DSM-IV Mania Symptoms in a Prepubertal and Early Adolescent Bipolar Disorder Phenotype Compared to Attention-Deficit Hyperactive and Normal Controls
Abstract
Objective: To compare the prevalence of Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) mania symptoms in a prepubertal and early adolescent bipolar disorder phenotype (PEA-BP) to those with attention deficit hyperactivity disorder (ADHD) and normal community controls (CC). Methods: To optimize generalizeability, subjects with PEA-BP and ADHD were consecutively ascertained from outpatient pediatric and psychiatric sites, and CC subjects were obtained from a random survey. All 268 subjects (93 with PEA-BP, 81 with ADHD, and 94 CC) received comprehensive, blind, baseline research assessments of mothers about their children and of children about themselves. PEA-BP was defined by DSM-IV mania with elation and/or grandiosity as one criterion to ensure that subjects had one of the two cardinal symptoms of mania and to avoid diagnosing mania only by criteria that overlapped with those for ADHD. Results: Five symptoms (i.e., elation, grandiosity, flight of ideas/racing thoughts, decreased need for sleep, and hypersexuality) provided the best discrimination of PEA-BP subjects from ADHD and CC controls. These five symptoms are also mania-specific in DSM-IV (i.e., they do not overlap with DSM-IV symptoms for ADHD). Irritability, hyperactivity, accelerated speech, and distractibility were very frequent in both PEA-BP and ADHD groups and therefore were not useful for differential diagnosis. Concurrent elation and irritability occurred in 87.1% of subjects with PEA-BP. Data on suicidality, psychosis, mixed mania, and continuous rapid cycling were also provided. Conclusion: Unlike late teenage/adult onset bipolar disorder, even subjects with PEA-BP selected for DSM-IV mania with cardinal symptoms have high rates of comorbid DSM-IV ADHD. High rates of concurrent elation and irritability were similar to those in adult mania.
Introduction
This article reports the prevalence of baseline Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV: American Psychiatric Association 1994) mania symptoms in 268 consecutively ascertained subjects (93 with a prepubertal and early adolescent bipolar disorder phenotype [PEA-BP], 81 with attention deficit hyperactivity disorder [ADHD], and 94 normal community controls [CC]) in the ongoing “Phenomenology and Course of Pediatric Bipolar Disorders” study (Geller et al. 1998c, 1998d, 2000a, 2000b, 2000c, 2001a, 2001b, in press-a). A comparison of the first 60 PEA-BP and the first 60 ADHD subjects was previously reported (Geller et al. 1998c, 1998d). This article expands these prior reports to the entire baseline sample.
Controversy over the existence of child-onset mania centered on the high prevalence of comorbid ADHD in mania samples and on the overlap of certain mania criteria with those for ADHD (e.g., hyperactivity, distractibility) (Faraone et al. 1997; Fristad et al. 1992; Geller et al. 1995, 2000b; National Institute of Mental Health Research Roundtable on Prepubertal Bipolar Disorder [NIMH Roundtable] 2001). This was in contrast to older adolescents and adults, in whom the differential diagnoses for bipolar disorder included schizophrenia and substance use disorders (Gershon et al. 1982; Horowitz 1975, 1977).
Our group addressed the issue of differentiating child mania from ADHD by investigating a PEA-BP phenotype defined as current DSM-IV mania with at least one of the two cardinal symptoms of mania (i.e., elated mood and/or grandiosity). Cardinal symptoms in DSM-IV are those that are essentially pathognomonic to a diagnosis. For example, the diagnosis of DSM-IV major depressive disorder (MDD) requires the cardinal symptoms of sad mood and/or anhedonia.
Reasons for selecting a DSM-IV PEA-BP characterized by elation and/or grandiosity were the following. To ensure that mania was not diagnosed using only criteria that overlapped with those for ADHD (e.g., irritability, hyperactivity, distractibility), to ensure that PEA-BP subjects had at least one of the cardinal features of mania (i.e., elation and/or grandiosity), and to increase the likelihood of continuity with the late-teenage/adult-onset bipolar disorder. The PEA-BP has been validated by reliable assessment (Geller et al. 2001b), 6-month stability of mania criteria and diagnoses (Geller et al. 2000c), and 1- and 2-year diagnostic longitudinal outcome (Geller et al. 2001a, in press). The rationale for combining prepubertal and early adolescent subjects into the same phenotype has also been reported (Geller et al. 2000b).
To our knowledge this is the first controlled study of DSM-IV symptom prevalences in a sample ascertained for a PEA-BP.
Methods
Study inclusion and exclusion criteria
Inclusion criteria for the PEA-BP group were 7–16 years old, males and females, good physical health, and severity at a level of definite caseness measured by a Children’s Global Assessment Scale (CGAS) score ≤60 (Bird et al. 1987; Shaffer et al. 1983). Subjects also needed DSM-IV current mania (or bipolar disorder-I manic or mixed phase) for at least 2 weeks, DSM-IV current hypomania (or bipolar disorder-II [or cyclothymia] manic or mixed phase) for at least 2 months, and elated mood and/or grandiosity as one of the mania/hypomania criteria. Exclusion criteria for the PEA-BP group were: adopted, IQ<70, pervasive developmental disorders, schizophrenia, epilepsy or other major medical or neurological disorder, and baseline substance dependency or pregnancy.
Inclusion criteria for the ADHD group were age 7–16 years, males and females, good physical health, definite caseness (CGAS≤60), DSM-IV ADHD (with hyperactivity, i.e., combined or hyperactive/impulsive types) with an onset before age 7 and with a duration ≥6 months. Exclusion criteria for the ADHD group were the same as those for the PEA-BP group, with the addition of major depressive disorder (MDD) and any bipolar disorder diagnosis.
The CC group was aggregately matched to the PEA-BP subjects by age, gender, socioeconomic status (SES), ethnicity, and zip code, were in good physical health; and had definite noncaseness CGAS≥70). Exclusion criteria for the CC group were the same as those for the PEA-BP group, with the addition of any current or past bipolar disorder diagnoses, MDD, or ADHD.
The rationales for these inclusion and exclusion criteria were the following. The duration criteria for PEA-BP were similar to conservative durations in multiple nosological schemas. Conservative durations were selected to increase the likelihood of caseness and to address the controversies in the field (NIMH Roundtable 2001). Current episodes of mania or hypomania were needed because this was a phenomenology study. Subjects with ultradian (continuous) rapid cycling (≥1 cycle/day lasting ≥4 hours) needed to have a cycle every day for at least 2 weeks for mania or at least 2 months for hypomania. The mean number of cycles/day was 3.7 (SD=2.1), consistent with continuous rapid cycling (Geller et al. 2000b). The rationale for the elation/grandiosity criterion is as given in the Introduction. A lower age of 7 was chosen because of credibility of interview assessments, and an upper age of 16 was selected so those subjects would still be teenagers at the 2-year follow-up assessment (Geller et al. in press-a). In the contrast psychiatric group, only ADHD and not attention deficit disorder was selected because the hyperactivity component was one of the major issues in differential diagnosis. Also, the ADHD subjects (and the PEA-BP subjects) could have conduct and/or oppositional defiant disorders because these were common comorbidities among children with ADHD, so excluding them would have produced an atypical ADHD sample. CGAS (Bird et al. 1987; Shaffer et al. 1983) scores were selected to ensure definite caseness for the PEA-BP and ADHD groups and definite noncaseness for the CC subjects. On this scale, 100 is best and 0 is worst functioning. Scores of ≤60 were definite cases, and ≥70 were definite noncases (Bird et al. 1987). At baseline only, substance use disorders and/or pregnancy were exclusion criteria to avoid confounding the diagnosis of bipolar disorder with mental status effects of substance use or gestational state. Subjects continued in the follow-up phase of the “Phenomenology” study if they developed substance use diagnoses or became pregnant after baseline. Because the mean age of the PEA-BP subjects at baseline was 10.9 years (SD=2.6 years), it is unlikely that this exclusion criterion affected the generalizeability of the study findings. Adoption was an exclusion criterion due to concurrent family and genetic studies.
Subject ascertainment
To optimize generalizeability, consecutive case ascertainment from outpatient child psychiatry and pediatric sites was used to recruit subjects with PEA-BP and ADHD. These were outpatient sites because the planned inpatient sites at Barnes Hospital and at St. Louis Children’s Hospital (both within the Washington University Medical Complex) closed soon after the project began. The outpatient sites were largely primary care centers for patients seeking pediatric care or the primary psychiatric center for subjects in large local health maintenance organizations. Records of every new patient at the ascertainment sites were reviewed by nonblind research nurses (i.e., different individuals from the blind research nurses who conducted the research assessments). Telephone screenings were administered to all potentially eligible cases (e.g., subjects with clear exclusionary criteria such as major medical illnesses or those not in the study age range did not receive a telephone screening). Subjects who were still eligible after the telephone screening were scheduled for in-person baseline assessments performed by blind research nurses. During the time that the 93 PEA-BP and 81 ADHD subjects were ascertained, 1,468 total new consecutive cases were seen at the pediatric and psychiatric ascertainment sites. Each of these cases was reviewed by a research nurse for any obvious study exclusionary criteria (e.g., diabetes mellitus, mental retardation, epilepsy). Of the 1,468 cases, 1,111 were from the psychiatric sites and 357 were from the pediatric sites. After chart review, 854 cases were excluded. Of the remaining 614 cases, telephone screening excluded an additional 162 cases, 144 cases refused participation at the telephone screening, and 308 remained. Thus, 9.8% (144/1,468) of all consecutive new outpatients refused participation, and 23.5% (144/614) of those eligible for telephone screening refused. The demography of the refusers was not significantly different from the nonrefusers. The 308 subjects who were not excluded were scheduled for in-person baseline assessment. During baseline evaluation, 134 cases did not fit inclusion criteria and thus were excluded, leaving the 174 cases that were entered. Thus, 6.3% (93/1,468) of consecutive new cases fit the PEA-BP category.
The CC group was ascertained from a random survey that matched the normal CC group to the PEA-BP subjects by age, gender, SES, ethnicity, and zip code.
Assessment instruments
The Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS) (Geller et al. 1996, 1998d, 2001b) is a semistructured interview that was administered by experienced research clinicians to mothers about their children and to children about themselves. It was developed from the KSADS (Puig-Antich and Ryan 1986) by adding items to assess the lifetime and current onset and offset of each symptom and syndrome, items to assess multiple DSM-IV diagnoses, and items to specifically assess prepubertal and early adolescent manifestations of DSM-IV mania criteria and rapid cycling. Skip-outs were minimized to enhance collection of phenomenology data. The data collection guideline is that the narrative documentation must justify the rating with respect to onset, offset, frequency, duration, intensity, and specific examples (Geller et al. 2001b, 2002). Thus, the narrative next to each WASH-U-KSADS item is part of using this assessment tool (e.g., part of the narrative next to a suicidal ideation item read, “cut her wrists four times with a kitchen knife and wanted to die to escape her sad feelings”). An additional example of part of the narrative documentation was a child who related feeling “high, off the charts high” before “crashing right down.” This example was part of the documentation of a euphoric state. The elation followed by “crashing” to a state of despair was part of the narrative for cycling. Examples of prepubertal mania manifestations, taken from WASH-U-KSADS interviews of children about themselves, in PEA-BP and CC subjects, appeared elsewhere (Geller et al. 2002). In this “examples” article (Geller et al. 2002), comparisons between manifestations of DSM-IV symptoms in prepubertal mania and in manic adults were also provided. To score the WASH-U-KSADS items, mother and child responses were combined by using either, in accordance with the methods described by Bird et al. (1992). Excellent reliability (Geller et al. 2001b), stability of mania items and mania diagnoses at 6 months (Geller et al. 2000c), and validity against parent and teacher reports has been shown (Geller et al. 1998d). In addition, this instrument is used in the large majority of NIMH-funded child bipolar disorder studies so that comparable data across studies can be facilitated (NIMH Roundtable 2001). Templates to the WASH-U-KSADS to assess DSM-IV substance use disorders in childhood were also given (Geller et al. 1998a, 1998b).
Overlapping time periods on the WASH-U-KSADS items of mania/hypomania and MDD were used as the definition of “mixed mania.” The definition of rapid cycling was four episodes per year. Ultrarapid cycling was defined as 5–364 and ultradian (continuous) as ≥365 episodes per year. In ultradian cycling, mania needed to occur for ≥4 hours per day (Geller et al. 1995, 1998c, 1998d, 2000b, 2001a). These definitions were adapted from Kramlinger and Post (1996).
The CGAS (Bird et al. 1987; Shaffer et al. 1983) is a global measure of severity based on psychiatric symptomatology and impairment of adaptation in family, social, school, and work areas. It was derived by raters who performed the WASH-U-KSADS. SES was established by the Hollingshead Four Point Index (Hollingshead 1976). The Pubertal Status Questionnaire (Duke et al. 1980) was completed by subjects ≥10 years old at baseline. Medical records were also obtained. Teacher ratings were obtained as previously described (Geller et al. 1998d).
To establish DSM-IV consensus diagnoses, all research materials (assessment instruments, school reports, agency records, pediatrician charts, and videotapes of WASH-U-KSADS interviews of mothers and separate WASH-U-KSADS interview videotapes of children) were reviewed in consensus conferences. These conferences included Dr. Geller and the research nurses who performed the ratings (Fennig et al. 1994; Klein et al. 1994; Kraemer, 1992). At these meetings, narrative documentation for each WASH-U-KSADS item was reviewed to ensure that the rating was justified.
As detailed elsewhere, raters were trained to interrater reliability and recalibrated annually (Geller et al. 2001b). At baseline, raters were blind to group status of the subjects.
After complete description of the study to parents and children, written informed consent was obtained from parents and written assent was obtained from children.
Data analyses
Chi-square and analysis of variance were used for the comparisons of characteristics in Table 1. Logistic regression was used for the between-groups comparisons of symptoms noted in Tables 2–5. Between-group comparisons of symptoms in Tables 2–5 were controlled for age and gender in the logistic regression analyses due to the significant differences between these variables in the ADHD compared to the PEA-BP and CC groups (see Table 1). It was decided not to force age, puberty, and gender matches between the PEA-BP and ADHD groups, because that would have produced a highly skewed, nonrepresentative ADHD group. Because age and puberty were highly correlated (r=0.76, p<0.0001), only age was controlled. Age was selected because it was the more precise measurement. Bonferroni corrections for multiple comparisons in Tables 2–5 were made by dividing p=0.05 by the number of comparisons in each table.
Results
Characteristics of the study sample
Table 1 presents a comparison of characteristics of the PEA-BP, ADHD, and CC groups. As noted in the Data Analyses section, it was decided not to force age, puberty, and gender matches between the PEA-BP and ADHD groups, because that would have produced a highly skewed, nonrepresentative ADHD group. These differences were controlled for in the statistical analyses. Consistent with the ascertainment schema, the PEA-BP and CC groups were excellently matched and not significantly different on any characteristic.
Comparisons of DSM-IV mania symptoms
Table 2 and Fig. 1 show the comparisons for four of the five symptoms (elated mood, grandiosity, decreased need for sleep, flight of ideas/racing thoughts) that provided the best discrimination between the PEA-BP and ADHD groups. These four symptoms and the hypersexuality symptom described below and in Table 3 and Fig. 2 are mania specific (i.e., they are DSM-IV symptoms for mania but are not DSM-IV symptoms for ADHD).
Table 3 and Fig. 2 demonstrate the comparisons for the WASH-U-KSADS symptoms that are used to rate the DSM-IV poor judgment criterion. Although the overall prevalences of the poor judgment criterion were significantly different between PEA-BP and ADHD subjects, poor judgment was a less clinically useful discriminator, because it also occurred in 44.4% of the ADHD group. By contrast, the hypersexuality symptom provided excellent discrimination between the PEA-BP and ADHD subjects.
Table 4 and Fig. 3 present comparisons for DSM-IV symptoms that are included in DSM-IV for both the PEA-BP and ADHD categories. Therefore, these symptoms are not mania specific because they occur in both DSM-IV mania and ADHD categories. In addition, Table 4 and Fig. 3 show the data for irritability. Even though there were statistically significant differences, these nonspecific mania symptoms were poor discriminators, because they were frequent in both the PEA-BP and ADHD groups. This is especially true for the irritability symptom, which occurred in 71.6% of the subjects with ADHD.
Concurrent elation and irritability
Coexisting elated mood and irritability occurred in 87.1% (n=81) of the subjects with PEA-BP.
Suicidality, psychosis, mixed mania, and rapid cycling
Table 5 and Figs. 4 and 5 present the prevalences of psychotic and suicidal symptoms and of mixed mania and rapid cycling course features. Psychosis only included malignant, pathological hallucinations and delusions. For example, hearing a voice call your name was not counted, but hearing a voice telling you to kill yourself was counted. It was previously shown that these items did not differ by age or gender within the PEA-BP group (Geller et al. 2000b). In the PEA-BP group, rapid cycling moods included elation, depression, and irritability. In the ADHD group, the rapid cycling mood was irritability.
Discussion
Data in this article on prevalences of DSM-IV symptoms in the PEA-BP subjects demonstrated their similarity to prevalences of DSM-IV symptoms reported for manic adults (Goodwin and Jamison 1990). The high prevalence of irritability in the PEA-BP, concurrent with a high prevalence of elated mood, was also similar to data from studies of bipolar adults (Goodwin and Jamison 1990). Thus, these findings support the phenotypic similarity of mania across the age span. The ongoing longitudinal study of the “Phenomenology” sample will address whether this similarity of DSM-IV symptom distribution between PEA-BP subjects and bipolar adults will continue as the PEA-BP group reaches late-teenage and adult years.
Five symptoms (i.e., elation, grandiosity, flight of ideas/racing thoughts, decreased need for sleep, and hypersexuality) provided the best discrimination of PEA-BP subjects from ADHD and CC subjects. These five symptoms are also mania specific in DSM-IV (i.e., they do not overlap with DSM-IV symptoms for ADHD). Irritability, hyperactivity, accelerated speech, and distractibility were very frequent in both PEA-BP and ADHD groups and therefore were not useful for differentiating between these two diagnoses.
Unlike late teenage/adult onset bipolar disorder, even PEA-BP subjects selected for DSM-IV mania with cardinal symptoms have high rates of comorbid DSM-IV ADHD.
The 6.3% rate of PEA-BP found at the pediatric and psychiatric ascertainment sites merits comment. This rate is likely higher than at other pediatric and psychiatric sites because of the following. After the pilot data study (Geller et al. 1995), Washington University in St. Louis became a referral site for children suspected of being bipolar. This referral site “status” most likely accounts for the higher rate at the psychiatric site. The pediatric sites that allowed consecutive new case ascertainment in their offices (e.g., they agreed to send letters to all of their new patients, they allowed the research nurses to review the new charts in their office) were more likely to be referral sites themselves. Because bipolar children may be viewed by their community practitioner gatekeepers as “complicated” ADHD cases, they may have been more likely to be referred to pediatric or child psychiatry sites. Referral of “complicated” ADHD cases to referral centers is consistent with the data of Zarin et al. (1998). Zarin et al. (1998) noted that psychiatrists treated more complicated ADHD patients than did those seen by other practitioners. Stated another way, noncomorbid, less impaired ADHD cases were more likely to be treated by gatekeepers. By contrast, comorbid, more impaired ADHD cases were more likely to be referred to specialists.
Considering mania in the differential diagnosis of children with the symptom hypersexuality, in the absence of sexual abuse or overstimulation, was clearly supported by data in this study and by that from the baseline psychosocial functioning findings from the ongoing “Phenomenology” study (Geller et al. 2000a). In the psychosocial data, only 1.1% of the PEA-BP sample had sexual abuse or overstimulation in the environment. Therefore, the 43.0% rate of hypersexuality in the PEA-BP subjects strongly supports hypersexuality as a symptom of mania.
The rates of mixed mania and of psychosis were somewhat higher than reports from samples of bipolar adults (Goodwin and Jamison 1990). By contrast, the 77.4% rate of continuous, ultradian rapid cycling was markedly higher than the <20% rate reported for bipolar adults (Goodwin and Jamison 1990). A discussion of the prevalence and lack of gender difference in these mixed cycling features in the PEA-BP sample has been previously reported (Geller et al. 2000c, 2001a). As discussed elsewhere, the PEA-BP sample resembles the chronic, mixed/cycling pattern seen in treatment-resistant adult mania (Geller et al. 2000c, 2001a, in press-a; Goodwin and Jamison 1990).
Suicidality occurring only in the PEA-BP group is consistent with the MDD exclusion criterion for the ADHD and CC groups. The high rate of suicidality in the PEA-BP subjects, who were only aged 10.9 years (SD=2.6 years), emphasizes the need for identification of childhood mania and for intervention research.
Limitations
Due to public health policies in effect at the time of subject enrollment, there were no low-SES sites available. Therefore, the findings from this high-SES sample may not generalize to lower SES groups. Also, findings from the PEA-BP group may not generalize to other child mania phenotypes discussed in the NIMH Roundtable (2001).
| PEA-BP | ADHD | CC | BP vs. ADHD vs. CC | BP vs. ADHD | BP vs. CC | ADHD vs. CC | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Mean | SD | Mean | SD | Mean | SD | F | p | t | p | t | p | t | p | |
| Baseline age | 10.9 | 2.6 | 9.7 | 2.0 | 11.0 | 2.6 | 7.5 | 0.0007 | 3.3 | 0.0012 | 0.5 | n.s. | 3.9 | 0.0002 | |
| Onset age of current bipolar episode | 7.3 | 3.5 | N/A | N/A | N/A | N/A | — | — | — | — | — | — | |||
| Years of current bipolar episode duration | 3.6 | 2.5 | N/A | N/A | N/A | N/A | — | — | — | — | — | — | |||
| CGAS score | 43.3 | 7.6 | 55.7 | 4.2 | 84.1 | 4.6 | 1237.5 | <0.0001 | 13.5 | <0.0001 | 44.2 | <0.0001 | 42.3 | <0.0001 | |
| % | n | % | n | % | n | χ2 | p | χ2 | p | χ2 | p | χ2 | p | ||
| Pubertal status | |||||||||||||||
| Prepubertal | 57.0 | 53 | 80.2 | 65 | 58.5 | 55 | 12.5 | 0.002 | 10.7 | 0.001 | 0.04 | ns | 9.5 | 0.002 | |
| Pubertal | 43.0 | 40 | 19.8 | 16 | 41.5 | 39 | |||||||||
| Gender | |||||||||||||||
| Male | 61.3 | 57 | 79.0 | 64 | 61.7 | 58 | 7.8 | 0.02 | 6.4 | 0.011 | 0.003 | ns | 6.2 | 0.013 | |
| Female | 38.7 | 36 | 21.0 | 17 | 38.3 | 36 | |||||||||
| Race | |||||||||||||||
| White | 89.2 | 83 | 87.6 | 71 | 90.4 | 85 | 0.3 | ns | 0.1 | ns | 0.1 | ns | 0.3 | ns | |
| Other | 10.8 | 10 | 12.4 | 10 | 9.6 | 9 | |||||||||
| SES class | 2nd highesta | 2nd highesta | 2nd highesta | ||||||||||||
| PEA-BP | ADHD | CC | BP vs. ADHD vs. CC | BP vs. ADHD | BP vs. CC | ADHD vs. CC | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptom | % | n | % | n | % | n | χ2 | p | χ2 | p | χ2 | p | χ2 | p |
| Elated mood | 89.3 | 83 | 13.6 | 11 | 0.0 | 0 | — | — | 64.2 | <0.0001 | — | — | — | — |
| Grandiosity | 86.0 | 80 | 4.9 | 4 | 1.1 | 1 | 85.7 | <0.0001 | 61.0 | <0.0001 | 36.6 | <0.0001 | — | — |
| Flight and/or racing | 71.0 | 66 | 9.9 | 8 | 0.0 | 0 | — | — | 47.0 | <0.0001 | — | — | — | — |
| Flight of ideas | 57.0 | 53 | 8.6 | 7 | 0.0 | 0 | — | — | 32.0 | <0.0001 | — | — | — | — |
| Racing thoughts | 49.5 | 46 | 1.2 | 1 | 0.0 | 0 | — | — | 17.6 | <0.0001 | — | — | — | — |
| Decreased need for sleep | 39.8 | 37 | 6.2 | 5 | 1.1 | 1 | 33.3 | <0.0001 | 19.9 | <0.0001 | 16.0 | <0.0001 | 3.5 | ns |
| PEA-BP | ADHD | CC | BP vs.ADHD vs. CC | BP vs.ADHD | BP vs. CC | ADHD vs. CC | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptom | % | n | % | n | % | n | χ2 | p | χ2 | p | χ2 | p | χ2 | p |
| Poor judgment | 90.3 | 84 | 44.4 | 36 | 3.2 | 3 | 74.3 | <0.0001 | 32.2 | <0.0001 | 65.1 | <0.0001 | 23.9 | <0.0001 |
| Hypersexuality | 43.0 | 40 | 6.2 | 5 | 0.0 | 0 | — | — | 20.8 | <0.0001 | — | — | — | — |
| Daredevil acts | 65.6 | 61 | 11.1 | 9 | 0.0 | 0 | — | — | 38.5 | <0.0001 | — | — | — | — |
| Silliness, laughing | 63.4 | 59 | 23.5 | 19 | 0.0 | 0 | — | — | 26.8 | <0.0001 | — | — | — | — |
| Uninhibited people seeking | 65.6 | 61 | 24.7 | 20 | 3.2 | 3 | 55.1 | <0.0001 | 22.7 | <0.0001 | 42.4 | <0.0001 | 11.8 | 0.0006 |
| PEA-BP | ADHD | CC | BP vs. ADHD vs. CC | BP vs. ADHD | BP vs. CC | ADHD vs. CC | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptom | % | n | % | n | % | n | χ2 | p | χ2 | p | χ2 | p | χ2 | p |
| Irritable mood | 97.9 | 91 | 71.6 | 58 | 3.2 | 3 | 68.0 | <0.0001 | 13.6 | 0.0002 | 45.7 | <0.0001 | 42.8 | <0.0001 |
| Accelerated speech | 96.8 | 90 | 81.5 | 66 | 11.7 | 11 | 84.8 | <0.0001 | 6.7 | ns | 62.9 | <0.0001 | 56.7 | <0.0001 |
| Distractibility | 93.6 | 87 | 96.3 | 78 | 2.1 | 2 | 64.8 | <0.0001 | 0.2 | ns | 40.0 | <0.0001 | 45.8 | <0.0001 |
| Increased energy | 100.0 | 93 | 95.1 | 77 | 11.7 | 11 | — | — | — | — | — | — | 62.6 | <0.0001 |
| Hyperenergetic | 94.6 | 88 | 88.9 | 72 | 6.4 | 6 | 97.3 | <0.0001 | 3.1 | ns | 53.8 | <0.0001 | 65.8 | <0.0001 |
| Increased productivity | 33.3 | 31 | 11.1 | 9 | 0.0 | 0 | — | — | 9.7 | ns | — | — | — | — |
| Sharpened thinking | 49.5 | 46 | 19.8 | 16 | 3.2 | 3 | 37.2 | <0.0001 | 13.5 | 0.0002 | 30.0 | <0.0001 | 11.0 | 0.0009 |
| Increased goal directed | 46.2 | 43 | 18.5 | 15 | 1.1 | 1 | 29.6 | <0.0001 | 14.8 | 0.0001 | 18.6 | <0.0001 | 8.5 | ns |
| PEA-BP | ADHD | CC | BP vs. ADHD vs. CC | BP vs. ADHD | BP vs. CC | ADHD vs. CC | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Feature | % | n | % | n | % | n | χ2 | p | χ2 | p | χ2 | p | χ2 | p |
| Suicidality | 24.7 | 23 | 0.0 | 0 | 0.0 | 0 | — | — | — | — | — | — | — | — |
| Total psychosis | 60.2 | 56 | 0.0 | 0 | 0.0 | 0 | — | — | — | — | — | — | — | — |
| Grandiose delusions | 50.5 | 47 | 0.0 | 0 | 0.0 | 0 | — | — | — | — | — | — | — | — |
| Mixed mania | 54.8 | 51 | 0.0 | 0 | 0.0 | 0 | — | — | — | — | — | — | — | — |
| Total rapid cycling | 87.1 | 81 | 8.6 | 7 | 0.0 | 0 | — | — | 66.1 | <0.0001 | — | — | — | — |
| Cycles/year | ||||||||||||||
| 4 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | — | — | — | — | — | — | — | — |
| 5–364 (ultrarapid) | 9.7 | 9 | 2.5 | 2 | 0.0 | 0 | — | — | 0.9 | ns | — | — | — | — |
| ≥365 (ultradian) | 77.4 | 72 | 6.2 | 5 | 0.0 | 0 | — | — | 55.1 | <0.0001 | — | — | — | — |
| PEA-BP | ADHD | CC | BP vs. ADHD vs. CC | BP vs. ADHD | BP vs. CC | ADHD vs. CC | ||||||||
| Feature | Mean | SD | Mean | SD | Mean | SD | F | p | t | p | t | p | t | p |
| Ultradian cycles/day | 3.7 | 2.1 | 3.0 | 1.8 | 0 | 0.0 | — | — | 8.1 | ns | — | — | — | — |
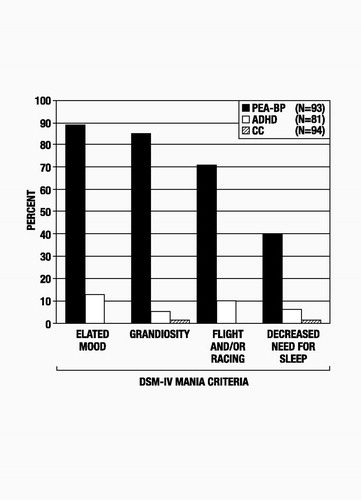
Figure 1. Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) mania-specific symptoms in 93 PEA-BP, 81 ADHD, and 94 CC subjects. Comparisons between groups appear in Table 2. ADHD=attention deficit hyperactivity disorder; CC=normal community controls; PEA-BP=prepubertal and early adolescent bipolar disorder phenotype.
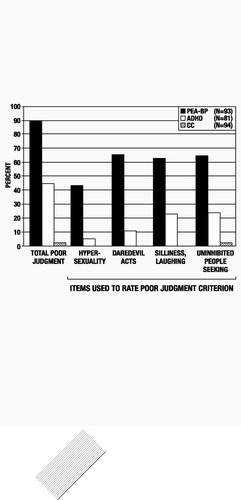
Figure 2. DSM-IV mania poor judgment symptoms in 93 PEA-BP, 81 ADHD, and 94 CC subjects. Comparisons between groups appear in Table 3. Abbreviations are as in Fig. 1.
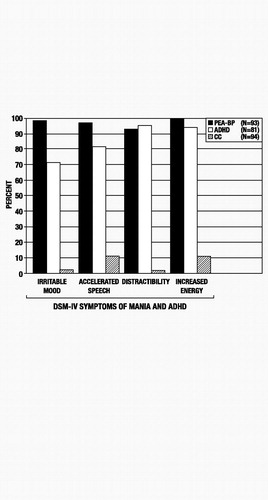
Figure 3. DSM-IV mania nonspecific symptoms in 93 PEA-BP, 81 ADHD, and 94 CC subjects. Comparisons between groups appear in Table 4. Abbreviations are as in Fig. 1.
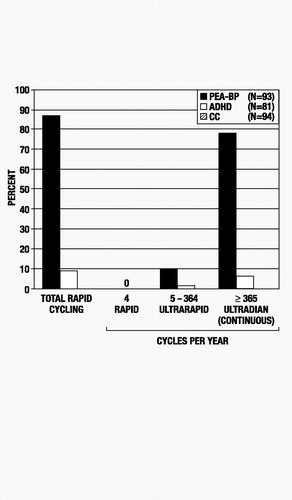
Figure 4. PEA-BP subjects with rapid cycling, ultrarapid cycling, and continuous rapid (ultradian) cycling. Comparisons of cycling patterns between PEA-BP, ADHD, and CC groups appear in Table 5. Abbreviations are as in Fig. 1.
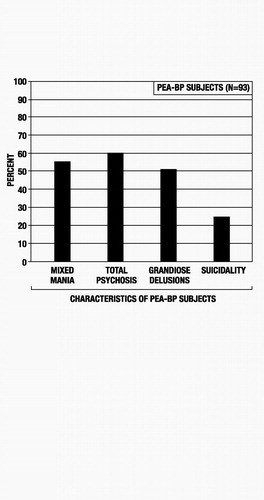
Figure 5. DSM-IV mania features in 93 PEA-BP subjects. Comparisons to ADHD and CC groups appear in Table 5. Abbreviations are as in Fig. 1.
American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM-IV). Washington (DC), American Psychiatric Association, 1994Google Scholar
Bird HR, Canino G, Rubio-Stipec M, Ribera JC: Further measures of the psychometric properties of the Children’s Global Assessment Scale. Arch Gen Psychiatry 44: 821–824, 1987Crossref, Google Scholar
Bird HR, Gould MS, Staghezza B: Aggregating data from multiple informants in child psychiatry epidemiological research J Am Acad Child Adolesc Psychiatry 31:78–85, 1992Crossref, Google Scholar
Duke PM, Litt IF, Gross RT: Adolescents’ self-assessment of sexual maturation. Pediatrics 66: 918–920, 1980Google Scholar
Faraone SV, Biederman J, Mennin D, Wozniak J, Spencer T: Attention-deficit hyperactivity disorder with bipolar disorder: A familial subtype? J Am Acad Child Adolesc Psychiatry 36:1378–1387, 1997Crossref, Google Scholar
Fennig S, Craig TJ, Tanenberg-Karant M, Bromet EJ: Comparison of facility and research diagnoses in first-admission psychotic patients. Am J Psychiatry 151: 1423–1429, 1994Crossref, Google Scholar
Fristad MA, Weller EB, Weller RA: The Mania Rating Scale: Can it be used in children? A preliminary report. J Am Acad Child Adolesc Psychiatry 31: 252–257, 1992Crossref, Google Scholar
Geller B, Sun K, Zimerman B, Luby J, Frazier J, Williams M: Complex and rapid-cycling in bipolar children and adolescents: A preliminary study. J Affect Disord 34: 259–268, 1995Crossref, Google Scholar
Geller B, Williams M, Zimerman B, Frazier J: Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS). St. Louis, Washington University, 1996Google Scholar
Geller B, Cooper TB, Sun K, Zimerman B, Frazier J, Williams M, Heath J: Double-blind and placebo-controlled study of lithium for adolescent bipolar disorders with secondary substance dependency. J Am Acad Child Adolesc Psychiatry 37: 171–178, 1998aCrossref, Google Scholar
Geller B, Cooper TB, Zimerman B, Frazier J, Williams M, Heath J, Warner K: Lithium for prepubertal depressed children with family history predictors of future bipolarity: A double-blind, placebo-controlled study. J Affect Disord 51: 165–175, 1998bCrossref, Google Scholar
Geller B, Warner K, Williams M, Zimerman B: Prepubertal and young adolescent bipolarity versus ADHD: Assessment and validity using the WASH-U-KSADS, CBCL and TRF. J Affect Disord 51: 93–100, 1998cCrossref, Google Scholar
Geller B, Williams M, Zimerman B, Frazier J, Beringer L, Warner KL: Prepubertal and early adolescent bipolarity differentiate from ADHD by manic symptoms, grandiose delusions, ultrarapid or ultradian cycling. J Affect Disord 51: 81–91, 1998dCrossref, Google Scholar
Geller B, Bolhofner K, Craney JL, Williams M, DelBello MP, Gundersen K: Psychosocial functioning in a prepubertal and early adolescent bipolar disorder phenotype. J Am Acad Child Adolesc Psychiatry 39: 1543–1548, 2000aCrossref, Google Scholar
Geller B, Zimerman B, Williams M, Bolhofner K, Craney JL, DelBello MP, Soutullo CA: Diagnostic characteristics of 93 cases of a prepubertal and early adolescent bipolar disorder phenotype by gender, puberty and comorbid ADHD. J Child Adolesc Psychopharmacol 10: 157–164, 2000bCrossref, Google Scholar
Geller B, Zimerman B, Williams M, Bolhofner K, Craney JL, DelBello MP, Soutullo CA: Six-month stability and outcome of a prepubertal and early adolescent bipolar disorder phenotype. J Child Adolesc Psychopharmacol 10: 165–173, 2000cCrossref, Google Scholar
Geller B, Craney JL, Bolhofner K, DelBello MP, Williams M, Zimerman B: One-year recovery and relapse rates of children with a prepubertal and early adolescent bipolar disorder phenotype. Am J Psychiatry 158: 303–305, 2001aCrossref, Google Scholar
Geller B, Zimerman B, Williams M, Bolhofner K, Craney JL, DelBello M, Soutullo C: Reliability of the Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS) mania and rapid cycling sections. J Am Acad Child Adolesc Psychiatry 40: 450–455, 2001bCrossref, Google Scholar
Geller B, Craney JL, Bolhofner K, Nickelsburg MJ, Williams M, Zimerman B: Two year prospective follow-up of children with a prepubertal and early adolescent bipolar disorder phenotype. Am J Psychiatry (in press)Google Scholar
Geller B, Zimerman B, Williams M, DelBello MP, FrazierJ, Beringer L: Phenomenology of prepubertal and early adolescent bipolar disorder: Examples of elated mood, grandiose behaviors, decreased need for sleep, racing thoughts and hypersexuality. J Child Adolesc Psychopharmacol 12: 3–10, 2002Crossref, Google Scholar
Gershon ES, Hamovit J, Guroff JJ, Dibble E, Leckman JF, Sceery W, Targum SD, Nurnberger JI, Goldin LR, Bunney WE. A family study of schizoaffective, bipolar I, bipolar II, unipolar, and normal control probands. Arch Gen Psychiatry 39: 1157–1167, 1982Crossref, Google Scholar
Goodwin FK, Jamison KR (eds): Manic-Depressive Illness. New York, Oxford University Press, 1990Google Scholar
Hollingshead AB: Four Factor Index of Social Status. New Haven, (Connecticut), Yale University, 1976Google Scholar
Horowitz HA: The use of lithium in the treatment of the drug-induced psychotic reaction. Dis Nerv Syst 36: 159–163, 1975Google Scholar
Horowitz HA: Lithium and the treatment of adolescent manic depressive illness. Dis Nerv Syst 38: 480–483, 1977Google Scholar
Klein DN, Ouimette PC, Kelly HS, Ferro T, Riso LP: Test-retest reliability of team consensus best-estimate diagnoses of axis I and II disorders in a family study. Am J Psychiatry 151: 1043–1047, 1994Crossref, Google Scholar
Kraemer HC: How many raters? Toward the most reliable diagnostic consensus. Stat Med 11: 317–331, 1992Crossref, Google Scholar
Kramlinger KG, Post R: Ultra-rapid and ultradian cycling in affective illness. Br J Psychiatry 168: 314–323, 1996Crossref, Google Scholar
National Institute of Mental Health research roundtable on prepubertal bipolar disorder. J Am Acad Child Adolesc Psychiatry 40: 871–878, 2001Crossref, Google Scholar
Puig-Antich J, Ryan N: The Schedule for Affective Disorders and Schizophrenia for School-age Children (Kiddie-SADS) 1986. Pittsburgh, Western Psychiatric Institute and Clinic, 1986Google Scholar
Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S: A Children’s Global Assessment Scale (CGAS) Arch Gen Psychiatry 40:1228–1231, 1983Crossref, Google Scholar
Zarin DA, Suarez AP, Pincus HA, Kupersanin E, Zito JM. Clinical and treatment characteristics of children with attention-deficit/hyperactivity disorder in psychiatric practice. J Am Acad Child Adolesc Psychiatry 37: 1262–1270, 1998Crossref, Google Scholar



