population, with an estimated 8.4 million in 2004 (5).
Heterogeneity of Hispanic Americans in aspects relevant to mental health
Despite a common ethnic identification, Hispanics are heterogeneous in some aspects that may influence the incidence, presentation, course, and treatment of mental illness, such as birthplace and acculturation, genetics and race, health care access and utilization, and language. For example, a recently published study found differences in alcohol, marijuana, and cocaine use among Hispanic students according to ethnic subgroup, language first spoken, parental education, urbanicity, and region (7).
The question of whether this heterogeneity detracts from the validity of studies on Hispanics does not have a simple answer. In many cases the report specifies which Hispanic population or subgroup was studied, or this information can be inferred from the location of the study. Other studies address subjects that traverse all or several of the Hispanic subgroups, such as monolingualism versus bilingualism, generational differences, or disadvantaged socioeconomic status. We simply want to emphasize that the generalizability of study results must be judged on a case-by-case basis.
Differences in genetics and race
Hispanic Americans include groups that are predominantly Native American, black or white, plus an admixture of all possible combinations. Table 2 presents estimates of the genetic pool of Mexican, Puerto Rican, and Cuban subgroups in the United States. Figures similar to those for the overall Mexican American population were reported for the Mexican American population of the San Luis Valley in Colorado (63% European, 34% Native American, and 3% African) (8). This genetic heterogeneity probably contributes to pharmacological differences among Hispanic subgroups, such as the different bronchodilator responses to albuterol between Puerto Ricans and Mexican Americans (9).
Differences according to birthplace
Two out of five (40.2%) Hispanic Americans are foreign-born (1). This is an important consideration, because birthplace (U.S. born vs. foreign born) and acculturation seem to influence health and behavior as well as the risk of mental illness among Hispanic Americans (11). Recent studies have consistently shown lower rates of diagnosable disorders among immigrant than among U.S.-born Hispanics of several major subgroups, such as Mexicans and Cubans (12–14). Data from a large survey, the Mexican American Prevalence and Services Survey, indicated that total rates for DSM-III-R anxiety, mood, and substance disorders were 50% lower for immigrants than for the U.S. born (15). Similar differences have been reported for psychotic symptoms and illicit drug use (16–19). In a recent study, differences for mood, anxiety, and substance use disorders were observed not only for foreign-born Latinos but also for foreign-born non-Hispanic whites (20). However, studies of some specific groups, for example the elderly, have shown the opposite trend, toward higher levels of psychopathology in immigrants. Data from the Sacramento Area Latino Study on Aging showed a higher prevalence of depression among immigrants, bicultural Latinos, and less acculturated Latinos compared with U.S.-born and more acculturated groups (21). Probably the levels of acculturative stress change the direction of the effect for some Hispanic populations. A study of Mexican immigrants found that acculturative stress is a risk factor for depression and suicidal ideation, whereas social support and agreement with the decision to migrate are protective factors (22). For comparison, in a study of Latin American refugees in Sweden, the strongest independent risk mediator for mental illness was ethnicity, with Latinos having an odds ratio of 4.11, compared with age-, sex- , and education-matched Swedish controls (23).
Access to, quality, and utilization of health care and mental health care
Hispanics are more likely to be uninsured, and even when insured, they have less access to medical care than other Americans. For example, in 2002, 35% of Hispanics reported being uninsured (vs. 14% of whites and 21% of African Americans) (4). Worse, the number of insured Hispanics, especially privately insured, seems to be diminishing faster than in other groups (Table 3).
In the 2004 National Healthcare Disparities Report, Hispanics scored lower than non-Hispanic whites on about 90% of access measures (25). The recent National Comorbidity Survey Replication showed that, for Hispanics, the 12-month odds ratio of receiving treatment for mental disorders was 0.6 (95% CI, 0.5–0.8; p<0.05) compared with non-Hispanic whites (26). Even insured Hispanics seem to use services less. A recent study at the Department of Veterans Affairs (VA) found that the odds ratio of having a health visit in the previous year was 0.4 for Hispanics, compared with 2.2 for non-Hispanic whites (27). Besides this disadvantaged position for Hispanics as a whole, significant differences may exist in health care access among Hispanic subgroups, with a negative effect on Mexicans and Central Americans in particular (Table 4). Undocumented and/or immigrant Hispanics also have less access and use services less (28, 29).
Because Hispanics are younger overall than other ethnic groups, any issue affecting them has a disproportionate impact on the young. More than a quarter (25.7%) of Hispanic children lack health insurance, with Mexican children faring the worst (30.4%), followed by Central and South Americans (23.8%), other Hispanics (18.6%), Puerto Ricans (11.4%), and Cubans (9.3%), compared with 7.8% for non-Hispanic whites (31).
Different types of studies have shown that the quality of health care received by Hispanics is below average. Depressed Hispanics seem to be less likely than Caucasians to receive a prescription for an antidepressant, to actually take the medication, and to receive specialty care (32–35). Some studies suggest that, compared with Caucasians, Hispanics with psychosis are less likely to receive medication or to receive an atypical antipsychotic, more likely to receive a depot antipsychotic, and less likely to have appropriate trials of antipsychotic medications (36–39). The 2004 National Healthcare Disparities Report (25) indicated that Hispanics received a poorer quality of care than non-Hispanic whites on about 40% of quality measures. The reasons for this disparity seem to be complex. For example, Hispanic Medicare beneficiaries have an odds ratio of 0.36 for receiving hip replacement surgery compared with non-Hispanics (40). Given that the procedure is fully covered by Medicare, this finding suggests that underutilization of health services by Hispanics cannot be attributed solely to lack of health insurance. In a recent study of an insured adult population at the VA, researchers found a trend toward greater inequality in the delivery of outpatient mental health care for Hispanics (41). These racial/ethnic differences in the treatment of mental illness have persisted under Medicare managed care (42).
The underutilization of mental health care by Hispanics, especially but not exclusively by Mexican Americans, has been noted for decades (43–46). This underutilization was recently demonstrated for Hispanics with schizophrenia or schizoaffective disorder who were receiving services in the public sector in San Diego: 19% of Latinos received case management services, compared with 30% of Caucasians and 17% of African Americans (47). Ethnic differences in utilization are not a simple issue. As shown in a study using data from the National Comorbidity Survey (NCS), to understand ethnic or racial disparities in specialty care, the effects of ethnicity or race should be analyzed in combination with variables related to socioeconomic status and environmental context (48).
Hispanics are significantly more likely to receive attention for mental disorders in primary care settings than in specialized settings, which is probably related to their underutilization of mental health care. Mexican Americans with mental disorders were found to have a 12-month utilization rate of 18.4% for general care providers and 8.8% for mental health specialists (49).
Among factors that complicate the issue of reduced access to mental health care for Hispanics, two are worth mentioning specifically: 1) knowing where to find a provider increases significantly the likelihood of using specialty mental health care (50); and 2) Latinos are more likely than Caucasians to perceive the health care system as unfair because of race or ethnicity (4, 51).
Behaviors and risk factors that complicate mental illness and its treatment
Among Hispanics, the risk of health factors that can complicate mental disorders or their treatment, such as obesity, diabetes mellitus, and lack of exercise, is growing rapidly. For some risky behaviors, such as use of alcohol, tobacco, and illegal drugs, Hispanics seem to be at lower risk than Caucasians (Table 5). Yet, again, differences exist in alcohol-related problems among Hispanic subgroups, with Mexican Americans demonstrating more problems than Cuban or Puerto Rican Americans. Furthermore, Hispanics seem to be at higher risk of some alcohol-related problems, such as driving under the influence, male-to-female partner violence, and alcohol-related mortality (cirrhosis) (52, 53).
Like the risk of mental illness, these health risk factors seem to increase with acculturation and time since entering the United States. An analysis using data from the National Longitudinal Study of Adolescent Health (57) suggested that the acculturation of overweight-related behaviors, such as diet, smoking, and inactivity, is rapid; moreover, longer residence in the United States was associated with increased weight gain among Puerto Ricans and Cubans.
However, other studies show differences between Hispanic subgroups in this regard. For example, poorer health was associated with higher socioeconomic status and acculturation among Mexicans but with lower socioeconomic status and acculturation among Latinos from the Caribbean Islands (58).
Family, environment, and mental illness
As noted earlier, Hispanics are more likely to live with family (1). They also seem to be more likely to engage in closed networks, as opposed to the open networks of most Americans of Caucasian origin. This may have both beneficial and adverse effects. Closed networks appear to provide more emotional support to their members; however, they may eventually pose barriers to problem solving because of the lack of bridges to outside networks (59).
A recently published study comparing Mexican and Anglo American patients with schizophrenia and their families (60) found that “family warmth” seemed to work in opposite ways in the two ethnic groups—as a protective factor for the Mexican patients and as a risk factor for the Anglo American patients. In another study (61), researchers found that greater self-reported family cohesion appeared to have a protective effect against emotional distress for Latino and African American relatives of patients with schizophrenia, but not for Caucasian American relatives. Researchers in California found that Mexican American patients and relatives reported lower rates of expressed emotion than Caucasians. High expressed emotion predicted relapse for Caucasians but not for Mexican Americans (62).
Linguistic barriers and communication with health care providers
About half of adult Hispanics report having low English proficiency. According to the 2000 census, about 80% of Hispanics age 5 years and older speak Spanish at home, and half of those harbor doubts about their proficiency in English (63). According to the 2002 National Survey of Latinos, 47% of adult Hispanics are Spanish dominant, 28% are bilingual, and 25% are English dominant (4). A significant number of Hispanics report difficulty communicating with doctors and other health care providers (4) (Table 6). This is worrisome, as poor English fluency in itself is a risk factor for less use of health care and mental health care services among Hispanics (64) (Table 7). Hispanic children whose parents had low English proficiency had triple the odds for fair or poor health status (65).
A significant number of Hispanics also have inadequate health literacy, even in Spanish, and have mistaken beliefs about mental illness. In a four-city study, rates of inadequate health literacy in Spanish among Spanish seniors ranged from 21.2% to 60% (66). A study of beliefs about the cause of mental illness among the elderly found that Hispanics were less likely than Caucasians or African Americans to endorse biopsychosocial causes of depression, and this lower endorsement predicted lower use of mental health services (67). Poor health literacy also seems to be higher among Hispanics with low English proficiency (68).
Moreover, once Hispanic patients access services, poor English proficiency is a risk factor for lower quality of care, delayed services, poorer follow-up, longer hospital stay, higher resource utilization, lower adherence to psychotropic medications, and patient dissatisfaction with provider and treatment (70–80). The authors of a study in Connecticut concluded that culturally sensitive clinics are not enough to address the difficulties monolingual Hispanics have in managing medications, which may be due to the persistent effects of the language barrier and low education levels (81).
Prevalence of mental disorders among Hispanic Americans
There is some debate on the frequency of the most common mental disorders, especially depression, in Hispanics (82), but the larger studies show lower caseness rates for Hispanics as a whole and for Mexican and Cuban Americans than for non-Latinos. A study using data from the National Health and Nutrition Examination Survey III (83) found that the prevalence of major depression was higher in Caucasians than African and Hispanic Americans; the opposite pattern was found for dysthymic disorder. The National Comorbidity Survey Replication (84) showed lower odds ratios for Hispanics compared with non-Hispanic whites for anxiety, mood, impulse control, and substance use disorders as well as for any disorder. Recently a large survey, the National Epidemiologic Survey on Alcoholism and Related Conditions (NESARC) (85), found 12-month prevalences of major depressive disorder of 4.27% for Hispanics, compared with 5.53% for Caucasians and 4.52% for African Americans. In the Hispanic Health and Nutrition Examination Survey 1982–1984 (14), however, Puerto Ricans had a significantly higher frequency of depression than Mexican and Cuban Americans. In a recent pooled analysis of the National Surveys on Drug Use and Health, 2001–2003 (86), similar findings were noted for Hispanics and Puerto Ricans. However, according to the Youth Risk Behavior Survey of the Centers for Disease Control and Prevention, in 1999, Latino youths were significantly more likely than young African and European Americans to have attempted suicide, made a suicide plan, or seriously considered suicide (87). Finally, some disadvantaged Hispanic subpopulations seem to be at higher risk of mental illness—for example, the elderly, illegal aliens, and segregated or impoverished sectors (88–91).
However, even if Hispanics do have a lower risk of mental disorders, they seem to have more persistent disorders (92, 93). This finding seems logical, given the less favorable environment for Hispanics, their lower rates of access to and utilization of mental health care, and the lower quality of the care they receive.
We have no reliable data on the frequency among Hispanics of mental disorders that are difficult to detect in the usual surveys, such as bipolar disorder and schizophrenia (94). For bipolar disorder, an analysis of the NESARC data found that the lifetime odds ratio of DSM-IV bipolar I disorder was 0.6 for Hispanics compared with Caucasians (95). Half a century ago, Malzberg (96, 97) found that the rate of first admissions to mental hospitals, especially for dementia praecox, for Puerto Ricans in New York State largely exceeded their proportion in the population. At the same time, Jaco (98), in Texas, found lower rates of psychiatric admissions for Mexican Americans than for white and black Americans. Similar data were reported in California (99–100). In Puerto Rico, the figures from the Epidemiologic Catchment Area (ECA) study are in line with national data, and data from the Los Angeles ECA study show no statistical differences between Mexican Americans and non-Hispanic whites (101–103). However, the methodology of this ECA study is highly suspect (104). The question of the prevalence of schizophrenia among Hispanic Americans is of further interest because studies in countries with national registries consistently reveal a higher incidence of schizophrenia in disadvantaged immigrant populations (105). A recent meta-analysis concluded that a history of migration is an important risk factor for schizophrenia, suggesting a role for psychosocial adversity in the etiology of the disease (106).
Studies of dementia suggest that its frequency is significantly higher among Hispanics than Caucasians and that Hispanics are at higher risk of developing both Alzheimer’s disease and vascular dementia (107–110).
Detection of mental disorders in Hispanic Americans
Hispanics seem to be at higher risk of not having mental health problems detected in primary care settings (111). In a study with 496 Mexican Americans, primary care providers noted depression in 21% of the patients who were found to have depressive disorders in a systematic evaluation (112). In a pediatric clinic, only 24% of Hispanic mothers with depression were correctly identified as depressed, compared with 31% of black mothers and 38% of other mothers (113). A study of elderly Medicare beneficiaries found that those in the “Hispanic or other” ethnic groups had an odds ratio of 0.72 for diagnosed depression compared with Caucasians (114). Several studies have suggested that rates of recognition and treatment of attention deficit hyperactivity disorder are lower in Hispanic children (115–118). This underrecognition seems to be influenced by not only clinician factors but also patient and environmental factors. Hispanic adolescents are less likely than Caucasians to have their mental health problems reported by caregivers (119). A study in California found high levels of maternal depressive symptoms among low-income Hispanic women, but only half of these women identified themselves as needing help with depression (120).
Diagnosis of mental disorders in Hispanic Americans
In the literature on the diagnosis of mental disorders in Hispanic Americans, we have mainly retrospective or small studies scattered over several decades, with conflicting results. The way Hispanics with mental illness are perceived seems to differ from the way Caucasians are perceived and seems to fluctuate over time. For example, from the 1960s to the early 1980s, studies consistently reported a tendency for higher disorganization and impairment among Hispanic than among nonminority patients with schizophrenia (121–125). However, studies from the 1980s to date report either no difference or a tendency for the nonminority group to be more symptomatic (126–134).
Some studies suggest that Hispanics are more likely than Caucasians to receive a diagnosis of a psychotic disorder and less likely to receive one of a mood disorder. In the 1980s, a review of the records of 76 patients with bipolar disorder showed that Hispanic (Puerto Rican) and black patients were more likely than whites to be misdiagnosed as having schizophrenia, particularly if they were young and had auditory hallucinations (135). A 7-year longitudinal study (136) of 936 inpatients in Texas who had at least four hospitalizations found that 44% of Hispanics who were initially diagnosed as having schizophrenia received a change in diagnosis during the study period, double the rate for Caucasians and African Americans. A study of a national sample of elderly inpatient veterans (137) found that African Americans and Hispanics were more likely than Caucasians to have a diagnosis of a psychotic disorder. However, a retrospective study in New Jersey examining new admissions in a large behavioral health system found that Hispanics, in contrast to African Americans, were not more likely than Caucasians to receive a diagnosis of schizophrenia, although they were disproportionately diagnosed as having major depression, despite higher levels of psychotic symptoms by self-report (138). A study using the Structured Clinical Interview for DSM-IV found that half of Hispanic adolescents diagnosed as having major depressive disorder met the criteria for bipolar disorder (139). A high frequency of psychotic symptoms in the absence of formal psychosis and associated especially with depression has been reported in Hispanic Americans. At a general medicine practice in New York City, psychotic symptoms were more commonly observed in depressed Hispanics than in depressed non-Hispanics (140). A study in Rhode Island found that Hispanics with major depression were more likely to report psychotic symptoms (141). A study in Boston found that 46% of outpatient Caribbean Latinos reported having hallucinations, but only 9% of them were diagnosed as having a thought disorder (142). A retrospective study of applicants for state benefits (143) found that Hispanics were more likely to endorse hallucinations but not to receive a diagnosis of psychosis.
A tendency for Hispanics to somatize distress has been repeatedly reported in Latin America, although the methodology of the studies has been criticized (144). A U.S. study using a personality inventory in claims for workers’ compensation (145) found that Hispanics were more likely than Caucasians to somatize. In a study in California (146), depressed Latinas and African American women scored significantly higher than Caucasians on somatization. A recent study of anxiety and fears (147) found that parents of Mexican children in Mexico and Hispanic American children in the United States reported more worry and physiological symptoms for their children than Caucasian parents.
Effect of language on diagnosis of mental disorders
Some studies and case reports have addressed the influence of language on psychiatric diagnosis and assessment in Hispanics, but the issue remains unsettled. A study in New York published in 1973 (148, 149) showed that Hispanics with schizophrenia were deemed sicker when interviewed in English. The authors posed three hypotheses: 1) the differences were due to raters’ prejudices; 2) the patients underwent change when they spoke English, probably because of the tension, and “gave up;” and 3) the English raters’ frame of reference was not applicable to the Spanish-American patients. A 1970 report from New Jersey (150) described several cases of foreign-born forensic patients, mostly Hispanic, who showed psychotic symptoms in interviews in their native language but not in English. A study published in 1981 comparing separately recorded Spanish- and English-language interviews (151) found that subjects expressed more symptoms during the Spanish interview. In a more recent New York study (152), symptom severity among Hispanic patients with schizophrenia and depression was rated highest in bilingual interviews, followed by those in Spanish, and lowest in those in English. Hispanic clinicians rated symptom severity higher than did Anglo clinicians.
Medication treatment of mentally ill Hispanic Americans
Metabolism/pharmacokinetics of psychotropic medications
Little information is available on the metabolism of medications in Hispanics. However, the evidence generated so far does not support the notion of different dosing guidelines for this ethnic group. Several relevant studies on the cytochrome P450 system have been published. For P450 enzyme 2D6 (CYP 2D6), perhaps the most important one in psychopharmacology, the initial study by Lam et al. (153), the larger one by Mendoza et al. (154), and the recent one by Casner (155), all of them with Mexican American subjects, found low proportions of slow metabolizers (4.5%, 3.2%, and 6%, respectively), with frequencies similar to that of Caucasians. As for the CYP 3A4 genotype, Paris et al. (156) found that the frequency of the active (AA) variant in Caucasian and Hispanic males (93% and 80%, respectively) was intermediate between those of Asian (100% AA) and African American males (19% AA). In the methylene-tetrahydrofolate reductase gene, the frequency of two single-nucleotide polymorphisms was high and was comparable between Puerto Rican Hispanics and Caucasians (157). A study on gut metabolism via CYP 3A4 or transport by P-glycoprotein, using cyclosporine, showed that the mean bioavailability in Hispanics (42.1%) was comparable in Caucasians (39.6%) and significantly higher than in African Americans (30.9%) (158). The genotypes for the aldehyde-dehydrogenases ADH2 and ALDH2 in Mexican Americans were found not to be different from those of Caucasians, although a higher frequency of the mutant CYP 2E1 was noted among Mexican Americans, which may have a role in the growing rate of alcoholic liver disease in this population (159). In contrast, however, Poland et al. (160) report no difference between Mexican and European Americans for CYP 2E1 and 3A activity.
Lam et al. (161) measured steady-state haloperidol and reduced haloperidol concentrations in 250 patients with schizophrenia from four ethnic groups (African, Caucasian, and Mexican in the United States, and Chinese in Taiwan). They found a statistically significant difference in the proportion of patients with low ratios of reduced haloperidol to haloperidol concentration between the Chinese and the other three groups but not among the non-Chinese groups.
Response to psychotropic medications
Large studies sponsored by pharmaceutical companies include too few minority subjects. A review (162) of the studies submitted to the FDA for the 185 new molecular entities approved between Jan. 1, 1995, and Dec. 31, 1999, showed that when race could be determined from the records, 88% of the participants were white, 8% African American, 3% Hispanic, and 1% or less each of other minorities. Even worse, it showed that the participation of minorities in clinical trials was decreasing. When comparisons were made by year, the participation of African Americans, the minority with the largest share, decreased from 12% in 1995 to 6% in 1999.
The large ongoing treatment studies sponsored by the National Institute of Mental Health have addressed this problem with variable success. In the Clinical Antipsychotic Trials of Intervention Effectiveness, the proportion of Hispanics is about 12% (163). In the Systematic Treatment Enhancement Program for Bipolar Disorder, it is only 3.5% (164).
In a pooled analysis of 104 double-blind placebo-controlled trials of paroxetine for depressive and anxiety disorders, Hispanics appear to have a lower response rate to medication and a higher response rate to placebo (165).
Medication treatment of depression
We found only one randomized placebo-controlled (166) study and four open-label studies (167–170) on the efficacy of pharmacological treatment of depression in Hispanic Americans. The randomized study included 118 subjects, 17 of them Hispanics, of which only three were completers (two responders). With these low figures, it is impossible to draw any conclusions.
Medication treatment of schizophrenia
We found only one prospective study of the efficacy of antipsychotic treatment in Hispanic Americans (171). This small open-label study of risperidone found that Hispanic patients (n=10) showed a faster response and more adverse events than non-Hispanic patients (n=8).
Retrospective studies report that Hispanics seem to receive antipsychotic doses similar to (172, 173) or lower than (174–177) those Caucasians receive. These findings contrast with the repeated finding that African Americans seem to receive higher antipsychotic doses than Caucasians.
As for risk factors and adverse effects of antipsychotics, Hispanic patients with schizophrenia have been shown to have a significantly higher prevalence of metabolic syndrome (71% vs. 41% for non-Hispanics), with differences among Hispanic subgroups (70% in Cuban Americans vs. 88% in other Hispanic subgroups) (178).
Medication adherence
Some studies show that Hispanics are significantly less adherent than Caucasians to antipsychotic and antidepressant medications (179, 180). However, the perceived differences in medication adherence in Hispanic Americans are likely better explained by socioeconomic and communication (i.e., monolingualism) factors by than cultural factors. Thus, a study in Texas reviewing the records of Hispanic outpatients with schizophrenia (181) found rates of compliance in line with those for patients with schizophrenia of other ethnic backgrounds. The authors found support from the family to be a reliable predictor of adherence. A study in which community-based patients in Ohio were interviewed (182) found that although medication adherence was lower for depressed Latinos than for depressed Caucasians, the figures were similar for patients with schizophrenia of both ethnic groups, which may reflect the higher degree of support that schizophrenics receive. A Connecticut study in which an electronic cap to monitor bottle openings was used with a convenience sample of patients with various diagnoses, including schizophrenia, reported a significantly lower rate of medication adherence in monolingual Hispanics than in Caucasians (183).
Psychotherapy and psychosocial interventions
A recent publication reviewed various psychosocial interventions for ethnic minorities (184). Here we focus on those with the most evidence of clinical efficacy.
Psychotherapy for depression
Studies of cognitive behavior therapy and interpersonal psychotherapy with women and adolescents in Puerto Rico show efficacy comparable to that found for other ethnic groups (185, 186).
In the continental United States, we found five studies:
| • | A randomized controlled trial using interpersonal psychotherapy, cognitive behavior therapy, supportive psychotherapy, or supportive psychotherapy plus imipramine therapy in depressed HIV-positive patients of Caucasian, African, Hispanic, and Asian American ethnicities (187) | ||||
| • | A randomized trial using cognitive behavior therapy alone or with clinical case management for low-income depressed outpatients of Caucasian, African, Hispanic, Asian, and Native American ethnicities (188) | ||||
| • | A randomized controlled trial comparing medication, psychotherapy intervention, and referral to community mental health services for low-income African American, Caucasian, and foreign-born Latina women (189) | ||||
| • | A study of quality improvement interventions for depressed Caucasian, African American, and Latina women (190, 191) | ||||
| • | A randomized trial comparing collaborative care and treatment as usual for depressed elderly patients from different ethnic groups (192) | ||||
In general, the results of these studies do not suggest an association between Hispanic ethnicity and outcome of psychotherapy treatment. However, Hispanic or Spanish-speaking participants seem more likely to improve when they receive supplemental case management, collaborative care, or quality improvement interventions as opposed to treatment as usual.
Psychotherapy for anxiety/phobic disorders in children
Two randomized clinical trials of cognitive behavior therapy for children with anxiety/phobic disorders showed similar positive responses and gain maintenance for Hispanic and Caucasian children and no moderating role for ethnicity in the outcome (193–195).
Psychosocial interventions in patients with schizophrenia
Hispanics seem to benefit at least as much as other groups from adapted psychosocial rehabilitation and training. The outcome of psychotherapeutic interventions, like behavioral family management, however, may be more unpredictable:
| • | A randomized study of behavioral family management compared with standard case management for 42 low-income Spanish-speaking patients found that sociocultural factors affect the response to intervention, with behavioral family management increasing the risk of exacerbation of symptoms in the less acculturated patients (196). | ||||
| • | Pooled data from two studies of community-based psychosocial rehabilitation with 226 people who had a schizophrenia spectrum disorder, including Latinos (n=37, 16%), Caucasians, and African Americans, showed similar evolution over time and comparable outcomes for the three groups (197). | ||||
| • | A 3-month intervention study of skills training with two modules, medication management, and symptom management with 92 Latino patients and their designated relatives showed favorable outcomes at 6 months in key domains of psychopathology, relapse, rehospitalization, and social functioning (198). | ||||
| • | A 24-session intervention program in Spanish to develop skills in six areas (medication management, social skills, communication skills, organization and planning, transportation, and financial management) showed improvement in everyday living performance at 6, 12, and 18 months, with no significant change in psychopathology (199, 200). | ||||
Conclusions and recommendations
Our purpose in this review was to synthesize a broad bibliography and to gauge the status of the current knowledge base on Latino mental health research. Hopefully, the review has made apparent the areas of glaring weakness in the research “menu.” We have not attempted a deep analysis, nor an exacting interpretation of this literature beyond primary findings, and inevitably many articles have been excluded in our effort to focus on the most relevant work for our purposes. It is our earnest hope that the rapidly accumulating knowledge about Latino mental health will be examined by researchers and practitioners and that gaps in the knowledge will be addressed through high-quality research followed by rapid dissemination of findings to practitioners. Outstanding problems such as the low enrollment rates in intervention trials require urgent attention from federal research and regulatory agencies. As this review demonstrates, disparities in mental heath care for Latinos remain numerous and are reinforced by inadequate information, which itself could serve to impede progress.
Here are some of the gaps in the research that in our opinion urgently need to be addressed:
| • | We need to learn the frequencies of disorders such as schizophrenia and bipolar illness and to define which groups are at high risk of mental disorders among Hispanic Americans. | ||||
| • | Research is needed on ways to improve access to mental health care for Hispanics. | ||||
| • | Research is needed to improve the identification and treatment of mentally ill Hispanics in primary care and interdisciplinary settings. | ||||
| • | We need to devise means of overcoming specific barriers to mental health care for Hispanics, such as low English proficiency, low educational level, and low health literacy. | ||||
| • | For more effective diagnosis and treatment, more research is needed on differences in the clinical presentation and course of mental illnesses in Hispanics. | ||||
| • | We need to increase the participation of Hispanics in core descriptive, genetic, pharmacological, and psychosocial intervention trials (with the latter adapted as necessary). | ||||
In closing, we offer providers who treat Hispanic patients some practical lessons drawn from our review:
| • | It is important to know the cultural traits that Hispanics share. Yet at the same time we must look for intragroup differences that can influence mental illness and its treatment, such as birthplace, degree of acculturation, English proficiency, and health literacy. | ||||
| • | Cultural sensitivity is critical, but some barriers, such as those presented by language and poor educational level, require specific interventions. | ||||
| • | We must keep in mind that Hispanics are more likely than average to experience non-ethnic-specific barriers to mental health care, such as lack of insurance or medication coverage, ignorance about services, lack of transportation, inability to obtain permission to leave work, and lack of access to child care services. All these factors can significantly affect attendance and compliance. | ||||
| • | Hispanics, especially those who are foreign born, seem to be at lower risk of depression and anxiety disorders but seem to have more protracted illness, possibly as a result of the barriers listed above. | ||||
| • | Hispanics tend to receive mental health care in general care settings. However, for various reasons, including a lower likelihood of self-identification as having a mental disorder, Hispanics are more likely to have mental disorders go unrecognized by health providers. | ||||
| • | We know little about differences in the presentation of mental disorders in Hispanics. Until this gap in our knowledge is filled, we should use inclusive rather than exclusive diagnostic criteria. We also must remember that Hispanics seem more likely to somatize distress and to report psychotic symptoms in the absence of a thought disorder. | ||||
| • | Similarly, we know little about Hispanics’ response to psychiatric medications. Until we learn more, we should use the usual guidelines but provide careful follow-up, especially regarding side effects and compliance. We must also keep in mind that Hispanics are at higher risk of developing metabolic syndrome, obesity, and diabetes. | ||||
| • | To the extent that the literature permits generalization, evidence-based psychotherapeutic and psychosocial interventions appear to be as effective with Hispanics as they are with mainstream treatment populations. However, what remains unknown is whether culturally tailoring these interventions might further enhance treatment effectiveness. | ||||
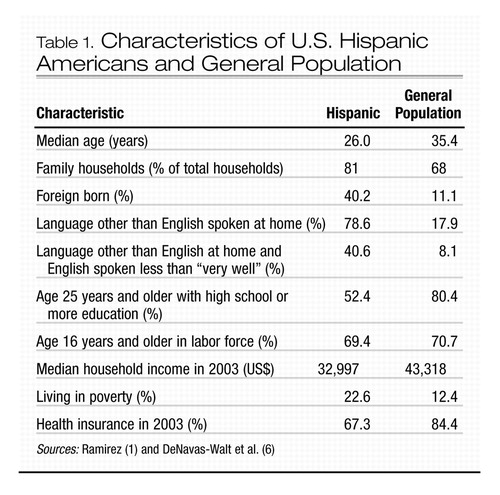 |
Table 1. Characteristics of U.S. Hispanic Americans and General Population
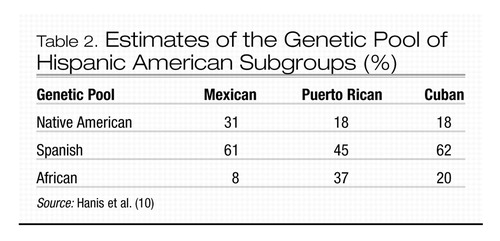 |
Table 2. Estimates of the Genetic Pool of Hispanic American Subgroups (%)
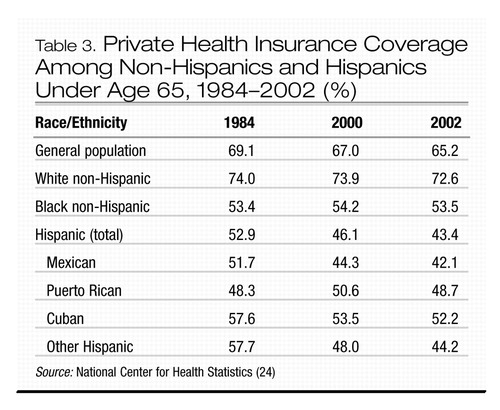 |
Table 3. Private Health Insurance Coverage Among Non-Hispanics and Hispanics Under Age 65, 1984–2002 (%)
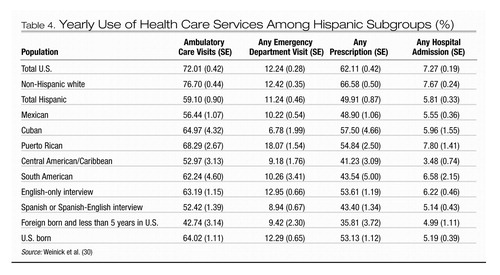 |
Table 4. Yearly Use of Health Care Services Among Hispanic Subgroups (%)
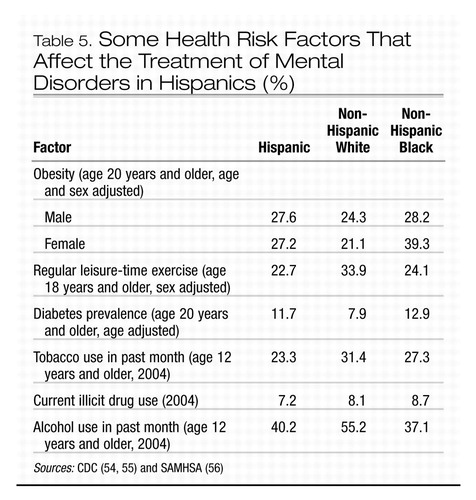 |
Table 5. Some Health Risk Factors That Affect the Treatment of Mental Disorders in Hispanics (%)
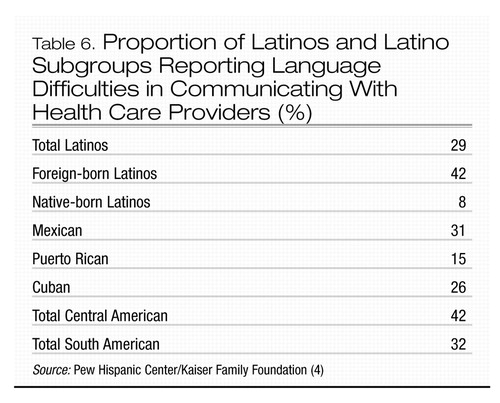 |
Table 6. Proportion of Latinos and Latino Subgroups Reporting Language Difficulties in Communicating With Health Care Providers (%)
 |
Table 7. Language and Unadjusted Relative Risk (RR) for Decreased Health Care Use
1 Ramirez RR: We the People: Hispanics in the United States. Washington, DC, US Census Bureau, December 2004Google Scholar
2 US Census Bureau News: Hispanic population passes 40 million. Washington, DC, US Census Bureau, June 9, 2005Google Scholar
3 US Census Bureau: US Interim Projections by Age, Sex, Race, and Hispanic Origin. Washington, DC, US Census Bureau, 2004. Available at http://www.census.gov/ipc/www/usinterimprojGoogle Scholar
4 Pew Hispanic Center/Kaiser Family Foundation: 2002 National Survey of Latinos: Summary of Findings. Menlo Park, Calif, Henry J. Kaiser Foundation, December 2002Google Scholar
5 Pasel JS: Unauthorized Migrants: Number and Characteristics. Washington, DC, Pew Hispanic Center, June 14, 2005Google Scholar
6 DeNavas-Walt C, Proctor BD, Mills RJ: Income, Poverty, and Health Insurance in the United States: 2003. Washington, DC, US Census Bureau, August 2004Google Scholar
7 Delva J, Wallace JM, O’Malley PM, Bachman JG, Johnston LD, Schulenberg JE: The epidemiology of alcohol, marijuana, and cocaine use among Mexican American, Puerto Rican, Cuban American, and other Latin American eighth-grade students in the United States: 1991–2002. Am J Public Health 2005; 95:696–702Crossref, Google Scholar
8 Bonilla C, Parra EJ, Pfaff CL, Dios S, Marshall JA, Hamman RF, Ferrell RE, Hoggart CL, McKeigue PM, Shriver MD: Admixture in the Hispanics of the San Luis Valley, Colorado, and its implications for complex trait gene mapping. Ann Hum Genet 2004; 68:139–153Crossref, Google Scholar
9 Choudry S, Ung N, Avila PC, Ziv E, Nazario S, Casal J, Torres A, Gorman JD, Salari K, Rodriguez-Santana JR, Toscano M, Sylvia JS, Alioto M, Castro RA, Salazar M, Gomez I, Fagan JK, Salas J, Clark S, Lilly C, Matallana H, Selman M, Chapela R, Sheppard D, Weiss ST, Ford JG, Boushey HA, Drazen JM, Rodriguez-Cintron W, Silverman EK, Burchard EG: Pharmacogenetic differences in response to albuterol between Puerto Ricans and Mexicans with asthma. Am J Respir Crit Care Med 2005; 171:563–570Crossref, Google Scholar
10 Hanis CL, Hewett-Emmett D, Bertin TK, Schull WJ: Origins of US Hispanics: implications for diabetes. Diabetes Care 1991; 14:618–627Crossref, Google Scholar
11 Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DE: Acculturation and Latino health in the United States. Annu Rev Public Health 2005; 26:367–397Crossref, Google Scholar
12 Canino GJ, Bird HR, Shrout PE, Rubio-Stipec M, Bravo M, Martinez R, Sesman M, Guevara LM: The prevalence of specific psychiatric disorders in Puerto Rico. Arch Gen Psychiatry 1987; 44:727–735Crossref, Google Scholar
13 Karno M, Hough RL, Burnam MA, Escobar JI, Timbers DM, Santana F, Boyd JH: Lifetime prevalence of specific psychiatric disorders among Mexican Americans and non-Hispanic whites in Los Angeles. Arch Gen Psychiatry 1987; 44:695–701Crossref, Google Scholar
14 Moscicki EK, Rae D, Regier DA, Locke B: The Hispanic Health and Nutrition Examination Survey: depression among Mexican Americans, Cuban Americans and Puerto Ricans, in Health and Behavior: Research Agenda for Hispanics (Simon Bolivar Research Monograph Series 1). Edited by Gaviria M, Arana JD. Chicago, University of Illinois at Chicago, 1987, pp 145–159Google Scholar
15 Vega WA, Kolody B, Aguilar-Gaxiola S, Alderete E, Catalano R, Caraveo-Anduaga J: Lifetime prevalence of DSM-III-R psychiatric disorders among urban and rural Mexican Americans in California. Arch Gen Psychiatry 1998; 55:771–778Crossref, Google Scholar
16 Vega WA, Sribney WM, Miskimen TM, Escobar JI: Putative psychotic symptoms in the Mexican American population: prevalence and co-occurrence with psychiatric disorders. J Nerv Ment Dis, in pressGoogle Scholar
17 Epstein JA, Botvin GJ, Diaz T: Linguistic acculturation associated with higher marijuana and polydrug use among Hispanic adolescents. Subst Use Misuse 2001; 36:477–499Crossref, Google Scholar
18 Turner RJ, Gil AG: Psychiatric and substance use disorders in South Florida: racial/ethnic and gender contrasts. Arch Gen Psychiatry 2002; 59:43–50Crossref, Google Scholar
19 Gil AG, Vega WA: Latino drug use: scope, risk factors, and reduction strategies, in Health Issues in the Latino Community. Edited by Aguirre-Molina M, Molina CW, Zambrana RE. San Francisco, Jossey-Bass, 2001, pp 435–458Google Scholar
20 Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, Anderson K: Immigration and lifetime prevalence of DSM-IV psychiatric disorders among Mexican Americans and non-Hispanic whites in the United States. Arch Gen Psychiatry 2004; 61:1226–1233Crossref, Google Scholar
21 Gonzalez HM, Haan MN, Hinton L: Acculturation and the prevalence of depression in older Mexican-Americans: baseline results of the Sacramento Area Latino Study on Aging. J Am Geriatr Soc 2001; 49:948–953Crossref, Google Scholar
22 Hovey JD: Acculturative stress, depression, and suicidal ideation in Mexican immigrants. Cultur Divers Ethnic Minor Psychol 2000; 6:134–151Crossref, Google Scholar
23 Sundquist J: Ethnicity as a risk factor for mental illness: a population-based study of 338 Latin American refugees and 996 age-, sex-, and education-matched Swedish controls. Acta Psychiatr Scand 1993; 87:208–212Crossref, Google Scholar
24 National Center for Health Statistics: Health, United States, 2004. Hyattsville, Md, NCHS, 2004Google Scholar
25 US Department of Health and Human Services: 2004 National Healthcare Disparities Report. 2nd printing, March 2005Google Scholar
26 Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC: Twelvemonth use of mental health services in the United States. Arch Gen Psychiatry 2005; 62:629–640Crossref, Google Scholar
27 Washington DL, Villa V, Brown A, Damron-Rodriguez J, Harada N: Racial/ethnic variations in veterans’ ambulatory care. Am J Public Health 2005; 95:2231–2237Crossref, Google Scholar
28 Sullivan MM, Rehm R: Mental health of undocumented Mexican immigrants: a review of the literature. Adv Nurs Sci 2005; 28:240–251Crossref, Google Scholar
29 Guendelman S, Angulo V, Wier M, Oman D: Overcoming the odds: access to care for immigrant children in working poor families in California. Matern Child Health J, Nov 15, 2005:1–12 (epub)Google Scholar
30 Weinick RM, Jacobs EA, Cacari Stone L, Ortega AN, Burstin H: Hispanic healthcare disparities: challenging the myth of a monolithic Hispanic population. Med Care 2004; 42:313–320Crossref, Google Scholar
31 Scott G, Hanyu N: Access to health care among Hispanic/Latino children: United States, 1998–2001. Advance Data from Vital and Health Statistics; No 344. Hyattsville, Md, National Center for Health Statistics, June 24, 2004Google Scholar
32 Sirey JA, Meyers BS, Bruce ML, Alexopoulos GS, Perlick DA, Raue P: Predictors of antidepressant prescription and early use among depressed outpatients. Am J Psychiatry 1999; 156:690–696Google Scholar
33 Skaer TL, Sclar DA, Robison LM, Galin RS: Trends in the rate of depressive illness and use of antidepressant pharmacotherapy by ethnicity/race: an assessment of office-based visits in the United States, 1992–1997. Clin Ther 2000; 22:1575–1589Crossref, Google Scholar
34 Richardson LP, DiGiuseppe D, Garrison M, Christakis DA: Depression in Medicare-covered youth: differences by race and ethnicity. Arch Pediatr Adolesc Med 2003; 157:984–989Crossref, Google Scholar
35 Miranda J, Cooper LA: Disparities in care for depression among primary care patients. J Gen Intern Med 2004; 19:120–126Crossref, Google Scholar
36 Adams GL, Dworkin RJ, Rosenberg SD: Diagnosis and pharmacotherapy issues in the care of Hispanics in the public sector. Am J Psychiatry 1984; 8:970–974Google Scholar
37 Citrome L, Levine J, Allingham B: Utilization of depot neuroleptic medication in psychiatric outpatients. Psychopharmacol Bull 1996; 32:321–326Google Scholar
38 Covell NH, Jackson CT, Evans AC, Essock SM: Antipsychotic prescribing practices in Connecticut’s public mental health system: rates of changing medications and prescribing styles. Schizophr Bull 2002; 28(1):17–29Crossref, Google Scholar
39 Juarez-Reyes MG, Shumway M, Battle C, Bacchetti P, Hansen MS, Hargreaves WA: Clozapine eligilibility: the effect of stringent criteria on ethnic, gender, and age subgroups of schizophrenic patients. Prog Neuropsychopharmacol Biol Psychiatry 1996; 20:1341–1352Crossref, Google Scholar
40 Escalante A, Barrett J, del Rincon I, Cornell JE, Phillips CB, Katz JN: Disparity in total hip replacement affecting Hispanic Medicare beneficiaries. Med Care 2002; 40:447–450Crossref, Google Scholar
41 Greenberg GA, Rosenheck RA: Change in mental health service delivery among blacks, whites, and Hispanics in the Department of Veterans Affairs. Adm Policy Ment Health 2003; 31:31–43Crossref, Google Scholar
42 Virnig B, Huang Z, Lurie N, Musgrave D, McBean AM, Dowd B: Does Medicare managed care provide equal treatment for mental illness across races? Arch Gen Psychiatry 2004; 61:201–205Crossref, Google Scholar
43 Karno M: The enigma of ethnicity in a psychiatric clinic. Arch Gen Psychiatry 1966; 14:516–520Crossref, Google Scholar
44 Karno M, Edgerton RB: Perception of mental illness in a Mexican-American community. Arch Gen Psychiatry 1969; 20:233–238Crossref, Google Scholar
45 Hough RL, Landsverk JA, Karno M, Burnam MA, Timbers DM, Escobar JI, Regier DA: Utilization of health and mental health services by Los Angeles Mexican Americans and non-Hispanic whites. Arch Gen Psychiatry 1987; 44:702–709Crossref, Google Scholar
46 Weinick RM, Zuvekas SH, Cohen JW: Racial and ethnic differences in access to and use of health care services, 1977 to 1996. Med Care Res Rev 2000; 57(suppl 1):36–54Crossref, Google Scholar
47 Barrio C, Yamada AM, Hough RL, Hawthorne W, Garcia P, Jeste DV: Ethnic disparities in use of public mental health case management services among patients with schizophrenia. Psychiatr Serv 2003; 54:1264–1270Crossref, Google Scholar
48 Alegría M, Canino G, Ríos R, Vera M, Calderon J, Rusch D, Ortega AN: Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino whites. Psychiatr Serv 2002; 53:1547–1555Crossref, Google Scholar
49 Vega WA, Kolody B, Aguilar-Gaxiola S, Catalano R: Gaps in service utilization by Mexican Americans with mental health problems. Am J Psychiatry 1999; 156:928–934Crossref, Google Scholar
50 Vega WA, Kolody B, Aguilar-Gaxiola S: Help seeking for mental health problems among Mexican Americans. J Immigr Health 2001; 3(3):133–140Crossref, Google Scholar
51 Lillie-Blanton M, Brodie M, Rowland D, Altman D, McIntosh M: Race, ethnicity, and the health care system: public perceptions and experiences. Med Care Res Rev 2000; 57(suppl 1):218–235Crossref, Google Scholar
52 Caetano R: Alcohol-related health disparities and treatment-related epidemiological findings among whites, blacks, and Hispanics in the United States. Alcohol Clin Exp Res 2003; 27:1337–1339Crossref, Google Scholar
53 Caetano R, McGrath C, Ramisetty-Mikler S, Field CA: Drinking, alcohol problems, and the five-year recurrence and incidence of male to female and female to male partner violence. Alcohol Clin Exp Res 2005; 29:98–106Crossref, Google Scholar
54 Centers for Disease Control and Prevention: Early Release of Selected Estimates Based on Data From the January–September 2004 National Health Interview Survey. Atlanta, CDC, March 2005Google Scholar
55 Centers for Disease Control and Prevention: National Diabetes Fact Sheet. Atlanta, CDC, 2003Google Scholar
56 Substance Abuse and Mental Health Services Administration, Office of Applied Studies: 2004 National Survey on Drug Use and Health, Results (Revisions as of 9/8/2005). Available at http://oas.samhsa.gov/nsduh.htmGoogle Scholar
57 Gordon-Larsen P, Harris KM, Ward DS, Popkin BM; National Longitudinal Study of Adolescent Health: Acculturation and overweight-related behaviors among Hispanic immigrants to the US: the National Longitudinal Study of Adolescent Health. Soc Sci Med 2003; 57:2023–2034Crossref, Google Scholar
58 Zsembik BA, Fennell D: Ethnic variation in health and the determinants of health among Latinos. Soc Sci Med 2005; 61:53–63Crossref, Google Scholar
59 Escobar JI, Randolph ET: The Hispanic and social networks, in Mental Health and Hispanic Americans. Edited by Becerra RM, Karno M, Escobar JI. New York, Grune & Stratton, 1982, pp 41–57Google Scholar
60 López SR, Hipke KN, Polo AJ, Jenkins JH, Karno M, Vaughn C, Snyder KS: Ethnicity, expressed emotion, attributions, and course of schizophrenia: family warmth matters. J Abnorm Psychol 2004; 113:428–439Crossref, Google Scholar
61 Weisman A, Rosales G, Kymalainen J, Armesto J: Ethnicity, family cohesion, religiosity and general emotional distress in patients with schizophrenia and their relatives. J Nerv Ment Dis 2005; 193:359–368Crossref, Google Scholar
62 Kopelowicz A, Zarate R, Gonzalez V, Lopez SR, Ortega P, Obregon N, Mintz J: Evaluation of expressed emotion in schizophrenia: a comparison of Caucasians and Mexican Americans. Schizophr Res 2002; 55:179–186Crossref, Google Scholar
63 Shin HB: Language use and English-speaking ability: 2000. Washington, DC, US Census Bureau, October 2003Google Scholar
64 Derose KP, Baker DW: Limited English proficiency and Latinos’ use of physician services. Med Care Res Rev 2000; 57:76–91Crossref, Google Scholar
65 Flores G, Abreu M, Tomany-Korman SC: Limited English proficiency, primary language at home, and disparities in children’s health care: how language barriers are measured matters. Public Health Rep 2005; 120:418–430Crossref, Google Scholar
66 Gazmararian JA, Baker DW, Williams MV, Parker RM, Scott TL, Green DC, Fehrenbach SN, Ren J, Koplan JP: Health literacy among Medicare enrollees in a managed care organization. JAMA 1999; 281:545–551Crossref, Google Scholar
67 Ayalon L, Alvidrez J, Arean P: Beliefs about the causes of mental illness explains low levels of mental health service use in ethnic minority older adults. Presentation at the Critical Research Issues in Latino Mental Health conference, Princeton, NJ, Nov 2005Google Scholar
68 Leyva M, Sharif I, Ozuah PO: Health literacy among Spanish-speaking Latino parents with limited English proficiency. Ambul Pediatr 2005; 5:56–59Crossref, Google Scholar
69 Fiscella K, Franks P, Doescher MP, Saver BG: Disparities in health care by race, ethnicity, and language among the insured. Med Care 2002; 40:52–59Crossref, Google Scholar
70 Morales LS, Cunningham WE, Brown JA, Liu H, Hays RD: Are Latinos less satisfied with communication by health care providers? J Gen Intern Med 1999; 14:409–417Crossref, Google Scholar
71 Baker DW, Hayes R, Fortier JP: Interpreter use and satisfaction with interpersonal aspects of care for Spanish-speaking patients. Med Care 1998; 36:1461–1470Crossref, Google Scholar
72 Weech-Maldonado R, Elliott MN, Morales LS, Spritzer K, Marshall GN, Hays RD: Health plan effects on patient assessment of Medicaid managed care among racial/ethnic minorities. J Gen Intern Med 2004; 19:130–145Crossref, Google Scholar
73 Sarver J, Baker DW: Effect of language barriers on follow-up appointments after an emergency department visit. J Gen Intern Med 2000; 15:256–264Crossref, Google Scholar
74 John-Baptiste A, Naglie G, Tomlinson G, Alibhai SM, Etchells E, Cheung A, Kapral M, Gold WL, Abrams H, Bacchus M, Krahn M: The effect of English language proficiency on length of stay and in-hospital mortality. J Gen Intern Med 2004; 19:221–228Crossref, Google Scholar
75 Todd KH, Samaroo N, Hoffman JR: Ethnicity as a risk factor for inadequate emergency department analgesia. JAMA 1993; 269:1537–1539Crossref, Google Scholar
76 Ng B, Dimsdale JE, Rollnik JD, Shapiro H: The effect of ethnicity on prescriptions for patient-controlled analgesia for post-operative pain. Pain 1996; 66:9–12Crossref, Google Scholar
77 James CA, Bourgeois FT, Shannon MW: Association of race/ethnicity with emergency department wait times. Pediatrics 2005; 115:310–315Crossref, Google Scholar
78 Hampers LC, Cha S, Gutglass DJ, Binns HJ, Krug SE: Language barriers and resource utilization in a pediatric emergency department. Pediatrics 1999; 103:1253–1256Crossref, Google Scholar
79 Diaz E, Woods SW, Rosenheck RA: Effects of ethnicity on psychotropic medication adherence. Community Ment Health J 2005; 41:521–537Crossref, Google Scholar
80 Carrasquillo O, Orav EJ, Brennan TA, Burstin HR: Impact of language barriers on patient satisfaction in an emergency department. J Gen Intern Med 1999; 14:82–87Crossref, Google Scholar
81 Diaz E, Prigerson H, Desai R, Rosenheck R: Perceived needs and service use of Spanish speaking monolingual patients followed at a Hispanic Clinic. Community Ment Health J 2001; 37:335–346Crossref, Google Scholar
82 Vega WA, Alegría M: Latino mental health and treatment in the United States, in Health Issues in the Latino Community. Edited by Aguirre-Molina M, Molina CW, Zambrana RE. San Francisco, Jossey-Bass, 2001, pp 179–210Google Scholar
83 Riolo SA, Nguyen TA, Greden JF, King CA: Prevalence of depression by race/ethnicity: findings from the National Health and Nutrition Examination Survey III. Am J Public Health 2005; 95:998–1000Crossref, Google Scholar
84 Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE: Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005; 62:593–602Crossref, Google Scholar
85 Hasin DS, Goodwin RD, Stinson FS, Grant BF: Epidemiology of major depressive disorder: results from the National Epidemiologic Survery on Alcoholism and Related Conditions. Arch Gen Psychiatry 2005; 62:1097–1106Crossref, Google Scholar
86 Harris KM, Edlund MJ, Larson S: Racial and ethnic differences in the mental health problems and use of mental health care. Med Care 2005; 43:775–784Crossref, Google Scholar
87 Canino G, Roberts RE: Suicidal behavior among Latino youth: suicide and life-threatening behavior. 2001; 31(suppl):122–131Google Scholar
88 Black SA, Markides KS, Miller TQ: Correlates of depressive symptomatology among older community-dwelling Mexican Americans: the Hispanic EPESE. J Gerontol B Psychol Sci Soc Sci 1998; 53:S198–S208Crossref, Google Scholar
89 Bromberger JT, Harlow S, Avis N, Kravitz HM, Cordal A: Racial/ethnic differences in the prevalence of depressive symptoms among middle-aged women: the Study of Women’s Health Across the Nation (SWAN). Am J Public Health 2004; 94:1378–1385Crossref, Google Scholar
90 Dunlop DD, Song J, Lyons JS, Manheim LM, Chang RW: Racial/ethnic differences in rates of depression among preretirement adults. Am J Public Health 2003; 93:1945–1952Crossref, Google Scholar
91 Saluja G, Iachan R, Scheidt PC, Overpeck MD, Sun W, Giedd JN: Prevalence of and risk factors for depressive symptoms among young adolescents. Arch Pediatr Adolesc Med 2004; 158:760–765Crossref, Google Scholar
92 Breslau J, Kendler KS, Su M, Gaxiola-Aguilar S, Kessler RC: Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychol Med 2005; 35:317–327Crossref, Google Scholar
93 Golding JM, Lipton RI: Depressed mood and major depressive disorder in two ethnic groups. J Psychiatr Res 1990; 24:65–82Crossref, Google Scholar
94 Jablensky A: The epidemiological horizon, in Schizophrenia, 2nd ed. Edited by Hirsch SR, Weinberger D. Oxford, UK, Blackwell Publishing, 2003, pp 203–231Google Scholar
95 Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, Ruan WJ, Huang B: Prevalence, correlates, and comorbidity of bipolar I disorder and axis I and II disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry 2005; 66:1205–1215Crossref, Google Scholar
96 Malzberg B: Dementia precox (schizophrenia), in Mental Disease Among the Puerto Rican Population of New York State 1960–61. Edited by Malzberg B. Albany, NY, Research Foundation for Mental Hygiene, 1965, pp 34–56Google Scholar
97 Malzberg B: Mental disease among Puerto Ricans in New York City, 1949–51, in Migration in Relation to Mental Disease. Edited by Malzberg B. Albany, NY, Research Foundation for Mental Hygiene, 1968, pp 170–192Google Scholar
98 Jaco EG: Mental health of the Spanish-American in Texas, in Culture and Mental Health: Cross-Cultural Studies. Edited by Opler MK. New York, Macmillan, 1959, pp 467–485Google Scholar
99 Karno M: The enigma of ethnicity in a psychiatric clinic. Arch Gen Psychiatry 1966; 14:516–520Crossref, Google Scholar
100 Karno M, Edgerton RB: Perception of mental illness in a Mexican-American community. Arch Gen Psychiatry 1969; 20:233–238Crossref, Google Scholar
101 Burnam MA, Hough RL, Escobar JI, Karno M, Timbers DM, Telles CA, Locke BZ: Six-month prevalence of specific psychiatric disorders among Mexican-Americans and non-Hispanic whites in Los Angeles. Arch Gen Psychiatry 1987; 44:687–694Crossref, Google Scholar
102 Karno M, Hough RL, Burnam MA, Escobar JI, Timbers DM, Santana F, Boyd JH: Lifetime prevalence of specific psychiatric disorders among Mexican Americans and non-Hispanic whites in Los Angeles. Arch Gen Psychiatry 1987; 44:695–701Crossref, Google Scholar
103 Canino GJ, Bird HR, Shrout PE, Rubio-Stipec M, Bravo M, Martinez R, Sesman M, Guevara LM: The prevalence of specific psychiatric disorders in Puerto Rico. Arch Gen Psychiatry 1987; 44:727–735Crossref, Google Scholar
104 Keith SJ, Regier DA, Rae DS: Schizophrenic disorders, in Psychiatric Disorders in America: The Epidemiological Catchment Area Study. Edited by Robins LN, Regier DA. New York, Free Press, 1991, pp 33–52Google Scholar
105 Eaton W, Harrison G: Ethnic disadvantage and schizophrenia. Acta Psychiatr Scand 2000; 102(suppl 407):38–43Crossref, Google Scholar
106 Cantor-Graae E, Selten JP: Schizophrenia and migration: a meta-analysis and review. Am J Psychiatry 2005; 162:12–24Crossref, Google Scholar
107 Perkins P, Annegers JF, Doody RS, Cooke N, Aday L, Vernon SW: Incidence and prevalence of dementia in a multiethnic cohort of municipal retirees. Neurology 1997; 49:44–50Crossref, Google Scholar
108 Fitten LJ, Ortiz F, Ponton M: Frequency of Alzheimer’s disease and other dementias in a community sample of Hispanics. J Am Geriatr Soc 2001; 49:1301–1308Crossref, Google Scholar
109 Demirovic J, Prineas R, Loewenstein D, Bean J, Duara R, Sevush S, Szapocznik J: Prevalence of dementia in three ethnic groups: the South Florida Program on Aging and Health. Ann Epidemiol 2003; 13:472–478Crossref, Google Scholar
110 Tan MX, Stern Y, Marder K, Bell K, Gurland B, Lantigua R, Andrews H, Feng L, Tycko B, Mayeux R: The APOE-ε4 allele and the risk of Alzheimer’s disease among African Americans, whites, and Hispanics. JAMA 1998; 279:751–755Crossref, Google Scholar
111 Borowsky SJ, Rubenstein LV, Meredith LS, Camp P, Jackson-Triche M, Wells KB: Who is at risk of nondetection of mental health problems in primary care? J Gen Intern Med 2000; 15:381–388Crossref, Google Scholar
112 Schmaling KB, Hernandez DV: Detection of depression among low-income Mexican Americans in primary care. J Health Care Poor Underserved 2005; 16:780–790Crossref, Google Scholar
113 Heneghan AM, Johnson Silver E, Bauman LJ, Stein RE: Do pediatricians recognize mothers with depressive symptoms? Pediatrics 2000; 106:1367–1373Crossref, Google Scholar
114 Crystal S, Sambamoorthi U, Walkup JT, Akincigil A: Diagnosis and treatment of depression in the elderly Medicare population: predictors, disparities, and trends. J Am Geriatr Soc 2003; 51:1718–1728Crossref, Google Scholar
115 Stevens J, Harman JS, Kelleher KJ: Ethnic and regional differences in primary care visits for attention-deficit hyperactivity disorder. J Dev Behav Pediatr 2004; 25:318–325Crossref, Google Scholar
116 Stevens J, Harman JS, Kelleher KJ: Race/ethnicity and insurance status as factors associated with ADHD treatment patterns. J Child Adolesc Psychopharmacol 2005; 15:88–96Crossref, Google Scholar
117 Raghavan R, Zima BT, Andersen RM, Leibowitz AA, Schuster MA, Landsverk J: Psychotropic medication use in a national probability sample of children in the Child Welfare System. J Child Adolesc Psychopharmacol 2005; 15:97–106Crossref, Google Scholar
118 Pastor PN, Reuben CA: Racial and ethnic differences in ADHD and LD in young school-age children: parental reports in the National Health Interview Survey. Public Health Rep 2005; 120:383–392Crossref, Google Scholar
119 Roberts RE, Alegría M, Ramsay Roberts CR, Chen IG: Mental health problems of adolescents as reported by their caregivers. J Behav Health Serv Res 2005; 32:1–13Crossref, Google Scholar
120 Chaudron LH, Kitzman HJ, Peifer KL, Morrow S, Perez LM, Newman MC: Prevalence of maternal depressive symptoms in low-income Hispanic women. J Clin Psychiatry 2005; 66:418–423Crossref, Google Scholar
121 Meadow A, Stoker D: Symptomatic behavior of hospitalized patients. Arch Gen Psychiatry 1965; 12:267–277Crossref, Google Scholar
122 Fabrega H, Swartz JD, Wallace CA: Ethnic differences in psychopathology, I: clinical correlates under varying conditions. Arch Gen Psychiatry 1968; 19:218–226Crossref, Google Scholar
123 Fabrega H, Swartz JD, Wallace CA: Ethnic differences in psychopathology, II: specific differences with emphasis on a Mexican American group. J Psychiatr Res 1968; 6:221–235Crossref, Google Scholar
124 Pokorny AD, Overall JE: Relationships of psychopathology to age, sex, ethnicity, education and marital status in state hospital patients. J Psychiatr Res 1970; 7:143–152Crossref, Google Scholar
125 Heiman EM, Kahn MW: Mexican American and European American psychopathology and hospital course. Arch Gen Psychiatry 1977; 34:167–170Crossref, Google Scholar
126 Lawson HH, Kahn MW, Heiman EM: Psychopathology, treatment outcome, and attitude toward mental illness in Mexican Americans and European patients. Int J Soc Psychiatry 1982; 28:20–26Crossref, Google Scholar
127 Adams GL, Dworkin RJ, Rosenberg SD: Diagnosis and pharmacotherapy issues in the care of Hispanics in the public sector. Am J Psychiatry 1984; 8:970–974Google Scholar
128 Randolph ET, Escobar JI, Paz DH, Forsythe AB: Ethnicity and reporting of schizophrenic symptoms. J Nerv Ment Dis 1985; 173:332–340Crossref, Google Scholar
129 Escobar JI, Randolph ET, Hill M: Symptoms of schizophrenia in Hispanic and Anglo veterans. Cult Med Psychiatry 1986; 10:259–276Crossref, Google Scholar
130 Brekke JS, Barrio C: Cross-ethnic symptom differences in schizophrenia: the influence of culture and minority status. Schizophr Bull 1997; 23:305–316Crossref, Google Scholar
131 Decnop Coelho VL, Strauss ME, Hunter Jenkins J: Expression of symptomatic distress by Puerto Rican and Euro-American patients with depression and schizophrenia. J Nerv Ment Dis 1998; 186:477–483Crossref, Google Scholar
132 Dasori AM, Alexander LM, Velligan D, Saldana D, Diamond P, Mathurin R: Ethnicity and negative symptoms in patients with schizophrenia. Cult Divers Ment Health 1998; 4:65–69Crossref, Google Scholar
133 Weisman AG, Lopez SR, Ventura J, Nuechterlein KH, Goldstein MJ, Hwang S: A comparison of psychiatric symptoms between Anglo-Americans and Mexica-Americans with schizophrenia. Schizophr Bull 2000; 26:817–824Crossref, Google Scholar
134 Barrio C, Yamada AM, Atuel H, Hough RL, Yee S, Berthot B, Russo PA: A tri-ethnic examination of symptom expression on the positive and negative syndrome scale in schizophrenia spectrum disorders. Schizophr Res 2003; 60:259–269Crossref, Google Scholar
135 Mukherjee S, Shukla S, Woodle J, Rosen AM, Olarte S: Misdiagnosis of schizophrenia in bipolar patients: a multiethnic comparison. Am J Psychiatry 1983; 140:1571–1574Crossref, Google Scholar
136 Chen YR, Swann AC, Burt DB: Stability of diagnosis in schizophrenia. Am J Psychiatry 1996; 153:682–686Crossref, Google Scholar
137 Kales HC, Blow FC, Bingham CR, Copeland LA, Mellow AM: Race and inpatient psychiatric diagnoses among elderly veterans. Psychiatr Serv 2000; 51:795–800Crossref, Google Scholar
138 Minsky S, Vega W, Miskimen T, Gara M, Escobar J: Diagnostic patterns in Latino, African American, and European American psychiatric patients. Arch Gen Psychiatry 2003; 60:637–644Crossref, Google Scholar
139 Dilsaver SC, Akiskal HS: High rates of unrecognized bipolar mixed states among destitute Hispanic adolescents referred for “major depressive disorder.” J Affect Disord 2005; 84:179–186Crossref, Google Scholar
140 Olfson M, Lewis-Fernandez R, Weissman MM, Feder A, Gameroff MJ, Pilowsky D, Fuentes M: Psychotic symptoms in an urban general medicine practice. Am J Psychiatry 2002; 159:1412–1419Crossref, Google Scholar
141 Posternak MA, Zimmerman M: Elevated rates of psychosis among treatment-seeking Hispanic patients with major depression. J Nerv Ment Dis 2005; 193:66–69Crossref, Google Scholar
142 Geltman D, Chang G: Hallucinations in Latino psychiatric outpatients: a preliminary investigation. Gen Hosp Psychiatry 2004; 26:153–157Crossref, Google Scholar
143 Nowell DD, Estes SE: Differential endorsement of hallucination experience among hispanics and non-Hispanic patients: increasing diagnostic accuracy and utility of the clinical interview. Presentation at the Critical Research Issues in Latino Mental Health conference, Princeton, NJ, Nov 2005Google Scholar
144 Marin H, Escobar JI: Special issues in the psychopharmacological management of Hispanic Americans. Psychopharmacol Bull 2001; 35:197–212Google Scholar
145 DuAlba L, Scott R: Somatization and malingering for workers compensation applicants: a cross-cultural MMPI study. J Clin Psychol 1993; 49:913–917Crossref, Google Scholar
146 Myers HF, Lesser I, Rodriguez N, Mira CB, Hwang WC, Camp C, Anderson D, Erickson L, Wohl M: Ethnic differences in clinical presentation of depression in adult women. Cultur Divers Ethnic Minor Psychol 2002; 8:138–156Crossref, Google Scholar
147 Varela RE, Vernberg EM, Sanchez-Sosa JJ, Riveros A, Mitchell M, Mashunkashey J: Anxiety reporting and culturally associated interpretation biases and cognitive schemas: a comparison of Mexican, Mexican American, and European American families. J Clin Child Adolesc Psychol 2004; 33:237–247Crossref, Google Scholar
148 Marcos LR, Murray A, Urcuyo L, Kesselman M: The effect of interview language on the evaluation of psychopathology in Spanish-American schizophrenic patients. Am J Psychiatry 1973; 130:549–553Crossref, Google Scholar
149 Marcos LR, Urcuyo L, Kesselman M, Murray A: The language barrier in evaluating Spanish-American patients. Arch Gen Psychiatry 1973; 29:655–659Crossref, Google Scholar
150 Del Castillo JC: The influence of language upon symptomatology in foreign-born patients. Am J Psychiatry 1970; 127:160–162Crossref, Google Scholar
151 Price C, Cuellar I: Effects of language and related variables on the expression of psychopathology in Mexican American psychiatric patients. Hisp J Behav Sci 1981; 3:145–160Crossref, Google Scholar
152 Malgady RG, Costantino G: Symptom severity in bilingual Hispanics as a function of clinician ethnicity and language of interview. Psychol Assess 1998; 10:120–127Crossref, Google Scholar
153 Lam YWF, Casto DT, Dunn JF: Drug metabolizing capacity in Mexican Americans. Clin Pharmacol Ther 1991; 49:159Google Scholar
154 Mendoza R, Wan YJ, Poland RE, Smith M, Zheng Y, Berman N, Lin KM. CYP2D6 polymorphism in a Mexican American population. Clin Pharmacol Ther 2001; 70:552–560Crossref, Google Scholar
155 Casner PR: The effect of CYP2D6 polymorphisms on dextromethorphan metabolism in Mexican Americans. J Clin Pharmacol 2005; 45:1230–1235Crossref, Google Scholar
156 Paris PL, Kupelian PA, Hall JM, Williams TL, Levin H, Klein EA, Casey G, Witte JS: Association between a CYP3A4 genetic variant and clinical presentation in African-American prostate cancer patients. Cancer Epidemiol Biomarkers Prev 1999; 8:901–905Google Scholar
157 Peng F, Labelle LA, Rainey BJ, Tsongalis GJ: Single nucleotide polymorphisms in the methylenetetrahydrofolate reductase gene are common in Caucasian and Hispanic American populations. Int J Mol Med 2001; 8:509–511Google Scholar
158 Johnson JA: Influence of race or ethnicity on pharmacokinetics of drugs. J Pharm Sci 1997; 86:1328–1333Crossref, Google Scholar
159 Wan YJ, Poland R, Lin KM: Genetic polymorphism of CYP2E1, ADH2, and ALDH2 in Mexican-Americans. Genet Test 1998; 2:79–83Crossref, Google Scholar
160 Poland RA, Lin KM, Nuccio C, Wilkinson GR: Cytochrome P450 2E1 and 3A activities do not differ between Mexican and European Americans. Clin Pharmacol Ther 2002; 72:288–293Crossref, Google Scholar
161 Lam YWF, Jann MW, Chang WH, Yu HS, Lin SK, Chen H, Davis CM: Intra-and inter-ethnic variability in reduced haloperidol to haloperidol ratios. J Clin Pharmacol 1995; 35:128–136Crossref, Google Scholar
162 Evelyn B, Toigo T, Banks D, Pohl D, Gray K, Robins B, Ernat J: Participation of racial/ethnic groups in clinical trials and race-related labeling: a review of new molecular entities approved 1995–1999. J Natl Med Assoc 2001; 93(suppl 12):18S–24SGoogle Scholar
163 Buckley PF: Hot Topics on CATIE. Presentation at the 18th annual US Psychiatric and Mental Health Congress, Las Vegas, Nov 2005Google Scholar
164 Gonzalez J, Thompson P, Escamilla M, Araga M, Farrelly N, Thase ME, Bowden C: Illness and treatment characteristics among Anglos, African Americans and Latinos with bipolar disorder: findings from the first 2000 patients in the Systematic Treatment Enhancement Program for Bipolar Disorder. Poster presentation at the Critical Research Issues in Latino Mental Health conference, Princeton, NJ, Nov 2005Google Scholar
165 Roy-Byrne PP, Perera P, Pitts CD, Christi JA: Paroxetine response and tolerability among ethnic minority patients with mood or anxiety disorders: a pooled analysis. J Clin Psychiatry 2005; 66:1228–1233Crossref, Google Scholar
166 Wagner GJ, Maguen S, Rabkin JG: Ethnic differences in response to fluoxetine in a controlled trial with depressed HIV-positive patients. Psychiatr Serv 1998; 49:239–240Crossref, Google Scholar
167 Alonso M, Val E, Rapaport MH: An open label study of SSRI treatment in depressed Hispanic and non-Hispanic women (letter). J Clin Psychiatry 1997; 58:31Crossref, Google Scholar
168 Ferrando SJ, Rabkin JG, de Moore GM, Rabkin R: Antidepressant treatment of depression in HIV-seropositive women. J Clin Psychiatry 1999; 60:741–746Crossref, Google Scholar
169 Sanchez-Lacay JA, Lewis-Fernandez R, Goetz D, Blanco C, Salman E, Davies S, Liebowitz M: Open trial of nefazodone among Hispanics with major depression: efficacy, tolerability, and adherence issues. Depress Anxiety 2001; 13:118–124Crossref, Google Scholar
170 Currier MB, Molina G, Kato M: Citalopram treatment of major depressive disorder in Hispanic HIV and AIDS patients: a prospective study. Psychosomatics 2004; 45:210–216Crossref, Google Scholar
171 Frackiewicz E, Herrera JM, Sramek JJ, Collazo Y, Lawson WB: Risperidone in the treatment of Hispanic inpatients with schizophrenia: a pilot study. Psychiatry 2002; 65:371–374Crossref, Google Scholar
172 Sramek J, Roy S, Ahrens T, Pinanong P, Cutler NR, Pi E: Prevalence of tardive dyskinesia among three ethnic groups of chronic psychiatric patients. Hosp Community Psychiatry 1991; 42:590–592Google Scholar
173 Adams GL, Dworkin RJ, Rosenberg SD: Diagnosis and pharmacotherapy issues in the care of Hispanics in the public sector. Am J Psychiatry 1984; 8:970–974Google Scholar
174 Collazo Y, Tam R, Sramek J, Herrera J: Neuroleptic dosing in Hispanic and Asian inpatients with schizophrenia. Mt Sinai J Med 1996; 63:310–313Google Scholar
175 Ruiz S, Chu P, Sramek J, Rotavu E, Herrera J: Neuroleptic dosing in Asian and Hispanic outpatients with schizophrenia. Mt Sinai J Med 1996; 63:306–309Google Scholar
176 Ruiz P, Varner RV, Small DR, Johnson BA: Ethnic differences in the neuroleptic treatment of schizophrenia. Psychiatr Q 1999; 70:163–172Crossref, Google Scholar
177 Leslie DL, Rosenheck RA: Use of pharmacy data to assess quality of pharmacotherapy for schizophrenia in a national health care system. Med Care 2001; 39:923–933Crossref, Google Scholar
178 Kato MM, Currier MB, Gomez CM, Hall L, Gonzalez-Blanco M: Prevalence of metabolic syndrome in Hispanic and non-Hispanic patients with schizophrenia. J Clin Psychiatry 2004; 6:74–77Google Scholar
179 Opolka JL, Rascati KL, Brown CM, Gibson PJ: Role of ethnicity in predicting antipsychotic medication adherence. Ann Pharmacother 2003; 37:625–630Crossref, Google Scholar
180 Sleath B, Rubin RH, Huston SA: Hispanic ethnicity, physician-patient communication, and antidepressant adherence. Compr Psychiatry 2003; 44:198–204Crossref, Google Scholar
181 Hosch HM, Barrientos GA, Fierro C, Fierro C, Ramirez JI: Predicting adherence to medications by Hispanics with schizophrenia. Hisp J Behav Sci 1995; 17:320–333Crossref, Google Scholar
182 Jenkins JH: Subjective experience of persistent schizophrenia and depression among US Latinos and Euro-Americans. Br J Psychiatry 1997; 171:20–28Crossref, Google Scholar
183 Diaz E, Neuse E, Woods S, Rosenheck R: Ethnocultural determinants of medication adherence. Poster presentation at the 156th annual meeting of the American Psychiatric Association, San Francisco, May 2003Google Scholar
184 Miranda J, Bernal G, Lau A, Kohn L, Hwang WC, LaFromboise T: State of the science on psychosocial interventions for ethnic minorities. Annu Rev Clin Psychol 2005; 1:113–142Crossref, Google Scholar
185 Rosselló J, Bernal G: The efficacy of cognitive-behavioral and interpersonal treatments for depression in Puerto Rican adolescents. J Consult Clin Psychol 1999; 67:734–745Crossref, Google Scholar
186 Comas-Diaz L: Effects of cognitive and behavioral group treatment on the depressive symptoms of Puerto Rican women. J Consult Clin Psychol 1981; 49:627–632Crossref, Google Scholar
187 Markowitz JC, Spielman LA, Sullivan M, Fishman B: An exploratory study of ethnicity and psychotherapy outcome among HIV-positive patients with depressive symptoms. J Psychother Pract Res 2000; 9:226–231Google Scholar
188 Miranda J, Azocar F, Organista KC, Dwyer E, Arean P: Treatment of depression among impoverished primary care patients from ethnic minority groups. Psychiatr Serv 2003; 54:219–225Crossref, Google Scholar
189 Miranda J, Chung JY, Green BL, Krupnick J, Siddique J, Revicki DA, Belin T: Treating depression in predominantly low-income young minority women. JAMA 2003; 290:57–65Crossref, Google Scholar
190 Miranda J, Duan N, Sherbourne C, Schoenbaum M, Lagomasino I, Jackson-Triche M, Wells KB: Improving care for minorities: can quality improvement interventions improve care and outcomes for depressed minorities? Results of a randomized, controlled trial. Health Serv Res 2003; 38:613–630Crossref, Google Scholar
191 Miranda J, Schoenbaum M, Sherbourne C, Duan N, Wells K: The effects of primary care depression treatment on minority patients’ clinical status and employment. Arch Gen Psychiatry 2004; 61:827–834Crossref, Google Scholar
192 Areán PA, Ayalon L, Hunkeler E, Lin EH, Tang L, Harpole L, Hendrie H, Williams JW, Unutzer J, IMPACT Investigators: Improving depression care for older minority patients in primary care. Med Care 2005; 43:381–390Crossref, Google Scholar
193 Silverman WK, Kurtines WM, Ginsburg GS, Weems CF, Lumpkin PW, Carmichael DH: Treating anxiety disorders in children with group cognitive-behavioral therapy: a randomized clinical trial. J Consult Clin Psychol 1999; 67:993–1003Google Scholar
194 Silverman WK, Kurtines WM, Ginsburg GS, Weems CF, Rabian B, Serafini LT: Contingency management, self-control, and education support in the treatment of childhood phobic disorders: a randomized clinical trial. J Consult Clin Psychol 1999; 67:675–687Crossref, Google Scholar
195 Pina AA, Silverman WK, Fuentes RM, Kurtines WM, Weems CF: Exposure-based cognitive-behavioral treatment for phobic and anxiety disorders: treatment effects and maintenance for Hispanic/Latino relative to European-American youths. J Am Acad Child Adolesc Psychiatry 2003; 42:1179–1187Crossref, Google Scholar
196 Telles C, Karno M, Mintz J, Paz G, Arias M, Tucker D, Lopez S: Immigrant families coping with schizophrenia: behavioral family intervention v case management with a low-income Spanish-speaking population. Br J Psychiatry 1995; 167:473–479Crossref, Google Scholar
197 Sung-Woo B, Brekke JS, Bola JR: Ethnicity and treatment outcome variation in schizophrenia. J Nerv Ment Dis 2004; 192:623–628Crossref, Google Scholar
198 Kopelowicz A, Zarate R, Gonzalez V, Lopez SR, Ortega P, Obregon N, Mintz J: Disease management in Latinos with schizophrenia: a family-assisted, skills training approach. Schizophr Bull 2003; 29:211–225Crossref, Google Scholar
199 Patterson TL, Bucardo J, McKibbin CL, Mausbach BT, Moore D, Barrio C, Goldman SR, Jeste DV: Development and pilot testing of a new psychosocial intervention for older Latinos with chronic psychosis. Schizophr Bull 2005; 31:922–930Crossref, Google Scholar
200 Bucardo J, Mausbach BT, Barrio C, McKibbin CL, Goldman SR, Lebowitz B, Jeste DV, Patterson TL: Psychosocial treatment in Spanish for older latinos with schizophrenia and other psychotic disorders. Presentation at the Critical Research Issues in Latino Mental Health conference, Princeton, NJ, Nov 2005Google Scholar



