Encouraging Posttreatment Self-Help Group Involvement to Reduce Demand for Continuing Care Services: Two-Year Clinical and Utilization Outcomes
Abstract
Background:
Accumulating evidence indicates that addiction and psychiatric treatment programs that actively promote self-help group involvement can reduce their patients' health care costs in the first year after treatment, but such initially impressive effects may wane over time. This paper examines whether the positive clinical outcomes and reduced health care costs evident 1 year after treatment among substance-dependent patients who were strongly encouraged to attend 12-step self-help groups were sustained at 2-year follow-up. Methods: A 2-year quasi-experimental analysis of matched samples of male substance-dependent patients who were treated in either 12-step-based (n = 887 patients) or cognitive-behavioral (CB, n = 887 patients) treatment programs. The 12-step-based programs placed substantially more emphasis on 12-step concepts, had more staff members “in recovery,” had a more spiritually oriented treatment environment, and promoted self-help group involvement much more extensively than did the CB programs. The 2-year follow-up assessed patients' substance use, psychiatric functioning, self-help group affiliation, and mental health care utilization and costs. Results: As had been the case in the 1-year follow-up of this sample, the only difference in clinical outcomes was a substantially higher abstinence rate among patients treated in 12-step (49.5%) versus CB (37.0%) programs. Twelve-step treatment patients had 50 to 100% higher scores on indices of 12-step self-help group involvement than did patients from CB programs. In contrast, patients from CB programs relied significantly more on outpatient and inpatient mental health services, leading to 30% lower costs in the 12-step treatment programs. This was smaller than the difference in cost identified at 1 year, but still significant ($2,440 per patient, p = 0.01). Conclusions: Promoting self-help group involvement appears to improve posttreatment outcomes while reducing the costs of continuing care. Even cost offsets that somewhat diminish over the long term can yield substantial savings. Actively promoting self-help group involvement may therefore be a useful clinical practice for helping addicted patients recover in a time of constrained fiscal resources.
(Reprinted with permission from Alcoholism: Clinical and Experimental Research 2007; 31(1):64–68)
Most public and private sector addiction treatment providers face substantial pressure to treat large numbers of patients within a constrained budget. Yet, reducing services to meet budgetary requirements may pose a risk to addicted patients, many of whom are in an acutely vulnerable state when they enter treatment (e.g., homeless, suicidal, HIV-positive). This study evaluates one strategy for reconciling these conflicting pressures: making self-help group involvement a central goal of treatment, such that patients will rely relatively less on professional continuing care services over time but still attain good outcomes.
The first formal evaluations of the potential health care cost offset of various peer-directed interventions were conducted with seriously mentally ill individuals. What we believe was the first such study showed that discharged psychiatric inpatients randomly assigned to a patient-led support network were 50% less likely to be rehospitalized in the ensuing 10 months than were patients assigned to usual aftercare (Gordon et al., 1979). Outpatient care needs were also reduced, with only 47.5% of experimental patients continuing to access community-based mental health services versus 74.0% of controls. This study did not report data on clinical outcomes, but later research on the 12-step self-help group GROW suggested that the organization reduces reliance on psychiatric care (Kennedy, 1989) while simultaneously leading to improvement on self-rated and interviewer-rated measures of socio-psychologic functioning (Roberts et al., 1999). Considered together, these findings raise the possibility that promoting self-help group involvement may yield cost savings without compromising outcomes.
Addiction researchers have more recently begun to examine the relationship of self-help group (also known as a mutual help group) involvement and health care utilization. In a sample of 201 alcohol-abusing individuals, those who first sought help from Alcoholics Anonymous (AA) versus from professional outpatient treatment providers experienced comparable decreases in alcohol consumption and dependence symptoms (around 70%) by 3-year follow-up. These gains were less expensively achieved in the AA condition, where alcohol-related health care costs were 45% lower over the duration of the study. The study was not a randomized trial, but the similarity of the 2 groups at baseline made self-selection an unlikely explanation for such a large difference in costs (Humphreys and Moos, 1996; see also Humphreys et al., 1996).
One cannot assume, however, that sizable cost offsets will persist in the long term. In the Walsh et al. (1991) randomized trial of alcohol-abusing blue collar workers, individuals initially assigned to AA-only no doubt had much lower costs in the first months of the study than did individuals assigned to AA+, hospital-based inpatient treatment program. But because the AA-only group experienced more relapses requiring medical intervention as the study progressed, by 2-year follow-up, the AA-only condition costs were only 10% lower than those of the AA+ Inpatient treatment condition. In the Humphreys and Moos (1996) study, waning of offsets over time was also evident: the 3-year difference in cost was entirely attributable to the offset in the first year of the study. Whether cost offsets and good outcomes from self-help group involvement can be sustained are vital questions for the addiction field because of the ever-present temptation in both public and private budgeting to adopt practices that “save money” simply by shifting costs to later budgets.
The present study is designed to test this question directly, using a sample of 1,774 veterans upon whom we previously reported findings in this journal (Humphreys and Moos, 2001). Patients treated in 12-step programs that extensively promoted mutual help group involvement had 25% higher abstinence rates and 40% lower health care costs 1 year after treatment than did patients treated in cognitive-behavioral (CB) programs. These are large differences, but the studies cited above caution against assuming that these cost and outcome differences will hold up over time. We examine this question here by analyzing the sample's 2-year clinical and health care utilization outcomes.
METHODS
TREATMENT PROGRAMS
The treatment programs were 12-step-oriented (n = 5) and CB (n = 5) inpatient programs participating in the Department of Veterans Affairs nationwide multisite substance abuse treatment outcome study (described in detail in a special section of this journal; see Moos et al., 1999). The programs treated drug and alcohol patients on an inpatient basis for 21 to 28 days and offered out-patient continuing care after discharge.
A range of data indicate that the programs classified as 12-step and CB, respectively, differed substantially in their approach to treatment. Site visits and analysis of program schedules showed that 12-step programs spent treatment time mainly on 12-step activities (e.g., reading AA/Cocaine Anonymous (CA)/Narcotics Anonymous (NA) literature, studying the 12 steps, attending self-help group meetings), whereas CB programs spent treatment time mainly on activities such as cognitive restructuring counseling, behavioral skills training, and CB psychotherapy (Humphreys and Moos, 2001). Staff surveys found that 12-step program staff were much more likely than CB program staff to believe that addiction is a disease and to describe themselves as “in recovery from addiction” (Moos et al., 1999; Ouimette et al., 1997). Finally, patients in the 2 types of programs differed in the expected direction on their level of endorsement of items from a religious/spiritual program environment scale (Moos and Moos, 1998). These items included “Patients are encouraged to pray as part of recovery” (73.3% endorsement in 12%-step, 29.7% in CB), “There is little emphasis on religion and spirituality” (endorsed by 14.5% of 12-step patients vs 56.5% of CB), and “Patients rarely read the Bible or talk to the chaplain” (35.0% endorsement in 12%-step, 57.5% in CB).
PATIENTS
As described in the 1-year analysis of this sample (Humphreys and Moos, 2001), the study included patients who provided informed consent at intake and were followed up 1 year later in a larger evaluation of VA treatment outcomes nationally (Moos et al., 1999). The sample analyzed here is a subsample of all enrollees in the larger study, namely 887 patients entering 12-step programs and 887 patients entering CB programs who were matched on their history of mental health utilization.
All patients were low-income substance-dependent male veterans. At intake, about one-fourth (24.7%) were employed and one-fifth (19.5%) were married. A total of 20.4% of patients had a comorbid Axis One psychiatric disorder. In the year before intake, the average patient utilized mental health services costing a total of $3,313 (in 2006 dollars). Extensive data analysis showed that patients in 12-step and CB programs did not differ at treatment intake on these variables or on any of the clinical, utilization, or cost outcomes used in this study (Humphreys and Moos, 2001).
PROCEDURE
On-site research assistants independent of the clinical staff described the study to treatment-seeking male veterans at intake. Consenting patients completed a self-administered survey at baseline, 1-year, and 2-year follow-up. The data in the inventory were supplemented with health care utilization data drawn from VA's national databases.
MEASURES
Four dichotomous clinical outcomes were assessed at each contact. The measures tapping substance use referred to the past 3 months and assessed complete abstinence from drugs and alcohol and lack of substance abuse-related problems. The latter variable was coded positively if patients answered “never” to a series of 15 items asking how frequently substance use had caused problems in a range of domains, including work, financial, legal, and family. Abstinent participants were still asked to complete the list of substance abuse-related problems (and frequently reported such problems) because many problems initiated by substance abuse can persist after an individual has ceased substance use (e.g., liver disease, marital strain, unemployment). The measures assessing psychiatric problems were derived from the Brief Symptom Index (BSI, Derogatis, 1993), which asks respondents to rate how much discomfort they have experienced from various symptoms (response options are “not at all,” “a little bit,” “moderately,” “quite a bit,” and “extremely”). Freedom from significant psychological distress was coded positively if patients rated their amount of discomfort as no higher than “moderately” on 8 or more of 12 items from the BSI Anxiety and Depression subscales, whereas freedom from significant psychiatric problems was coded positively if the patient responded in this fashion to 7 or more of 10 items from the BSI Psychoticism and Paranoid Ideation subscales. These cutting scores on the BSI accurately distinguish VA substance use disorder patients who do versus do not have severe comorbid psychopathology (Moos et al., 2000).
Affiliation with 12-step self-help groups was measured using 2 items, which assessed affiliation with AA, CA, and NA in the past 3 months. These were frequency of group attendance (response options ranged from 0 = “none” to 4 = “30 or more meetings”) and talking with one's sponsor (response options ranged from 0 = “never” to 4 = “several times a week”).
MENTAL HEALTH SERVICE UTILIZATION AND COSTS
The national VA database captures all treatment encounters system wide. This database was used to calculate the number of mental health outpatient visits and inpatient days for each patient for the period being examined here (i.e., from 1 to 2 years posttreatment). Mental health treatment was defined as that provided for patients' substance use disorder and any psychiatric comorbidities. Costs were calculated in 2006 dollars using VA budgets at $85 per visit for outpatient care and $750 per day for inpatient care.
RESULTS
TWO-YEAR FOLLOW-UP RATES
The matched sample of patients in each program had all been followed up at 1 year (Humphreys and Moos, 2001). Of these individuals, 1,528 (86.1%) were followed up again at 2 years and thus reported on the clinical outcomes and mutual help group affiliation indices examined here. The follow-up rate was slightly higher for patients treated in CB (88.4%) than in 12-step programs (83.9%), χ2 = 7.55, p = 0.006. Because VA health care data are available on all patients, the follow-up rate for the cost and utilization outcomes is 100% (i.e., all 1,774 participants).
CLINICAL OUTCOMES
Chi-square analyses were used to examine differences between treatments on the substance use and psychiatric outcomes (see Table 1). As was found at 1-year follow-up (Humphreys and Moos, 2001), the outcomes did not differ substantially, except for the abstinence rate, which was one-third higher among 12-step treatment patients than among CB patients (p < .001). To test whether these results could be attributable to loss of patients at follow-up or the slightly higher rate of follow-up in the CB programs, we reran the analysis, assuming that all nonlocated patients had poor outcomes. This analysis also found no difference on any outcomes, except for abstinence, which was significantly higher for patients in the 12-step programs (results not shown).
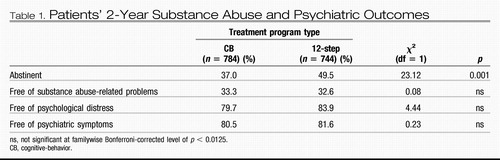 |
Table 1. Patients' 2-Year Substance Abuse and Psychiatric Outcomes
TWELVE-STEP SELF-HELP GROUP AFFILIATION
As had been the case at 1-year follow-up (Humphreys and Moos, 2001), patients treated in 12-step programs had significantly higher rates of self-help group involvement at 2-year follow-up. Independent sample t-tests showed that this held true both for frequency of attending group meetings (M = 1.28 in 12-step, M = 0.89 in CB, t = 5.46, p < 0.000) and of talking with a sponsor (M = 0.82 in 12-step, M = 0.46 in CB, t = 5.84, p < 0.000). In practical terms, these numbers reflect that among 12-step treatment patients, the rate of attending 10 or self-help group meetings in the past 3 months was about 50% greater (36.0% vs 23.6% in CB) and the rate of talking to a sponsor once or twice a month or more was almost 100% greater (24.7% in 12-step vs 13.6% in CB).
MENTAL HEALTH TREATMENT UTILIZATION AND COST
Independent sample t-tests showed that from 1-year to 2-year follow-up, patients treated in 12-step programs had fewer inpatient days (M = 7.2 vs 10.2 in CB, t = 2.56, p = 0.011) and outpatient visits (M = 6.6 vs 9.8 in CB, t = 2.28, p = 0.023). This translates to about 30% lower average per-patient costs in the 12-step condition ($5,638) than in the CB condition ($8,078, t = 2.50, p = 0.01).
Relative to the differences found at 1-year follow-up (Humphreys and Moos, 2001), the above difference in cost is smaller in proportion (30 vs 40% at 1 year) and in size ($2,440 per patient vs $5,735 at 1 year).1 Yet, it is still in absolute terms a sizable practical difference in cost, and by persisting even to a lesser extent into the second year after inpatient treatment, the offset identified here magnifies the size of the overall offset across the entire 2-year period (a total of $8,175 per patient lower cost after 12-step treatment).
DISCUSSION
This quasi-experimental evaluation of patients entering two distinct forms of addiction treatment showed that the pattern of findings at 1 year largely persisted at 2 years. Both 12-step and CB program patients experienced substantial and comparable improvements in substance-related problems and psychiatric outcomes and required less ongoing professional treatment between 1 and 2 years than they had in the year after discharge. However, patients treated in 12-step treatment programs achieved substantially better abstinence rates (49.5 vs 37.5% in CB). This difference is actually slightly larger than that identified at 1-year follow-up (45.7% in 12-step vs 36.2% in CB, Humphreys and Moos, 2001).
Group differences in help-seeking patterns were also similar to those found at 1 year. Not surprisingly, given the strong evidence 12-step treatment programs place on 12-step ideas and self-help group attendance, their patients attend meetings and talk to sponsors at substantially higher rates than do CB patients even 2 years after treatment. Although the size of the difference diminishes somewhat from the 1-year to the 2-year follow-up, 12-step patients also continue to use relatively less professional mental health services, increasing the savings associated with 12-step treatment over 2 years to an average of more than $8,000 per patient, in a sample of patients who had comparable mental health care utilization patterns before treatment. Because this figure does not include assessments of how the greater abstinence rate of 12-step patients may have reduced medical costs other than mental health services, increased employment rates, and lowered criminal justice costs, it likely represents a conservative estimate of the total savings to society produced by the active facilitation of posttreatment mutual help group involvement.
As mentioned, this study was not a randomized trial. Patients in each condition were not different at baseline on any measured variable, but this does not rule out the possibility that they differed on an unmeasured variable as would be ruled out (at least theoretically) in a randomized design. Our confidence in our results is therefore bolstered by the fact that randomized studies have also found that facilitation of 12-step mutual help group involvement promotes better outcomes (e.g., Timko et al., 2006), and that peer support approaches reduce health care costs of patients with addictive and psychiatric disorders (e.g., Galanter et al., 1987; Gordon et al., 1979). Results such as those of this study suggesting a substantial improvement in outcomes that saves rather than costs money are welcome, even exciting, but we wish to make the following cautions against their overinterpretation.
First, the study must be understood in light of the impressive size of 12-step mutual help organizations in the United States. An addicted person can find an AA or NA meeting in virtually any city or town in the United States and at most hours of the day, which makes it more likely that 12-step treatment staff's efforts to promote group involvement will succeed. The causal chain analysis that we have conducted with this sample shows that this increased rate of 12-step mutual help involvement mediates the superior abstinence rate found after 12-step treatment versus CB treatment (Humphreys et al., 1999). This does not mean that CB programs should convert to being 12-step oriented, but rather that they should either consider developing strategies for better linking their patients to 12-step groups (many emphases in CB programs have parallels in 12-step approaches; see Finney et al., 1998) or starting CB-oriented self-help groups such as SMART Recovery, as are some treatment professionals in the United Kingdom. Because substance abuse patients are diverse, it would be incorrect to assume that all patients would have better outcomes and lower costs in 12-step than in other types of programs.
Second, it would be equally inaccurate to conclude from these results that because promoting self-help group involvement lowers the demand for continuing care, professional treatment services should be cut back and replaced with self-help groups. Every participant in this study received an intensive professional intervention, namely a 21-day to 28-day inpatient stay, and many afterwards received outpatient continuing care, which can work synergistically with posttreatment mutual help group involvement (Ouimette et al., 1998). Therefore, the study's results contrast substantial professional treatment plus varying amounts of self-help group participation, rather than self-help groups only versus professional services only. As mentioned, the Walsh et al. (1991) randomized trial indicates that inpatient treatment plus AA cannot be replaced by AA alone, as alcohol-abusing individuals in the former condition are less prone to relapse over time.
If the above would be the wrong conclusions, what would be the right ones? First, the national emphasis being placed by certain agencies (e.g., the Substance Abuse and Mental Health Services Administration) on “recovery support services,” including self-help groups, is probably a cost-effective investment. Certain tasks supportive of recovery, such as providing encouragement, social activities, friendship, monitoring, and spiritual support, can probably be accomplished by peer-based services as well as they can by health care professionals, and at greatly reduced costs. This has a 2-fold benefit: greater likelihood of long-term recovery for the addicted individual and greater targeting of scarce professional resources to those patients who require such assistance.
In our experience, making the case that treatment programs should prioritize self-help group involvement can be difficult because many treatment providers believe they “do this already”; indeed, that every program does. In practice, however, what this often means is that at some point during treatment a counselor gives the patient a list of local self-help groups and suggests that the patient attend a meeting, which is a minimally effective clinical practice (Sisson and Mallams, 1981). We therefore encourage treatment providers to use the more intensive methods of promoting self-help group involvement empirically demonstrated to be effective (see, e.g., McCrady et al., 1999; Sisson and Mallams, 1981). The present study and a large number of other research projects (see Humphreys, 2004, for a review) indicate that such efforts will maximize the maintenance of treatment gains. Even if the added costs of actively facilitating self-help group involvement cost several hundred dollars per patient, the results here indicate that such an investment would be an excellent use of fiscal resources.
In a time of reduced resources for addiction treatment in the United States, clinicians feel understandably stressed in their efforts to provide high-quality care under budget constraints. There is no magic bullet for this difficult situation, but the results presented here indicate that actively promoting self-help group involvement is a useful method for extending the benefits of treatment while lowering its ongoing cost.
Derogatis L (1993) Brief Symptom Inventory Administration, Scoring and Procedures Manual, 3rd ed. National Computer Systems, Minneapolis, MN.Google Scholar
Finney JW, Noyes C, Coutts A, Moos R (1998) Evaluating substance abuse treatment process models: I. Changes on proximal outcome variables during 12-step and cognitive-behavioral treatment. J Stud Alcohol 59: 371– 380.Crossref, Google Scholar
Galanter M, Castaneda R, Salamon I (1987) Institutional self-help therapy for alcoholism: clinical outcomes. Alcohol Clin Exp Res 11: 424– 429.Crossref, Google Scholar
Gordon RE, Edmunson E, Bedell J, Goldstein N (1979) Reducing rehospitalization of state mental patients: peer management and support. J Florida Med Assoc 65: 927– 933.Google Scholar
Humphreys K (2004) Circles of Recovery: Self-Help Organizations for Addictions. Cambridge University Press, Cambridge, UK.Google Scholar
Humphreys K, Dearmin Huebsch P, Moos RH, Finney JW (1999) A comparative evaluation of substance abuse treatment: V. Treatment can enhance the effectiveness of self-help groups. Alcohol Clin Exp Res 23: 558– 563.Crossref, Google Scholar
Humphreys K, Moos RH (1996) Reduced substance abuse-related health care costs among voluntary participants in Alcoholics Anonymous. Psychiatr Serv 47: 709– 713.Crossref, Google Scholar
Humphreys K, Moos RH (2001) Can encouraging substance abuse inpatients to participate in self-help groups reduce demand for health care?: a quasi-experimental study. Alcohol Clin Exp Res 25: 711– 716.Crossref, Google Scholar
Humphreys K, Phibbs CS, Moos RH (1996) Addressing self-selection effects in evaluations of mutual help groups and professional mental health services: an introduction to two-stage sample selection models. Eval Program Plann 19: 301– 308.Crossref, Google Scholar
Kennedy M (1989). Psychiatric hospitalization of Growers. Paper presented at the Second Biennial Conference of Community Research and Action, E. Lansing, MI.Google Scholar
McCrady BS, Epstein EE, Hirsch LS (1999) Maintaining change after conjoint behavioral alcohol treatment for men: outcomes at six months. Addiction 94: 1381– 1396.Crossref, Google Scholar
Moos RH, Finney JW, Moos BS (2000) Inpatient substance abuse care and the outcome of subsequent community residential and outpatient care. Addiction 95: 833– 846.Crossref, Google Scholar
Moos RH, Finney JW, Ouimette PC, Suchinsky RT (1999) A comparative evaluation of substance abuse treatment: treatment orientation, amount of care, and 1-year outcomes. Alcohol Clin Exp Res 23: 529– 536.Google Scholar
Moos RH, Moos B (1998) The staff workplace and the quality and outcome of substance abuse treatment. J Stud Alcohol 59: 43– 51.Crossref, Google Scholar
Ouimette PC, Finney JW, Moos RH (1997) Twelve step and cognitive-behavioral treatment for substance abuse: a comparison of effectiveness. J Consult Clin Psychol 65: 230– 240.Crossref, Google Scholar
Ouimette PC, Moos RH, Finney JW (1998) Influence of outpatient treatment and 12-step group involvement on one-year substance abuse treatment outcomes. J Stud Alcohol 59: 513– 522.Crossref, Google Scholar
Roberts LJ, Salem D, Rappaport J, Toro PA, Luke DA, Seidman E (1999) Giving and receiving help: interpersonal transactions in mutual-help meetings and psychosocial adjustment of members. Am J Commun Psychol 27: 841– 868.Crossref, Google Scholar
Sisson RW, Mallams JH (1981) The use of systematic encouragement and community access procedures to increase attendance at Alcoholics Anonymous and Al-Anon meetings. Am J Drug Alcohol Abuse 8: 371– 376.Crossref, Google Scholar
Timko C, DeBenedetti A, Billow R (2006) Intensive referral to 12-step self-help groups and 6-month substance use disorder outcomes. Addiction 101: 678– 688.Crossref, Google Scholar
Walsh D, Hingson R, Merrigan D, Levenson S, Cupples L, Heeren T, Coffman G, Becker C, Barker T, Hamilton S, McGuire T, Kelly C (1991) A randomized trial of treatment options for alcohol-abusing workers. New Engl J Med 325: 775– 782.Crossref, Google Scholar



