Antipsychotic Use in Children and Adolescents: Minimizing Adverse Effects to Maximize Outcomes
Abstract
(Reprinted with permission from the Journal of the American Academy of Child and Adolescent Psychiatry 2008; 47(1):9–20)
In children and adolescents, antipsychotics are being used in large and increasing quantities for a wide range of disorders and psychopathology, including psychotic, mood, and disruptive behavior disorders (1). Moreover, antipsychotics are also being used in children and adolescents to treat irritability associated with autism, tic disorders, obsessive-compulsive disorder, posttraumatic stress disorder and aggression; (2–4) however, the widespread use exceeds the database regarding efficacy as well as safety and tolerability in this population. At the time of this writing, only three antipsychotics—haloperidol, thioridazine, and risperidone—have been approved for use in children and adolescents by the U.S. Food and Drug Administration, with most randomized controlled data being available for risperidone. To appropriately use this potent class of medications, clinicians need to actively weigh the potential risks and benefits of individual agents. The present article aims to succinctly review available data on antipsychotic-related adverse effects in children and adolescents and provide a practical guide for the evaluation and management of antipsychotic-related adverse effects in this vulnerable population.
Receptor pharmacology predicts clinical effects
Antipsychotic agents differ in their effects on brain neuroreceptor systems (Table 1). Although still limited, current knowledge links therapeutic and adverse effects of antipsychotics to their different effects on dopaminergic, noradrenergic, serotonergic, histaminergic, and cholinergic receptors, among others (Table 2). Recently, the presence of withdrawal or rebound phenomena has also been recognized (Table 2), which can result from a too-rapid transition from antipsychotics with substantial anticholinergic or antihistaminergic effects (e.g., clozapine, olanzapine, quetiapine) to agents with minimal cholinergic or histaminergic blockade, (e.g., aripiprazole, ziprasidone). In addition to pharmacodynamic differences, therapeutic and adverse effects can vary substantially depending on differences in antipsychotic absorption, half-life, dose, and interindividual susceptibility that is usually unknown until a specific medication trial is undertaken. For example, dopamine rebound/ withdrawal syndromes (Table 2) can occur during a switch when the first antipsychotic drug achieved a comparatively high dopamine blockade and is then switched too abruptly to an antipsychotic that achieves a considerably lower dopamine blockade. This can occur when the second antipsychotic is dosed much lower during the initial titration process, has a longer relative half-life, thus taking longer to reach the equivalent blood level (e.g., aripiprazole), or because the absorption is dependent on food and the antipsychotic is taken without food (e.g., ziprasidone). To avoid rebound/withdrawal phenomena under these circumstances, the initial antipsychotic should not be discontinued abruptly, and crosstitration or (even better) overlapping switch strategies should be used (5).
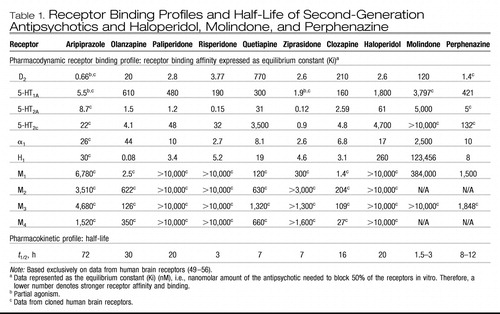 |
Table 1. Receptor Binding Profiles and Half-Life of Second-Generation Antipsychotics and Haloperidol, Molindone, and Perphenazine
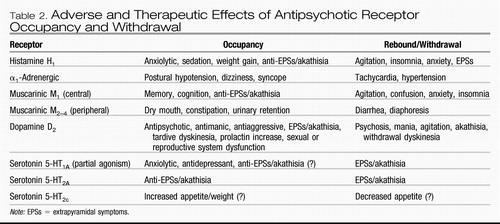 |
Table 2. Adverse and Therapeutic Effects of Antipsychotic Receptor Occupancy and Withdrawal
Table 3 summarizes the time course, dose/titration dependency, and general side effect propensities across the seven second-generation antipsychotics (SGAs) available in the United States and haloperidol as examples of a high-potency, first-generation antipsychotics (FGAs), as well as perphenazine and molindone as examples of mid-potency FGAs that were used in recent large-scale, randomized trials in adults and adolescents, respectively. Because, unfortunately, antipsychotic therapeutic and adverse effect data in children and adolescents are still sparse, much of the safety information in Table 3 is extrapolated from adult data. However, as children and adolescents receiving antipsychotics are also experiencing enormous physical and psychological maturation, it is not surprising that therapeutic and adverse effects can differ between pediatric and adult populations.
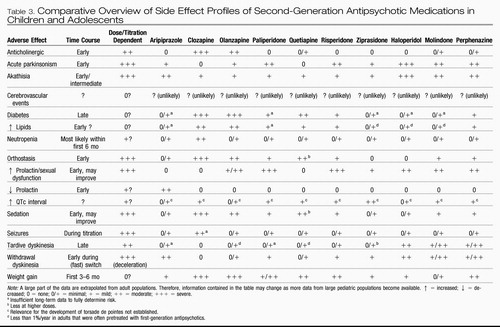 |
Table 3. Comparative Overview of Side Effect Profiles of Second-Generation Antipsychotic Medications in Children and Adolescents
NEUROMOTOR ADVERSE EFFECTS
EXTRAPYRAMIDAL SIDE EFFECTS
In general, children and adolescents are more likely to experience extrapyramidal side effects (EPSs; i.e., parkinsonian side effects and dystonia) associated with FGAs and SGAs than adults (6). To date, only one double-blind, randomized pediatric study directly compared EPS rates with an FGA (i.e., haloperidol; mean dose 5.0 mg/day) and SGAs (i.e., risperidone, mean dose 4.0 mg/day, and olanzapine, mean dose 12.3 mg/day) (7). Results of substantial EPSs not only with haloperidol (67%) but also with olanzapine (56%) and risperidone (53%) suggest that children and adolescents are at risk for EPSs, even when treated with SGAs, at least at doses required to control psychosis. Although overall EPS rates were not significantly different in this study (n = 40), the severity was greater with haloperidol, indicating that reporting global incidence rates are insufficient to guide clinical treatment. In several short-term, double-blind, placebo-controlled trials, risperidone was associated with EPS rates between 8% and 26% (8–11). In four open-label extension trials lasting 11 to 36 months, EPS rates ranged from 8.6% to 26.0% (mean 15.7%) (12). Although in these trials, rating scale-measured EPS severity generally did not increase, EPS rates could be underestimates because they are based on spontaneous reports of mostly prepubertal individuals with autism spectrum disorder treated with relatively modest mean risperidone doses (1–2 mg/day). As in adults, clozapine (13, 14) and quetiapine (15) appear to be associated with relatively low EPS rates in pediatric patients, whereas more data are needed for ziprasidone and aripiprazole. In one recently presented double-blind, placebo-controlled study of aripiprazole in adolescents with schizophrenia, EPSs occurred in 18% of patients (16). Of note, due to complementary actions of dopamine and serotonin regarding EPSs, concurrent treatment with serotonin reuptake inhibitors may trigger or aggravate EPSs. Treatment options are listed in Table 4.
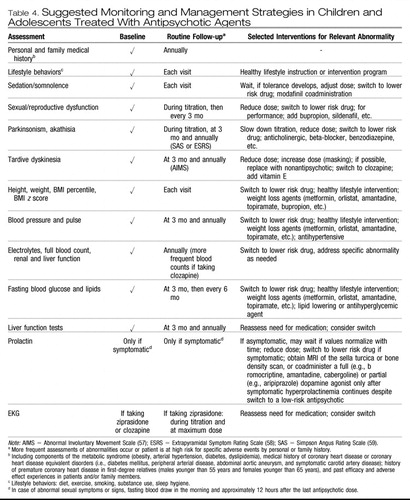 |
Table 4. Suggested Monitoring and Management Strategies in Children and Adolescents Treated With Antipsychotic Agents
Akathisia. In children and adolescents, less is known regarding the risk for akathisia, which has been substantial with FGAs across age groups. In general, it can be difficult to properly diagnose akathisia because the presentation overlaps with psychomotor agitation due to psychosis, mania, and anxiety. In children and adolescents, akathisia may present as difficulty falling asleep and can be mistaken for attention-deficit/ hyperactivity disorder. In one study (7), olanzapine was associated with akathisia in 12.5% of pediatric patients. Aripiprazole, the only available antipsychotic with partial dopamine D2 agonism, has been associated with akathisia in adults. In one retrospective chart review of 30 children and adolescents (mean age 13.3 years, range 5–19), akathisia was recorded in as many as 23% of patients taking aripiprazole (17). However, the mean starting dose of 9 ± 4 mg in this sample was relatively high and almost identical to the mean final dose of 10 ± 3 mg. Furthermore, it is unclear whether abrupt switches could also have increased the akathisia rate via withdrawal/rebound phenomena (Table 2). In a large randomized placebo-controlled study of more than 300 patients, aripiprazole dosed at 10 or 30 mg/day was associated with akathisia in <10% of adolescents with schizophrenia, but patients were titrated from a starting dose of 2 mg/day, reaching the maximum dose at day 5 or 13, respectively (16). This suggests that slower titration of a partial agonist may reduce the rate of akathisia in some patients. As for parkinsonian adverse effects, concurrent use of serotonin reuptake inhibitors can also trigger or aggravate akathisia. Treatment options are listed in Table 4.
Withdrawal Dyskinesia. During treatment with FGAs, children and adolescents seem to be at risk for developing withdrawal dyskinesias, yet, different from adults, these are frequently reversible (18). Rates of withdrawal dyskinesia appear to be lower with SGAs compared with FGAs (19), although a switch from an antipsychotic with strong D2 affinity (e.g., risperidone, aripiprazole) to one with less potent affinity (e.g., quetiapine) may predispose to withdrawal dyskinesia. In one study (20), 2 of 13 children (15.4%) developed mild, reversible withdrawal dyskinesia after 7 months of risperidone treatment. In another, more recent study, however, 0 of 38 patients developed withdrawal dyskinesia after risperidone (mean dose 2 mg/day) was discontinued after 4 months of treatment (21). The risk for withdrawal dyskinesia can be reduced with slow cross-titration and overlapping cross-titration (5).
Tardive Dyskinesia (TD). A recent meta-analysis of 10 studies lasting at least 11 months reported on TD rates in 783 pediatric patients ages 4 to 18 (weighted mean 9.8) years old (12). Most patients were prepubertal (79.2%), male (81.7%), and white (78.4%). Across these studies, only three cases of TD were reported, resulting in an annualized incidence rate of 0.4%. Although this pediatric rate is approximately half the risk found in another meta-analysis of 1,964 nonelderly adults, (22) firm conclusions are precluded by the facts that none of the pediatric studies were designed specifically to detect TD, antipsychotic doses were low, and lifetime exposure was relatively short.
NEUROLEPTIC MALIGNANT SYNDROME
Neuroleptic malignant syndrome (NMS) is a rare but potentially fatal medical emergency that can result from antipsychotic treatment. The clinical picture consists of severe (“lead pipe”) rigidity, tachycardia, fever, arterial hyper- or hypotension, elevated creatinine phosphokinase, and elevated white cell count. It has been suggested that SGAs may be associated less with NMS than FGAs and that SGAs are associated with a more benign course of NMS (23), but this is unclear. In children and adolescents, several cases of NMS have been reported, even with SGAs. Thus, clinicians should be vigilant and rule out NMS in antipsychotic-treated children and adolescents presenting with fever, tachycardia, and rigidity.
WEIGHT GAIN AND METABOLIC ADVERSE EFFECTS
Although pediatric data are largely missing and the effects of illness versus treatment history are unclear, children and adolescents with psychiatric disorders seem to be at increased risk for being overweight/obese (24). Age-inappropriate weight gain is of particular concern in children and adolescents due to its association with glucose and lipid abnormalities and cardiovascular morbidity/ mortality (25). Reasons for weight gain are likely complex, including psychiatric illness, unhealthy lifestyle, and the treatment used. A recent review of pediatric data suggested that the weight gain potential of SGAs follows roughly the same ranking order as found in adults (Table 3), but that the magnitude is greater (26). Exceptions may be a greater relative weight gain propensity of risperidone (27), and a greater likelihood of aripiprazole and ziprasidone to not be weight neutral in subgroups of pediatric patients (26). Of note, combined SGA treatment with a stimulant does not seem to substantially attenuate SGA-induced weight gain (28), whereas combined treatment with a mood stabilizer or combination treatment seems associated with more weight gain than monotherapy with mood stabilizers and may lead to greater weight gain than treatment with just one SGA (29).
Although in adults the link between antipsychotic treatment and adverse metabolic consequences, such as dyslipidemia, hyperglycemia, diabetes, and the metabolic syndrome, has been established (25), the few published pediatric studies (7, 30, 31) have produced conflicting results. However, interpretation of these data is limited by the small sample size, varying treatment histories, and inclusion of random glucose assessments. Case reports of new-onset diabetes in antipsychotic-treated children and adolescents (26) and the established link between weight gain and metabolic abnormalities suggest that children and adolescents are at least as liable to develop metabolic abnormalities as adults, which is suggested also by an ongoing prospective pediatric safety study (26).
PROLACTIN-RELATED SIDE EFFECTS
As recently summarized, (26) FGAs and SGAs can elevate prolactin levels, but other reasons for hyperprolactinemia need to be ruled out, including hyperthyroidism, renal failure, pregnancy, or oral contraception. Hyperprolactinemia can result in sexual side effects, such as amenorrhea and oligomenorrhea, erectile dysfunction, decreased libido, and hirsutism, and breast symptoms, such as enlargement, engorgement, pain, and galactorrhea, although prolactin levels are not closely correlated with these symptoms. Available data also suggest that hyperprolactinemia is dose dependent, seems to normalize over time, and resolves after antipsychotic discontinuation. Similar to adults, albeit at higher levels during adolescence, the relative potency of antipsychotic drugs in inducing hyperprolactinemia is roughly as follows: risperidone/paliperidone > haloperidol > olanzapine > ziprasidone > quetiapine > clozapine > aripiprazole. Aripiprazole may lower prolactin below baseline values, with low endpoint levels being most likely in boys and prepubertal individuals who have low baseline values. Whether hyperprolactinemia at the levels found in response to antipsychotics alters bone density, sexual maturation, or the risk for breast cancer or benign prolactinomas during periods of critical maturation is unclear, partly because data are largely based on prepubertal boys treated with risperidone, lacking enough peripubertal patients followed for sufficient periods of time (26).
Due to the lack of evidence for the physiological risks of asymptomatic, subclinical prolactin elevations, current guidelines do not suggest routine prolactin monitoring, unless sexual adverse effects are present. Sexual functioning needs to be actively inquired about, but screening is less sensitive in prepubertal individuals and those not sexually active. Because prolactin levels vary during the day and can be elevated by food, exercise, stress, and medications, blood should be obtained after fasting in the morning and before medications are taken. In asymptomatic patients with elevated prolactin (usually <100 ng/mL), one may wait to see whether values normalize over time. In overtly symptomatic patients, dose reduction or a switch to a lower risk agent is indicated. Magnetic resonance imaging of the sella turcica to rule out prolactinomas or bone density scans, using dual x-ray absorptiometry, or coadministration of a full (e.g., bromocriptine, amantadine, cabergoline) or partial (e.g., aripiprazole) dopamine agonist are recommended only after symptomatic hyperprolactinemia continues despite a switch to a low-risk antipsychotic.
CARDIAC SIDE EFFECTS
DIZZINESS/ORTHOSTASIS
Antipsychotics with more pronounced α1 blockade (e.g., clozapine, quetiapine) are most likely to lead to usually transient dizziness. This effect is enhanced in patients receiving antihypertensive medications used for hyperactivity (α2 agonists) or for akathisia or tremor (beta-blockers). Slowing the titration and waiting for the adrenergic system to adjust are usually sufficient to deal with this adverse effect. Due to beginning blockade of the α2 autoreceptors at doses at or around 300 mg/day, quetiapine may actually lead to less dizziness and orthostasis at higher than at lower doses.
QTC PROLONGATION
Antipsychotics can differentially prolong the heart rate-corrected QT interval of the electrocardiogram, which may lead to torsade de pointes, a potentially fatal arrhythmia (32). In adults, QTc prolongation is usually minimal compared with placebo, except for thioridazine and droperidol (33). Among SGAs, QTc prolongation to >430 milliseconds has been described in 3 of 20 pediatric patients treated prospectively with ziprasidone (mean QTc prolongation of 28 ± 26 milliseconds), without relationship to ziprasidone dose (32). However, in an earlier albeit smaller study, no significant increase was found (34), and the clinical relevance of this degree of QTc prolongation is unclear. In adults, SGAs, especially those with marked anticholinergic activity, have been noted to affect heart rate variability (35), but the clinical significance of this for pediatric patients is unclear.
MYOCARDITIS
Among the SGAs, only clozapine has been associated with a relevant risk for myocarditis, which is most prominent early on in treatment, but even in children and adolescents, the incidence seems relatively low (36).
MISCELLANEOUS ADVERSE EFFECTS
SEDATION/SOMNOLENCE
Sedation/somnolence are frequent and often impairing side effects of antipsychotics that usually are dose dependent, although tolerance may develop over time in many patients. Similar to orthostasis, an exception to the dose-dependent nature of sedation may be quetiapine, which seems to be less sedating at doses ≥300 mg/day where α2 blockade sets in. Although limited by the mixture of studies with different populations, doses, and methodologies, a recent comparison of adult U.S. Food and Drug Administration labeling trials with pediatric data suggested a similar rank order for the propensity to lead to sedation, but overall increased rates in children and adolescents compared with adults (6). In the reviewed pediatric studies, sedation rates ranged from 0% to 33% for aripiprazole, 42% to 69% for ziprasidone, 25% to 80% for quetiapine, 29% to 89% for risperidone, and 44% to 94% for olanzapine and 46% to 90% with clozapine. In randomized controlled and open-label extension studies with risperidone, somnolence was spontaneously reported in 12% to 61% of patients taking risperidone and 10% to 13% taking placebo (9, 28, 37–39). In studies following patients who had tolerated and benefited from acute treatment, somnolence rates dropped as low as 6% and 1.7% (37). Of note, patients with autism spectrum disorders cotreated with psychostimulants had lower rates of somnolence than those treated with risperidone monotherapy (37% versus 51%) (28).
LIVER TOXICITY
Increased liver enzymes have been reported with antipsychotics in several pediatric studies (7, 40). Although the extent and significance of liver toxicity are unclear, the combination of divalproex with antipsychotics, particularly olanzapine, may increase the risk for abnormal liver function and, possibly, pancreatitis or steatohepatitis (fatty infiltration of the liver) (41).
NEUTROPENIA AND AGRANULOCYTOSIS
With the exception of clozapine, the decrease in white blood cell counts is generally not clinically significant with antipsychotics. In a chart review of 172 clozapine-treated pediatric patients (42), the cumulative 1-year probability of an initial adverse hematologic event was 16.1% (neutropenia: n = 23, 13%; agranulocytosis: n = 1, 0.6%). However, 11 (48%) of the 24 children and adolescents with newly emerging neutropenia were successfully rechallenged, and only 8 patients (5%) discontinued clozapine because of agranulocytosis (n = 1) or neutropenia (n = 7). In general, specific monitoring is not required for other antipsychotics, except in patients with low baseline white blood cell counts.
ASSESSMENT AND MONITORING
Adverse effect assessment and monitoring in pediatric patients must be proactive. Suggested baseline and followup assessments and intervals, as well as management strategies for adverse effects, are detailed in Table 4. Before adding another medication to counter side effects of the antipsychotic, which may have additional adverse effects and lead to drug-drug interactions, prescribers should reevaluate the need for the antipsychotic and consider dose reduction or a switch to a lower risk medication. It is important to note that in growing individuals, the assessment of a number of physical and laboratory measures needed to gauge the level of adverse effects requires taking into consideration developmental norms that incorporate age- and sex-specific thresholds as listed in Tables 5 and 6.
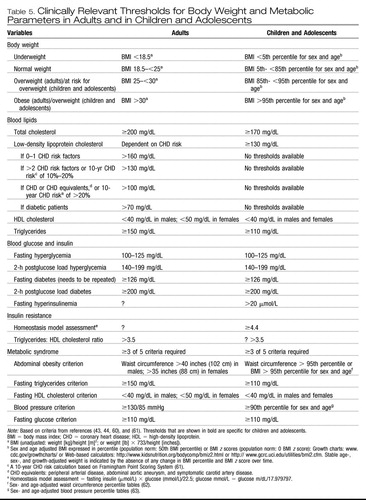 |
Table 5. Clinically Relevant Thresholds for Body Weight and Metabolic Parameters in Adults and in Children and Adolescents
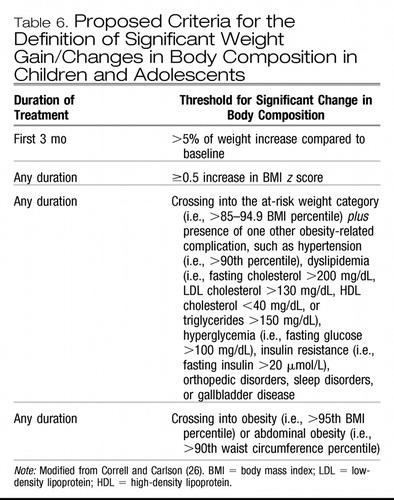 |
Table 6. Proposed Criteria for the Definition of Significant Weight Gain/Changes in Body Composition in Children and Adolescents
Although it can be difficult to obtain fasting blood values, every attempt should be made to accommodate the patient's schedule to facilitate the sample collection (e.g., 8-hour daytime fast, using a laboratory close to home/with convenient hours) because particularly glucose, triglyceride, and low-density lipoprotein cholesterol levels are strongly affected by nonfasting status. Only if fasting assessments cannot be obtained, then a 2-hour postprandial blood draw after a large meal can be used as the last resort to potentially identify patients with hyperglycemia (Table 6). To assess the effect of weight gain or antipsychotic treatment on the risk for diabetes, fasting glucose is a highly insensitive marker. Before hyperglycemia develops, the body compensates by increasing insulin levels. If the insulin level required to keep the blood glucose normal is >20 μU/L (i.e., hyperinsulinemia) (43) or the product of fasting glucose and insulin (i.e., homeostasis model assessment: fasting insulin (μmol/L) × glucose (mmol/L)/22.5; glucose mmol/L = glucose m/dL/17.979797) is >4.19 in adolescents, (44) insulin resistance is present. Although the homeostasis model assessment is the most sensitive noninvasive marker of insulin resistance, insulin levels are not widely obtained. A relatively crude but simple proxy measure for insulin resistance, used in adults and not validated in children and adolescents, is the ratio of (≥8-hour) fasting triglycerides/fasting high-density lipoprotein cholesterol. The triglyceride:high-density lipoprotein cholesterol ratio should be <3.5 and can be used for tracking of development/worsening of insulin resistance (26). Hemoglobin A1C is not suggested as a screening test because it is insensitive and should only be used as a long-term monitoring tool in patients with diabetes (45).
MANAGEMENT
Education about adverse effects and healthy lifestyle behaviors should be part of any psychiatric medication prescribing process. Table 7 lists one proposed 12-step program designed to promote healthy behaviors. Because simultaneously initiating all of the following steps is often unrealistic, the first contact should be used to start by identifying the degree to which patients deviate from the suggested behaviors. Next, one or two of the unhealthiest behaviors that can be addressed most easily should be targeted first, followed by others, once initial goals have been achieved.
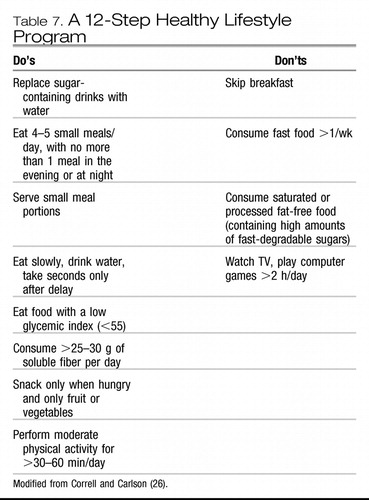 |
Table 7. A 12-Step Healthy Lifestyle Program
In addition to healthy lifestyle instructions, minimizing concerning adverse effects can be achieved most effectively by choosing a lower risk antipsychotic, ideally at the beginning of treatment. Should adverse effects occur, a switch to a lower risk agent, if available, should be considered. Furthermore, the importance of a healthy lifestyle program should be reinforced. Finally, for clinically relevant abnormalities, targeted treatments (Table 4) and/or referrals to specialists for comanagement should be initiated.
SUMMARY
Although more data are needed, children and adolescents seem generally more susceptible to develop sedation, acute EPSs, withdrawal dyskinesia, hyperprolactinemia, and age-inappropriate weight gain with related metabolic abnormalities. Clinicians and researchers should use age-appropriate side effect measures that also take severity and time course of the adverse effects into account to help evaluate and manage more comprehensively antipsychotic risks and benefits in a given individual. Although antipsychotic safety and tolerability data in children and adolescents are limited and most extensive for risperidone, this is likely to change. Several large-scale, randomized, placebo-controlled data sets have either been completed (11, 16, 46–52) or are under way for all nonclozapine SGAs. In addition, a federally funded trial, the Treatment of Early Onset Psychosis Study (48), was recently completed that compared olanzapine, risperidone, and molindone. To counter randomization bias and provide safety and tolerability data in generalizable patient populations and settings, large-scale observational studies will also be helpful. Collectively, safety and efficacy data should inform a carefully weighed antipsychotic selection that takes general probabilities and patient/family preferences into account. Finally, because adverse effects are generally more easily predicted than therapeutic efficacy and because differences in efficacy between antipsychotics are generally smaller than those for adverse effects, initial treatment selection should be guided largely by varying adverse effect profiles across agents.
Disclosure: Dr. Correll has been a consultant to AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Intra-Cellular Therapeutics, Organon, Otsuka, Pfizer, Solvay, Supernus, and Vanda, and has served on the speakers' bureaus/advisory boards of AstraZeneca, Bristol-Myers Squibb, Janssen, Eli Lilly, and Otsuka.
1 Olfson M, Blanco C, Liu L, Moreno C, Laje G. National trends in the outpatient treatment of children and adolescents with antipsychotic drugs. Arch Gen Psychiatry. 2006; 63: 679– 685Crossref, Google Scholar
2 Cheng-Shannon J, McGough JJ, Pataki C, McCracken JT. Second-generation antipsychotic medications in children and adolescents. J Child Adolesc Psychopharmacol. 2004; 14: 372– 394Crossref, Google Scholar
3 Schur SB, Sikich L, Findling RL, et al. Treatment recommendations for the use of antipsychotics for aggressive youth (TRAAY): I. A review. J Am Acad Child Adolesc Psychiatry. 2003; 42: 132– 144Crossref, Google Scholar
4 Pappadopulos E, McIntyre JC II, Crismon ML, et al. Treatment recommendations for the use of antipsychotics for aggressive youth (TRAAY): II. J Am Acad Child Adolesc Psychiatry. 2003; 42: 145– 161Crossref, Google Scholar
5 Correll CU. Real life switching strategies with second-generation antipsychotics. J Clin Psychiatry. 2006; 67: 160– 161Crossref, Google Scholar
6 Correll CU, Penzner JB, Parikh UH, et al. Recognizing and monitoring adverse events of second-generation antipsychotics in children and adolescents. Child Adolesc Psychiatr Clin N Am. 2006; 15: 177– 206Crossref, Google Scholar
7 Sikich L, Hamer RM, Bashford RA, Sheitman BB, Lieberman JA. A pilot study of risperidone, olanzapine, and haloperidol in psychotic youth: a double-blind, randomized, 8-week trial. Neuropsychopharmacology. 2004; 29: 133– 145Crossref, Google Scholar
8 McCracken JT, McGough J, Shah B, et al. Risperidone in children with autism and serious behavioral problems. N Engl J Med. 2002; 347: 314– 321Crossref, Google Scholar
9 Turgay A, Binder C, Snyder R, Fisman S. Long-term safety and efficacy of risperidone for the treatment of disruptive behavior disorders in children with subaverage IQs. Pediatrics. 2002; 110: e34Crossref, Google Scholar
10 Snyder R, Turgay A, Aman M, et al. Effects of risperidone on conduct and disruptive behavior disorders in children with subaverage IQs. J Am Acad Child Adolesc Psychiatry. 2002; 41: 1026– 1036Crossref, Google Scholar
11 Haas M, Unis AS, Copenhaver M, Quiroz J, Kushner S, Kusumakar V. Efficacy and safety of risperidone in adolescents with schizophrenia. Poster presented at the American Psychiatric Association meeting, San Diego, May 19–24, 2007Google Scholar
12 Correll CU, Kane JM. One-year tardive dyskinesia rates in children and adolescents treated with second-generation antipsychotics: a systematic review. J Child Adolesc Psychopharmacol 2007; 17: 647– 655Crossref, Google Scholar
13 Kumra S, Frazier JA, Jacobsen LK, et al. Childhood-onset schizophrenia: a double-blind clozapine-haloperidol comparison. Arch Gen Psychiatry. 1996; 53: 1090– 1097Crossref, Google Scholar
14 Shaw P, Sporn A, Gogtay N, et al. Childhood-onset schizophrenia: a double-blind, randomized clozapine-olanzapine comparison. Arch Gen Psychiatry. 2006; 63: 721– 730Crossref, Google Scholar
15 DelBello MP, Schwiers ML, Rosenberg HL, Strakowski SM. A double-blind, randomized, placebo-controlled study of quetiapine as adjunctive treatment for adolescent mania. J Am Acad Child Adolesc Psychiatry. 2002; 41: 1216– 1223Crossref, Google Scholar
16 Findling RA, Robb AS, Nyilas M, et al. Tolerability of aripiprazole in the treatment of adolescents with schizophrenia. Poster presented at the American Psychiatric Association meeting, San Diego, May 19–24, 2007Google Scholar
17 Barzman DH, DelBello MP, Kowatch RA, et al. The effectiveness and tolerability of aripiprazole for pediatric bipolar disorders: a retrospective chart review. J Child Adolesc Psychopharmacol. 2004; 14: 593– 600Crossref, Google Scholar
18 Campbell M, Armenteros JL, Malone RP, Adams PB, Eisenberg ZW, Overall JE. Neuroleptic-related dyskinesias in autistic children: a prospective, longitudinal study. J Am Acad Child Adolesc Psychiatry. 1997; 36: 835– 843Crossref, Google Scholar
19 Connor DF, Fletcher KE, Wood JS. Neuroleptic-related dyskinesias in children and adolescents. J Clin Psychiatry. 2001; 62: 967– 974Crossref, Google Scholar
20 Malone RP, Maislin G, Choudhury MS, Gifford C, Delaney MA. Risperidone treatment in children and adolescents with autism: short-and long-term safety and effectiveness. J Am Acad Child Adolesc Psychiatry. 2002; 41: 140– 147Crossref, Google Scholar
21 Research Units on Pediatric Psychopharmacology Autism Network. Risperidone treatment of autistic disorder: longer-term benefits and blinded discontinuation after 6 months. Am J Psychiatry. 2005; 162: 1361– 1369Crossref, Google Scholar
22 Correll CU, Leucht S, Kane JM. Lower risk for tardive dyskinesia associated with second-generation antipsychotics: a systematic review of 1-year studies. Am J Psychiatry. 2004; 161: 414– 425Crossref, Google Scholar
23 Ananth J, Parameswaran S, Gunatilake S. Side effects of atypical antipsychotic drugs. Curr Pharm Des. 2004; 10: 2219– 2229Crossref, Google Scholar
24 Patel NC, Hariparsad M, Matias-Akthar M, et al. Body mass indexes and lipid profiles in hospitalized children and adolescents exposed to atypical antipsychotics. J Child Adolesc Psychopharmacol. 2007; 17: 303– 311Crossref, Google Scholar
25 American Diabetes Association, American Psychiatric Association, American Association of Clinical Endocrinologists, North American Association for the Study of Obesity. Consensus development conference on antipsychotic drugs and obesity and diabetes. J Clin Psychiatry. 2004; 65: 267– 272Google Scholar
26 Correll CU, Carlson HE, Endocrine and metabolic adverse effects of psychotropic medications in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2006; 45: 771– 791Crossref, Google Scholar
27 Safer DJ. A comparison of risperidone-induced weight gain across the age span. J Clin Psychopharmacol. 2004; 24: 429– 436Crossref, Google Scholar
28 Aman MG, Binder C, Turgay A. Risperidone effects in the presence/ absence of psychostimulant medicine in children with ADHD, other disruptive behavior disorders, and subaverage IQ. J Child Adolesc Psychopharmacol. 2004; 14: 243– 254Crossref, Google Scholar
29 Correll CU. Weight gain and metabolic effects of mood stabilizers and antipsychotics in pediatric bipolar disorder: a systematic review and pooled analysis of short-term trials. J Am Acad Child Adolesc Psychiatry. 2007; 46: 687– 700Crossref, Google Scholar
30 Biederman J, Mick E, Hammerness P, et al. Open-label, 8-week trial of olanzapine and risperidone for the treatment of bipolar disorder in preschool-age children. Biol Psychiatry. 2005; 58: 589– 594Crossref, Google Scholar
31 Martin A, L'Ecuyer S. Triglyceride, cholesterol and weight changes among risperidone-treated youths. A retrospective study. Eur Child Adolesc Psychiatry. 2002; 11: 129– 133Crossref, Google Scholar
32 Blair J, Scahill L, State M, Martin A. Electrocardiographic changes in children and adolescents treated with ziprasidone: a prospective study. J Am Acad Child Adolesc Psychiatry. 2005; 44: 73– 79Crossref, Google Scholar
33 Glassman AH, Bigger JT Jr. Antipsychotic drugs: prolonged QTc interval, torsade de pointes, and sudden death. Am J Psychiatry. 2001; 158: 1774– 1782Crossref, Google Scholar
34 Sallee FR, Kurlan R, Goetz CG, Singer H, et al. Ziprasidone treatment of children and adolescents with Tourette's syndrome: a pilot study. J Am Acad Child Adolesc Psychiatry. 2000; 39: 292– 299Crossref, Google Scholar
35 Silke B, Campbell C, King DJ. The potential cardiotoxicity of antipsychotic drugs as assessed by heart rate variability. J Psychopharmacol. 2002; 16: 355– 360Crossref, Google Scholar
36 Wehmeier PM, Schuler-Springorum M, Heiser P, Remschmidt H. Chart review for potential features of myocarditis, pericarditis, and cardiomyopathy in children and adolescents treated with clozapine. J Child Adolesc Psychopharmacol. 2004; 14: 267– 271Crossref, Google Scholar
37 Reyes M, Croonenberghs J, Augustyns I, Eerdekens M. Long-term use of risperidone in children with disruptive behavior disorders and subaverage intelligence: efficacy, safety, and tolerability. J Child Adolesc Psychopharmacol. 2006; 16: 260– 272Crossref, Google Scholar
38 Croonenberghs J, Fegert JM, Findling RL, et al. Risperidone in children with disruptive behavior disorders and subaverage intelligence: a 1-year, open-label study of 504 patients. J Am Acad Child Adolesc Psychiatry. 2005; 44: 64– 72Crossref, Google Scholar
39 Aman MG, Arnold LE, McDougle CJ, et al. Acute and long-term safety and tolerability of risperidone in children with autism. J Child Adolesc Psychopharmacol. 2005; 15: 869– 884Crossref, Google Scholar
40 Kumra S, Herion D, Jacobsen LK, Briguglia C, Grothe D. Case study: risperidone-induced hepatotoxicity in pediatric patients. J Am Acad Child Adolesc Psychiatry. 1997; 36: 701– 705Crossref, Google Scholar
41 Gonzalez-Heydrich J, Raches D, Wilens TE, Leichtner A, Mezzacappa E. Retrospective study of hepatic enzyme elevations in children treated with olanzapine, divalproex, and their combination. J Am Acad Child Adolesc Psychiatry. 2003; 42: 1227– 1233Crossref, Google Scholar
42 Gerbino-Rosen G, Roofeh D, Tompkins DA, et al. Hematological adverse events in clozapine-treated children and adolescents. J Am Acad Child Adolesc Psychiatry. 2005; 44: 1024– 1031Crossref, Google Scholar
43 Williams CL, Hayman LL, Daniels SR, et al. Cardiovascular health in childhood: a statement for health professionals from the Committee on Atherosclerosis, Hypertension, and Obesity in the Young (AHOY) of the Council on Cardiovascular Disease in the Young. American Heart Association. Circulation. 2004; 106: 143– 160Crossref, Google Scholar
44 Lee JM, Okumura MJ, Davis MM, Herman WH, Gurney JG. Prevalence and determinants of insulin resistance among US adolescents: a population-based study. Diabetes Care. 2006; 29: 2427– 2432Crossref, Google Scholar
45 Lee TJ, Safranek S. FPIN's clinical inquiries. A1C testing in the diagnosis of diabetes mellitus. Am Fam Physician. 2006; 74: 143– 144Google Scholar
46 Kryzhanovskaya L, Schulz CM, McDougle CJ, et al. Efficacy and safety of olanzapine in adolescents with schizophrenia: results from a double-blind, placebo-controlled trial. Poster presented at the 44th American College of Neuropsychopharmacology Meeting, Waikoloa, HI, December 1–15, 2005Google Scholar
47 Correll CU, Nyilas M, Aurang C, et al. Long term safety and tolerability of aripiprazole in children (10–17 y/o) with bipolar I disorder. Poster presented at the 54th annual meeting of the American Academy of Child and Adolescent Psychiatry, Boston, October 23–28, 2007Google Scholar
48 Robb AJ, Findling RL, Nyilas M, Forbes RA, McQuade RD, Mallikaarjun S, et al. Efficacy of aripiprazole in the treatment of adolescents with schizophrenia. Poster presented at the 160th annual meeting of the American Psychiatric Association, San Diego, May 19–24, 2007Google Scholar
49 Delbello MP, Findling RL, Earley WR, Acevedo LD, Stankowski J. Efficacy of quetiapine in children and adolescents with bipolar mania: a 3-week, double-blind, randomized, placebo-controlled trial. Poster presented at the 54th annual meeting of the American Academy of Child and Adolescent Psychiatry, Boston, October 23–28, 2007Google Scholar
50 Tohen M, Kryzhanovskaya L, Carlson G, Delbello M, Wozniak J, Kowatch R, et al. Olanzepine versus placebo in the treatment of adolescents with bipolar mania. Am J Psychiatry. 2007; 164: 1547– 1556Crossref, Google Scholar
51 Chang KD, Nyilas M, Aurang C, Johnson B, Jin N, Marcus R, et al. Efficacy of aripiprazole in children (10–17 years old) with mania. Poster presented at the 54th annual meeting of the American Academy of Child and Adolescent Psychiatry, Boston, October 23–28, 2007Google Scholar
52 Pandina G, Delbello M, Kushner S, Van Hove I, Augustyns I, Kusumakar V, et al. Risperidone treatment of acute mania in bipolar youth. Poster presented at the 54th annual meeting of the American Academy of Child and Adolescent Psychiatry, Boston, October 23–28, 2007Google Scholar
53 Richelson E, Souder T. Binding of antipsychotic drugs to human brain receptors focus on newer generation compounds. Life Sci. 2000; 68: 29– 39Crossref, Google Scholar
54 Richelson E. Neuroleptic binding to human brain receptors: relation to clinical effects. Ann N Y Acad Sci. 1988; 537: 435– 442Crossref, Google Scholar
55 Richelson E, Nelson A. Antagonism by neuroleptics of neurotransmitter receptors of normal human brain in vitro. Eur J Pharmacol. 1984; 103: 197– 204Crossref, Google Scholar
56 Preskorn SH, Flockhart DA. 2006 guide to psychiatric drug interactions. Primary Psychiatry. 2006; 13: 35Google Scholar
57 Guy W, ed. ECDEU Assessment Manual for Psychopharmacology: Publication ABM 76-338. Washington, DC: US Department of Health, Education, and Welfare; 1976: 534– 537Google Scholar
58 Chouinard G, Ross-Chouinard A, Annabel L, Jones BD. The Extrapyramidal Symptom Rating Scale. Can J Neurol Sci. 1980; 7: 233Google Scholar
59 Simpson GM, Angus JW. A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl. 1970; 212: 11– 19Crossref, Google Scholar
60 Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988–1994. Arch Pediatr Adolesc Med. 2003; 157: 821– 827Crossref, Google Scholar
61 Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001; 285: 2486– 2497Crossref, Google Scholar
62 Fernandez JR, Redden DT, Pietrobelli A, Allison DB. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. J Pediatr. 2004; 145: 439– 444Crossref, Google Scholar
63 National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004; 114: 555– 576Crossref, Google Scholar



