The Doctor-Patient Relationship
Abstract
(Reprinted with permission from Simon RI, Shuman DW: The doctor-patient relationship, in Clinical Manual of Psychiatry and Law. Arlington VA, American Psychiatric Publishing Inc. 2007; 17–36)
OVERVIEW OF THE LAW
The establishment of the doctor-patient relationship is the legal predicate to the recognition of a professional duty of care owed to a patient. Because a medical malpractice claim demands proof that a doctor breached the duty he or she owed to a patient, the existence of a doctor-patient relationship and the duty of care it demands is a core issue in every malpractice claim. As a general rule, a psychiatrist in private practice is not required to accept anyone who seeks treatment and may choose whomever he or she wishes to treat (American Medical Association 1989; Gross v. Burt 2004). Similarly, psychiatrists have no legal obligation to provide emergency medical care to someone with whom they do not have a preexisting doctor-patient relationship, absent any contractual or statutory obligation (e.g., emergency department). Once a psychiatrist has agreed (explicitly or implicitly) to accept a patient, however, tort law anticipates continuity of care until the relationship is appropriately terminated.
THE LEGAL FOUNDATION FOR THE DOCTOR-PATIENT RELATIONSHIP
The legal foundation for recognizing the existence of a doctor-patient relationship is based on the agreement of the parties. Rather than impose duties that articulate when doctors should agree to treat patients, the law imposes duties when doctors have agreed to treat patients. The express or implied agreement to treat a patient creates a relationship with corresponding duties and rights for both parties (Oja v. Kin 1998). The doctor's duty of care is not predicated on the payment of a fee and arises even when care is provided gratuitously. It derives from the “agreement” by the physician to render services and the patient's reliance on that expectation.
The duty of care owed by the doctor to the patient as recognized under tort law does not demand that patients be cured but rather that the care not be negligent. Absent specific assurances by the doctor, initiating the professional relationship does not create any guarantee of specific results. Rather, initiation of the relationship implies a promise that the psychiatrist will exercise reasonable care according to the standards of the profession (Brown v. Koulizakis 1985).
When a psychiatrist is performing an evaluation for the benefit of a third party rather than treatment for the benefit of the patient, a doctor-patient relationship is generally not created. When the examination exclusively benefits a third party such as an employer (i.e., preemployment physical), insurance company (i.e., life insurance qualifying examination), or the courts (i.e., independent medical examination), usually no doctor-patient relationship and corresponding tort duty is found, because treatment or diagnosis in contemplation of treatment is not undertaken (State v. Supreme Court of Georgia 2005).
Psychiatrists who owe a duty of care to the patient and employ or supervise other professionals may be held vicariously liable for those other professionals' negligence, despite the absence of proof that the psychiatrist was negligent in care of the patient or in hiring, training, or supervising the employee (Lection v. Dyll 2001). Under the doctrine of respondeat superior, psychiatrists are vicariously liable, without regard to their own fault, for their employees' negligent acts in the scope of their employment. Whether the relationship is regarded as employer-employee, to which vicarious liability applies, or an independent contractor, to which vicarious liability does not apply, depends on the right or ability of the psychiatrist to control the other professional (e.g., supervisee or employee; Simons v. Northern P.R. Co. 1933).
FIDUCIARY ROLE: AVOIDING CONFLICT
One facet of the doctor-patient relationship policed by tort law is that of the fiduciary role the doctor is expected to play and the corresponding professional duties that arise (i.e., given the trust a patient places in his or her psychiatrist, a doctor owes duty of trust and candor). A psychiatrist is expected to act in good faith in his or her relations with a patient. This obligation is implicit within the consensual arrangement that gives rise to the relationship and inherent in all psychiatrist-patient relationships as an ethical and legal duty. Persons acting as a fiduciary are not permitted to use the professional relationship for their personal benefit. Thus, for example, psychiatrists must be particularly careful not to exploit transference for their personal gain. Double-agent role problems frequently arise when psychiatrists attempt to serve simultaneously the patient and an agency, institution, or society. These conflicts are examined in greater detail as they arise in the clinical management section of each chapter.
TERMINATION AND ABANDONMENT
Once a professional relationship has been created, a psychiatrist is legally required to provide the patient treatment unless or until the relationship is properly terminated (Ricks v. Budge 1947). Improper termination constitutes the tort of abandonment and the risk of malpractice liability for consequential harm. Generally, the psychiatrist-patient relationship may be properly terminated in one of the following ways:
| •. | Mutual agreement of psychiatrist and patient that the psychiatrist's services are no longer needed or useful | ||||
| •. | A unilateral act of the patient that indicates a withdrawal from treatment | ||||
| •. | A unilateral act of the psychiatrist that terminates treatment and provides a timely opportunity for the patient to obtain alternate care | ||||
A psychiatrist is not obligated to provide perpetual care for a patient. If there is no emergency or pending crisis (e.g., threatened suicide or danger to the public), generally a psychiatrist can lawfully terminate treatment by following certain procedures (Table 2–1).
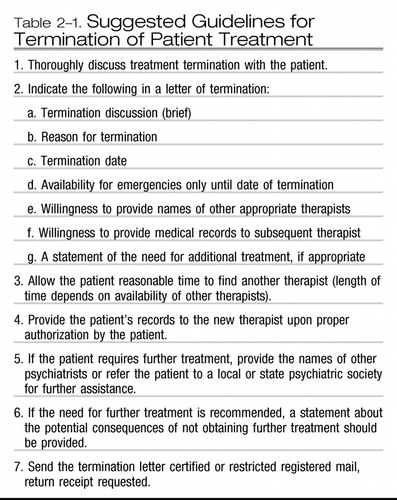 |
Table 2-1. Suggested Guidelines for Termination of Patient Treatment
Abandonment—tortiously failing to attend a patient absent the proper termination of the doctor-patient relationship—may be either overt or implied (e.g., failure to attend, monitor, or observe the patient). Many courts have widened the concept of abandonment to include situations in which delay and inattention in providing care caused the patient injury, termed constructive abandonment (i.e., as though actual abandonment had occurred [Mains 1985]). For example, in Bolles v. Kinton (1928), the court stated that a physician cannot discharge a case by simply not attending the patient without sufficient notice. Others courts have found abandonment when psychiatrists make themselves inaccessible to patients, particularly if a crisis is occurring or foreseeable. The following have all been construed by the courts as negligent acts amounting to abandonment:
| •. | Failure to provide patients with a way to contact the psychiatrist between sessions | ||||
| •. | Failure to maintain reasonable contact with a hospitalized patient | ||||
| •. | Failure to provide adequate clinical coverage when away from practice | ||||
CLINICAL MANAGEMENT OF LEGAL ISSUES
CREATION OF THE DOCTOR-PATIENT RELATIONSHIP
A psychiatrist does not owe a professional duty of care to a person as a patient unless a psychiatrist-patient relationship exists. Once that relationship is established, however, duties attach, and the psychiatrist is liable for damages that are proximately caused by their breach (Roberts v. Sankey 2004). Whether a psychiatrist-patient relationship exists is a mixed question of law and fact. If the existence of a relationship is disputed, the court determines, as a preliminary matter, whether the patient entrusted care to the psychiatrist and whether the psychiatrist indicated acceptance of that care (Dehn v. Edgecombe 2005). Most often, a psychiatrist-patient relationship is established knowingly and voluntarily by both parties. Occasionally, however, a doctor-patient relationship is unwittingly created.
Although the law imposes no duty on physicians to accept a prospective patient, courts have been quick to recognize a doctor-patient relationship when the physician affirmatively undertakes to diagnose and or treat a person (Kelley v. Middle Tenn. Emergency Physicians, P.C. 2004). Several examples are instructive. Giving advice, making interpretations, or prescribing medication during the course of an independent medical evaluation may create a doctor-patient relationship (Newman and Newman 1989). A doctor-patient relationship may be created when a person is provided care over the telephone, if that person has the expectation that he or she is accepted for treatment. Courts will likely treat doctor-patient relationships created by e-mail as they have those created by phone, mail, or in person (Table 2–2).
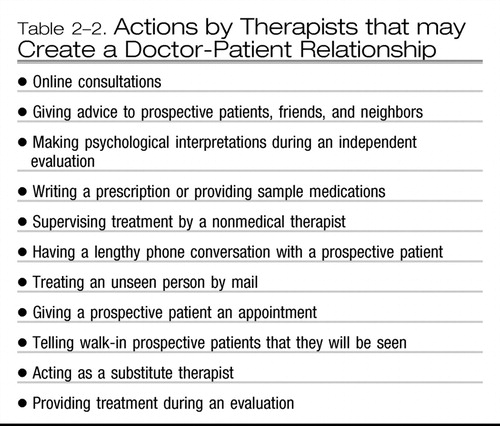 |
Table 2-2. Actions by Therapists that may Create a Doctor-Patient Relationship
Judicial decisions that hold therapists liable to third persons—not because they are patients, but because they allege that the therapist's negligent patient care resulted in harm to them—have increased. These claims have been made by persons about whom the patient made threats in therapy and who were later injured by the patient. The injured third party in these cases claims the threats were mishandled (Tarasoff v. Regents of the University of California 1976). Another class of third-party claims have been made by individuals who allege that, because of inappropriate therapies used by the psychiatrist, they were wrongfully remembered by the patient in therapy as having been the perpetrator of childhood sexual abuse (Appelbaum et al. 1997). The duty issue in these cases is separate from the duty issue that arises with participants in formal family or group therapy. The courts addressing these third-party claims do not focus on the requirements for the existence of a doctor-patient relationship but instead on whether the harm that may have been caused by the therapist's negligence is proximate or too remote to be attributed to any negligence in the care of the patient.
Unless they are a formal part of the patient's therapy, families are usually not considered parties to the case (Gutheil and Simon 1997). Family members who are brought into the patient's treatment in a brief, adjunctive role must be clearly informed that they are not being seen as patients. If therapy for other family members is indicated, they should be referred elsewhere for treatment.
Psychiatrists and other clinicians are often asked by friends, family members, neighbors, or colleagues for clinical advice or medications. These quasimedical relationships are potentially fraught with serious problems (LaPuma and Priest 1992). Psychiatrists who wish to provide professional services in these situations must understand they may be creating a doctor-patient relationship with an attendant duty of care. As in the usual clinical situation, medical records should be maintained that document that the standard of care was met in evaluation, diagnosis, and indications for treatment.
Ordinarily, clinicians who perform preemployment, insurance, or workers' compensation examinations do so for the benefit of a third party, not the examinee, and accordingly a doctor-patient relationship does not arise for purposes of medical malpractice liability (Chiasera v. Employers Mut. Liability Ins. Co. 1979; Ervin v. American Guardian Life Assurance Co. 1988; Violandri v. New York 1992). Independent of medical malpractice liability for negligence as a caregiver, psychiatrists may be liable for performing negligent examinations (McKinney v. Bellevue Hosp. 1992) or for defamation if untrue and damaging statements are made about the examinee (James v. Brown 1982). Therapists who examine litigants at the request of the court are typically immune from liability for negligence. Psychiatrists appointed by the court in civil commitment cases are generally protected from liability as well. When, however, the psychiatrist medically certifies his or her own patient, liability claims may not be barred by imposition of immunity for negligently initiated commitment. (This issue is examined further in Chapter 7, “Involuntary Hospitalization.”)
“Curbside consultations,” or informal advice given in response to a colleague's question, are not categorically excluded from the recognition of a duty of care enforceable in a medical malpractice claim because of their location, reimbursement, or informality. Rather, in the event of a malpractice claim, each consultation will be judged by the court on its own facts, applying the criteria generally applied for recognition of a doctor-patient relationship. Thus the law's expectations for consultations do not countenance a sliding competence scale for discounted opinions.
Patient evaluation: the right to accept or reject new patients.
When seeing a prospective patient for the first time, psychiatrists may want to conduct an evaluation before accepting the person as a patient. The clinician should inform the prospective patient that no treatment will be provided during the evaluation. In actual clinical practice, this may not always be possible. The psychiatrist usually does not know the extent of the prospective patient's disturbance prior to seeing him or her for the first time. Some individuals show floridly psychotic symptoms during the initial visit and may be a danger to themselves or others. The psychiatrist may decide to immediately intervene and forgo the initial evaluation period. The clinician's first duty is to the welfare of the patient.
The common law “no duty to rescue” rule is still very much good law. Not even health care professionals have a duty to come to the aid of a stranger who is helpless and in peril, but if that duty is undertaken there is an obligation to do so non-negligently (Shuman 1993). The application of this rule to a psychiatrist in private practice means that he or she is not required to accept a new patient, but if he or she does there is an obligation to provide competent care. Psychiatrists may feel helpless and trapped when confronted with a new patient who is in a crisis and requires immediate attention. Psychiatrists who do not want to accept the patient for treatment should attempt to find immediate, competent help. In some instances, this may require accompanying the patient to a hospital or an emergency department. Professional ethics and concern for the patient in crisis dictate that the patient be assisted in obtaining immediate care (Simon 1992).
Malpractice concerns can be an additional incentive to see prospective patients for an initial evaluation before accepting them for treatment. In split treatment or collaborative therapy, careful evaluation of the patient's suitability is necessary. Psychiatrists are increasingly vulnerable to lawsuits by patients seen within a short period of time, even less than 30 days. Eight out of every 10 persons who commit suicide have visited a physician within the 6 months prior to the attempt, and half (50%) have seen a physician within 1 month prior. The psychiatrist should perform a suicide risk assessment at the initial evaluation, even if the patient denies being suicidal.
Clinicians usually accept many more patients than they reject. Upon completion of the evaluation, a decision by both the psychiatrist and the patient can be made about whether to begin treatment. The psychiatrist should scrupulously avoid rendering advice, interpretations, or any other intervention that might be construed as treatment during the evaluation period.
Psychiatrists have no legal obligation to provide emergency medical care to a person who is not a patient (failure to provide emergency care to an existing patient may constitute abandonment). Nevertheless, the American Medical Association (1989) advises, “The physician should, however, respond to the best of his [or her] ability in cases of emergency where first aid treatment is essential” (p. 33). If a psychiatrist undertakes to render assistance to the person “at the wayside,” Good Samaritan statutes provide a layer of protection for physicians providing gratuitous emergency medical care against damages arising out of any professional act or omission performed in “good faith” and not amounting to gross negligence (Estate of Heune ex. rel. Heune v. Edgecomb 2005). Good Samaritan laws typically include the physician who is not licensed in the state where the emergency care takes place (for a listing of Good Samaritan statutes, see Centner 2000).
Role conflicts.
The practice of psychiatry bristles with moral dilemmas. Role conflicts occur when mental health professionals have irreconcilable interests that interfere with their fiduciary responsibility to act solely in the best interest of the patient. These role conflicts are sometimes labeled as double agentry, which refers to a conflict between serving the patient and serving some external agency (The Hastings Center 1978). Role conflicts hold a high potential for interfering with the fiduciary duties psychiatrists owe their patients. For example, psychiatrists working in mental institutions must manage the conflict between serving their patients and advancing the goals of the institution and society. Following the emergence of Tarasoff in those states that recognize a psychotherapist's duty to protect third parties endangered by their patients, psychiatrists were explicitly called upon to balance the conflicting duty to protect patient confidentiality and to protect persons identified as at risk in a patient's confidential communications. Psychiatrists who work in prisons, in schools, or in the military regularly face potentially serious double-agent conflicts. Psychiatrists and other mental health professionals are expected to clinically manage conflicting pressures that inevitably arise from these different sectors without disrupting the doctor-patient relationship.
Therapists who sexually exploit their patients violate their fiduciary responsibilities. Such violation also may occur when patients who have been sexually abused are referred to a new therapist for much-needed treatment, and the new therapist, because of forensic interests or moral outrage, converts the treatment relationship into a forensic case. The therapist may encourage the patient to file a lawsuit and help initiate ethical and licensure proceedings against the former therapist. Therapists should not confound treatment with advocacy. The roles of treater and expert witness must be kept separate to avoid serious conflicts of interest (Strasburger et al. 1997). Advocacy should not be misrepresented to the patient as treatment. “Once a patient, always a patient” is a sound principle that allows patients to go about their lives free from the presence and influence of their therapists.
SUPERVISOR-SUPERVISEE RELATIONSHIPS AND LIABILITY
Under the doctrine of respondeat superior (vicarious liability), an institution and its staff (e.g., supervising psychiatrist) may be liable for the negligent acts and omissions of other mental health professional employees in the scope of their employment. Vicarious liability is imposed based on the negligence of the employee, not the employer.
A professional distinction exists in a psychiatrist's supervisory obligation for medical and nonmedical psychotherapists. The American Psychiatric Association's (1980)Official Actions: Guidelines for Psychiatrists in Consultative, Supervisory, or Collaborative Relationships With Nonmedical Therapists states that the psychiatrist who supervises a nonmedical therapist is responsible for the patient's diagnosis and treatment plan and ensuring that the treatment plan is properly administered with suitable adjustments for the patient's condition. The guidelines do not specify the frequency of supervisory contacts. While supervising nonmedical therapists, psychiatrists are responsible for the patients as though the patients are their own. The guidelines have not been updated to accord with the current systems of mental health care delivery.
Direct and vicarious liability.
When a psychiatrist supervises a psychiatric resident or intern who is treating the psychiatrist's patient, the resident or intern may be considered a borrowed servant. As a result, the psychiatrist is vicariously responsible for negligence of the resident or intern that leads to harm (Frazier v. Hurd 1967). Interns and residents treating their own patients but supervised by a psychiatrist may incur liability directly for negligence, whereas the supervisor and the institution may incur vicarious liability. Residents are held to the same standard of care as attending psychiatrists when they represent themselves to the public as treaters of mental illness. Psychiatrists supervising other graduate psychiatrists may be viewed as independent contractors who would not likely be liable for acts of negligence of the supervised psychiatrist. Although not strictly consultative, the supervisory relationship with graduate psychiatrists appears to be closer to the consultative model, even though it occurs on a continuing basis.
The psychiatric treatment team concept has gained considerable popularity in the managed care era. The team usually contains a psychiatrist, nurses, social workers, and other mental health professionals. Team members may be held liable for the negligence of an individual team member. Psychiatrists also may be held liable under the doctrine of joint and several liabilities for the negligent acts of partners, even though they have not treated the patient (Fanelli v. Adler 1987). Finally, vicarious liability may be imposed on psychiatrists for the negligent acts of employees committed within the scope of their employment (Steinberg v. Dunseth 1994).
Collaborative relationships: split treatment.
In a collaborative relationship, responsibility for the patient's care is shared according to the qualifications and limitations of each discipline (American Psychiatric Association 1980). The responsibilities of each discipline do not diminish those of the other discipline. Split treatment is an example of a collaborative relationship. The shrinking of available mental health dollars and increases in administrative pressure from third-party payers, particularly managed care organizations (MCOs), are the driving forces behind the increasing utilization of split treatment in the clinical management of the severely mentally ill.
The psychiatrist-psychotherapist team must overcome some difficult hurdles to facilitate the collaboration (Meyer and Simon 1999a, 1999b). The patient's clinical illness cannot be easily placed into the domain of one clinician or the other. Because neither clinician can rightfully claim to be in charge of the other, there is no established clinical hierarchy. Often, there is neither a preexisting agreement by which clinicians convey information about the patient nor one about what information needs to be conveyed. Psychiatrists and their nonphysician mental health colleagues should reach an agreement about the respective clinical duties of each clinician and a plan for clinical interactions. The main liability dangers of collaborative treatment include the following:
| •. | Failure to establish clear lines of communication and clinical responsibility in split-treatment situations, early and in writing, between the psychiatrist and the nonmedical therapist (e.g., coverage for emergencies, hospitalizations, absences). | ||||
| •. | Insufficient clinical knowledge of the patient | ||||
| •. | Failure to provide careful monitoring of the patient's clinical condition | ||||
| •. | Failure to maintain ongoing communication with the nonmedical therapist regarding the patient's treatment | ||||
PATIENT BILLING
Dubious practices.
Conflicting, self-serving interventions can occur over billing and fees. Most therapists explain their fees at the beginning of treatment so that patients can agree, disagree, or enter into negotiations for a mutually agreed-on fee. Role conflicts can arise over billing for times reserved or by discounting or inflating bills.
Discounting of bills occurs when the patient has insurance but is unable to pay the full portion of the bill. The therapist may accept either no payment or a lower payment from the patient. When the psychiatrist accepts the insurance reimbursement as payment in full, the insurer is actually paying 100% of the bill. Insurance carriers consider this practice to be fraudulent because the participating psychiatrist is pocketing their “overpayment.”
Psychiatrists who inflate bills to insurance carriers may also be vulnerable to charges of fraud and misrepresentation. Inflating of bills refers to charging the insurance carrier a higher fee than the therapist is actually charging the patient. When this happens, the difference is pocketed or applied to the patient's portion. Therapists are not agents of the insurance company, nor should they be agents of the patient against the carrier. Exaggerating the severity of a patient's mental disorder to obtain coverage under managed care is a related deceptive practice. A position of neutrality on insurance matters maintains the psychiatrist's integrity and preserves the treatment. Engaging in dubious fee practices undermines the credibility of the psychiatrist if she or he becomes entangled with the patient in litigation.
Psychiatrists are entitled to charge a reasonable fee for their services. Billing for missed appointments is appropriate if the patient is advised of this practice at the outset and freely consents. Charges for missed sessions should not be represented as treatment sessions to third-party payers. This practice could be interpreted as misrepresentation and fraud. Psychiatrists who receive direct payment from third-party payers are not paid for appointments that are reported as missed. Moreover, under provider contractual agreements, most MCOs and other third-party payers prohibit psychiatrists from billing the patient for any unauthorized services, including missed appointments. The ethical and prudent course is to note missed appointments on the billing form, even if the psychiatrist must take a financial loss. In some circumstances, a legitimate arrangement may be worked out with the patient to pay for missed appointments.
Nonpayment: clinical issues.
In general, the psychiatrist has no legal duty to continue to treat patients who do not pay. The psychiatrist, however, must be careful not to abandon the patient. The patient who runs out of money during the course of extended therapy presents a difficult problem. Terminating the patient's treatment may be very destructive to the unique relationship that developed between psychiatrist and patient. The psychiatrist may decide to treat the patient for a token fee until the patient's financial situation improves, at which time a new fee can be negotiated. Allowing the patient to pay the money owed at a later date places the psychiatrist in the position of a creditor, a potentially conflicting role. Similarly, entering into a barter arrangement with a nonpaying patient should be avoided. Patients in need of treatment may not be able to objectively assess the value of their goods. When others assume financial responsibility for the patient, the therapist may wish to formalize the arrangement with a written agreement. As insurance benefits for psychiatric care continue to be cut back by MCOs and other third-party payers' cost-containment policies, treatment of patients needing further care may be improperly terminated.
ABANDONMENT
Once the psychiatrist agrees to treat the patient, a psychiatrist-patient relationship is formed with the duty to provide treatment as long as is necessary. When the psychiatrist-patient relationship is unilaterally and prematurely terminated by the psychiatrist without reasonable notice, the psychiatrist may be liable for abandonment if care is still needed by the patient (see Grant v. Douglas Women's Clinic P.C. 2003). If an emergency exists, the psychiatrist should see the patient through the current crisis or make suitable arrangements for attendance of another qualified mental health professional (see Johnson v. Vaughn 1963). For patients in perpetual crisis, this is a daunting task. Similarly, terminating treatment of a chronically ill patient who is in serious psychiatric difficulty should be deferred until the immediate crisis is over or until the patient is well enough to be transferred or discharged.
Although the doctor-patient relationship may be terminated unilaterally by the patient, the following actions by a patient do not, in and of themselves, terminate the doctor-patient relationship:
| •. | Nonpayment of a bill (However, there are limits: for example, in Surgical Consultants, P.C. v. Ball [1989], the court ruled that the doctor did not have to continue treatment when the patient failed to pay her bill after 11 sessions.) | ||||
| •. | Noncooperation in treatment (However, the physician does not have to continue treatment when there is no hope of helping the patient through current therapy.) | ||||
| •. | Unilateral consultation with another mental health professional | ||||
| •. | Failure to keep an appointment | ||||
None of these actions by the patient, in and of themselves, constitutes unilateral termination of treatment. However, these issues should be taken up as treatment matters. If the patient stops coming for regularly scheduled appointments, does the therapist have a duty to contact the patient? The answer to this question depends on whether the patient's absence is a direct function of mental illness. The more severe the illness, the more the psychiatrist should assume responsibility for contacting the patient. When it is not clear whether the patient has terminated treatment, the psychiatrist should attempt to clarify the patient's intentions concerning further treatment. If a patient stops coming for treatment without further explanation, the psychiatrist should send a certified letter (return receipt requested) to ascertain whether treatment has been terminated by the patient.
When the doctor-patient relationship has not been properly terminated by the patient, by the psychiatrist, or by the mutual agreement of both, the negligent acts may be categorized as abandonment of the patient (see Table 2–3).
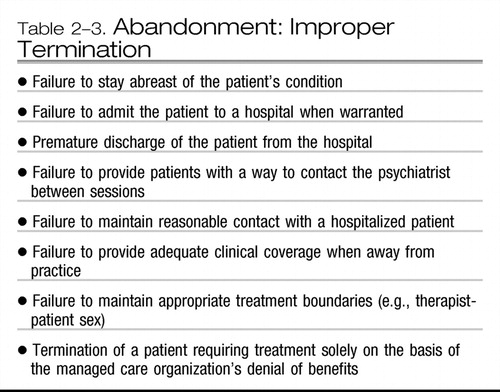 |
Table 2-3. Abandonment: Improper Termination
Psychiatrists who request other psychiatrists to hospitalize their patients should stay in contact with the admitting psychiatrist and shift temporarily into a consultative role. Unless the patient is being permanently transferred to the care of the hospitalizing psychiatrist, the referring psychiatrist should continue to stay abreast of clinical developments with his or her patient. Communication between psychiatrists is essential to the patient's care.
Finally, abandonment may become an issue when therapists do not list a phone number in the telephone directory or with directory assistance. Being inaccessible to patients measurably increases their anxiety and causes some patients to go to extraordinary lengths to find their therapists. Ready availability of the psychiatrist appears to diminish patients' anxiety and results in fewer calls. In addition, if an emergency should arise, claims of abandonment are preempted when the psychiatrist can be easily contacted. Leaving a message on the answering service such as “If you have a true emergency, please go to your nearest emergency department” may be perceived by the patient as abandonment. In an emergency, patients want to speak to their psychiatrists. Waiting for hours to be seen in an emergency department may exacerbate the patient's illness and result in the patient leaving prematurely.
COVERAGE
When a psychiatrist obtains clinical coverage for absences from his or her practice, a clinician of similar experience and training should be found. Clinical information about patients who may be considered at risk for suicide or vulnerable to regression in the clinician's absence should be provided to the covering psychiatrist with the patient's permission. Patients need to be informed of the name of the psychiatrist providing coverage as well as the length of the treating psychiatrist's absence. A psychiatrist who obtains coverage is not generally liable for the covering psychiatrist's negligence unless the covering psychiatrist is acting as an agent of the psychiatrist or due diligence was not exercised in selecting the substitute covering psychiatrist. If a fixed stipend is paid to the covering psychiatrist from fees collected, an agent (employee) relationship is likely established. If the patient is billed and the proceeds are shared with the covering psychiatrist after expenses, then a partnership is created. To reduce legal entanglements, the covering psychiatrist should bill independently for services rendered.
TERMINATION
The psychiatrist has the right to terminate a doctor-patient relationship if proper notice is given so that the patient may find a suitable substitute (see Brandt v. Grubin 1974).
Unilateral terminations.
A psychiatrist may seek to terminate a patient's treatment because of managed care limitations on insurance benefits. However, the liability exposure for terminating treatment of a patient in crisis because of managed care restrictions is high. As noted earlier, termination of treatment for the patient in crisis should be deferred until his or her situation is reasonably stabilized. Before termination, the psychiatrist should give the patient sufficient notice to make other treatment arrangements. The psychiatrist should also review with the patient the current diagnosis, the importance of continuing with prescribed treatments, and the need for additional treatment. A note in the patient's chart and a brief letter sent to the patient should summarize the psychiatrist's treatment recommendations. The psychiatrist may decide to continue to treat a patient after managed care benefits end. Managed care contracts should be checked for any clause that prohibits treatment of managed care patients under a private fee-for-service arrangement.
The patient has the right to leave treatment at any time and without notice. In some instances, the patient may terminate by simply not showing up for scheduled appointments. A patient who is mentally ill and poses a substantial danger to self or others may suddenly decide to terminate. In such instances, the psychiatrist's ethical and professional duties to care for the patient continue and require that the psychiatrist consider a variety of clinical interventions.
Some patients are genuinely difficult and demanding in their own right, presenting unique problems that some psychiatrists can handle better than others. The fit between psychiatrist and patient may not be workable. If treatment becomes stalemated or contentious, the patient should be referred elsewhere.
Professional and ethical duty demands that the psychiatrist not treat patients beyond the point of benefit. Patients can become mired in therapeutic stalemates extending for years. This situation tends to occur when an Axis I clinical syndrome is successfully treated, but the remaining Axis II personality disorder goes undiagnosed or is intractable to treatment. Even though the patient may strenuously resist, it is not abandonment if such a patient is referred to another therapist who may be able to treat the patient more effectively once the previous treatment is appropriately terminated.
Method of termination.
Termination and the treatment issues surrounding it should be openly discussed with the patient and a notation of the discussion placed in the patient's record. A certified letter notifying the patient of termination should be sent and a return receipt requested. If the terminated patient is seen again after the letter is issued and termination is still intended, the entire termination process must be reinstituted (Table 2–1).
How much time should the patient be given to find another therapist? The time allowed should be based on the severity of the patient's condition and the availability of alternative care. Patients who present with complex, severe mental illnesses may find it more difficult to find a psychiatrist willing or able to treat them. Sufficient notice also depends on the locality. The availability of psychiatrists in rural settings is often limited. The patient may need more time to find a psychiatrist than would be necessary in an urban area. The courts have used such normative words as ample, sufficient, and reasonable when referring to the time that should be given the patient to find a substitute.
MANAGED CARE AND THE DISCHARGE OF HOSPITALIZED PATIENTS
Doctors—not hospitals or MCOs—are responsible for the discharge of patients (Simon 1997). Hospitalized psychiatric patients should not be summarily discharged because insurance coverage for recommended continued hospitalization is denied. Provisions for continuing adequate care should be made before the patient is discharged. Occasionally, a hospital will pressure a psychiatrist to discharge a patient whose insurance benefits have ended. If the patient presents a high risk of danger to self or others, both the psychiatrist and the hospital will be at increased risk of liability if the patient or a third party is harmed. Managed care considerations must not be permitted to override treatment and discharge decisions. The premature discharge of psychiatric inpatients that are at increased risk of committing violence toward themselves or others is expected to become an increasingly important area of litigation in the managed care era (Simon 1998).
MCO cost-containment policies often restrict physicians' therapeutic discretion even as the physicians' professional and legal responsibilities to patients continue unchanged. For example, hospital lengths of stay may be abbreviated, often inappropriately, for inpatients with serious psychiatric disorders. When managed care guidelines conflict with the psychiatrist's duty to provide appropriate clinical care, the psychiatrist should vigorously appeal managed care decisions that abridge necessary treatments. If advocacy efforts fail, patients should be informed of their right to appeal MCO denial of services that the psychiatrist has documented as medically necessary. Once a treatment plan is recommended to the patient, the psychiatrist has a duty to complete the treatment or arrange for a suitable treatment alternative (Siebert and Silver 1991). MCOs generally limit or deny payment for services but not the actual services themselves. The physician is responsible for decisions involving patient care and disposition (Wickline v. California 1986; Wilson v. Blue Cross of So. California et al. 1990).
American Medical Association: Current Opinions: The Council on Ethical and Judicial Affairs of the American Medical Association. Chicago, IL, American Medical Association, 1989Google Scholar
American Psychiatric Association: Official actions: guidelines for psychiatrists in consultative, supervisory, or collaborative relationships with nonmedical therapists. Am J Psychiatry 137: 1489– 1491, 1980Crossref, Google Scholar
Appelbaum PS: General guidelines for psychiatrists who prescribe medication for patients treated by nonmedical therapists. Hosp Community Psychiatry 42: 281– 282, 1991Google Scholar
Appelbaum PS, Uyehara LA, Elin MR (eds): Trauma and Memory: Clinical and Legal Controversies. New York, Oxford University Press, 1997Google Scholar
Centner TJ: Tort liability for sports and recreational activities: expanding statutory immunity for protected classes and activities. J Legis 26: 1– 44, 2000Google Scholar
Gutheil TG, Simon RI: Clinically based risk management principles for recovered memory cases. Psychiatr Serv 48: 1403– 1407, 1997Crossref, Google Scholar
LaPuma J, Priest ER: Is there a doctor in the house? An analysis of the practice of physicians treating their own families. JAMA 267: 1810– 1812, 1992Crossref, Google Scholar
Mains J: Medical abandonment. Med Trial Tech Q 31: 306– 328, 1985Google Scholar
Meyer D, Simon RI: Split treatment: clarity between psychiatrists and psychotherapists, part I. Psychiatr Ann 29: 241– 245, 1999aCrossref, Google Scholar
Meyer D, Simon RI: Split treatment: clarity between psychiatrists and psychotherapists, part II. Psychiatr Ann 29: 327– 332, 1999bCrossref, Google Scholar
Newman A, Newman K: Physician's duty in independent medical evaluations. Leg Aspects Med Pract 17: 8– 9, 1989Google Scholar
Shuman DW: The duty of the state to rescue the vulnerable in the United States, in The Duty to Rescue: The Jurisprudence of Aid. Edited by Menlowe M, McCall Smith A. Brookfield, VT, Dartmouth Publishing, 1993, pp 131– 158Google Scholar
Siebert SW, Silver SB: Managed health care and the evolution of psychiatric practice, in American Psychiatric Press Review of Clinical Psychiatry and the Law, Vol 2. Edited by Simon RI. Washington, DC, American Psychiatric Press, 1991, pp 259– 270Google Scholar
Simon RI: Clinical Psychiatry and the Law, 2nd Edition. Washington, DC, American Psychiatric Press, 1992Google Scholar
Simon RI: Discharging sicker, potentially violent psychiatric inpatients in the managed care era: standard of care and risk management. Psychiatr Ann 27: 726– 733, 1997Crossref, Google Scholar
Simon RI: Psychiatrists' duties in discharging sicker and potentially violent inpatients in the managed care era. Psychiatr Serv 49: 62– 67, 1998Crossref, Google Scholar
Strasburger LH, Gutheil TG, Brodsky A: On wearing two hats: role conflict in serving as both psychotherapist and expert witness. Am J Psychiatry 154: 448– 456, 1997Crossref, Google Scholar
The Hastings Center: In the Service of the State: The Psychiatrist as Double Agent (Special Supplement). Hastings-on-Hudson, NY, The Hastings Center, 1978Google Scholar
Bolles v Kinton, 83 Colo. 147, 153, 263 P. 26, 28 ( 1928)Google Scholar
Brandt v Grubin, 131 NJ Super 182, 329 A.2d 82 ( 1974)Google Scholar
Brown v Koulizakis, 229 Va. 524, 331 S.E.2d 440 ( 1985)Google Scholar
Chiasera v Employers Mut. Liability Ins. Co., 101 Misc.2d 877, 422 N.Y.S.2d 341 ( 1979)Google Scholar
Dehn v Edgecombe, 865 A.2d 603 (Md., 2005)Google Scholar
Estate of Heune ex. rel. Heune v. Edgecomb, 823 N.E.2d 1123 (Ill. App., 2005)Google Scholar
Ervin v American Guardian Life Assurance Co., 545 A.2d 354 (Pa. Super. Ct., 1988)Google Scholar
Fanelli v Adler, 516 N.Y.S.2d 716, 131 A.D.2d 631 (N.Y.A.D. 2 Dept., 1987)Google Scholar
Frazier v Hurd, 149 N.W.2d 226 (Mich. App., 1967)Google Scholar
Grant v Douglas Women's Clinic P.C., 580 S.E.2d 532 (Ga. App., 2003)Google Scholar
Gross v Burt, 149 S.W.3d 213 (Tex. App., 2004)Google Scholar
James v Brown, 637 S.W.2d 914 (Tex., 1982)Google Scholar
Johnson v Vaughn, 370 S.W.2d 591 (Ky., 1963)Google Scholar
Kelley v Middle Tenn. Emergency Physicians, P.C., 133 S.W.3d 587 (Tenn., 2004)Google Scholar
Lection v Dyll, 65 S.W.3d 696, 704 (Tex. App. Dallas, 2001) review denied (Nov. 8, 2001)Google Scholar
McKinney v Bellevue Hosp. 584 N.Y.S.2d 538, 183 A.D.2d 563 (N.Y.A.D. 1 Dept., 1992)Google Scholar
Oja v Kin, 581 N.W.2d 739, 229 Mich. App. 184 (Mich. App., 1998)Google Scholar
Ricks v Budge, 64 P.2d 208 (Utah, 1947)Google Scholar
Roberts v Sankey, 813 N.E.2d 1195 (Ind. App., 2004)Google Scholar
Simons v Northern P.R. Co., 22 P.2d 609 (Mont., 1933)Google Scholar
State v Supreme Court of Georgia, 613 S.E.2d 647 (Ga., 2005)Google Scholar
Steinberg v Dunseth, 631 N.E.2d 809, 813 (Ill. App.), cert. denied, 642 N.E.2d 1304 (Ill. 1994)Google Scholar
Surgical Consultants, P.C. v Ball, 447 N.W.2d 676 (Iowa Ct. Appl., 1989)Google Scholar
Tarasoff v Regents of the University of California, 17 Cal.3d 425; 551 P.2d 334 (Cal. Rptr., 14 1976)Google Scholar
Violandri v New York, 184 A.D.2d 364, 584 N.Y.S.2d 842 ( 1992)Google Scholar
Wickline v California, 183 Cal. App.3d 1175, 228 Cal. Rptr. 661 (Cal. Ct. App., 1986)Google Scholar
Wilson v Blue Cross of So. California et al., 222 Cal. App.3d 660 ( 1990)Google Scholar



